Introduction
Through the Sustainable Development Goals, aided by the encouraging outcomes of the Millennium Development Goals, the international community has boldly aimed to end the tuberculosis (TB) epidemic by 20301,2. The Millennium Development Goals have seen TB prevention, diagnosis and treatment interventions save approximately 37 million lives worldwide between the years 2000 and 20133. Treatment success rates have been reported at or above 85% since 20071. In most countries in the Western Pacific region, the reported TB prevalence has decreased by 50% and the mortality rate reduced by more than 70%4.
Despite these reported advances, TB remains a problem in Solomon Islands. In 2015, the new case rate for TB in Solomon Islands was estimated at 66/100 000, with an incidence of 89/100 000 (including new and relapsed cases) and a fatality rate of 9.8/100 0005. The Solomon Islands population is geographically dispersed across over 900 islands with approximately 80% of the community living in rural or remote areas6. In Solomon Islands, limited healthcare resources, geography and sociocultural beliefs contribute to low detection rates and delayed treatment, facilitating the continued spread of the disease, particularly in remote provinces. The two principal sociocultural beliefs that have been identified as hindering the treatment of TB Solomon Islands revolve around the challenge of translating the concept of TB into local language and the challenge to have patients continue to take medication when they feel well. These beliefs mean there is a reduced rate of people presenting for treatment in hospital and a likely low level of compliance with completing the full course of prescribed TB treatment7.
The health system in Solomon Islands comprises the National Referral Hospital (NRH) in Honiara, supported by a network of seven provincial hospitals (staffed by just one to three doctors) and small community clinics and aide posts occupied by either registered or enrolled nurses8. The medical workforce is predominantly based at the NRH where over 70% of doctors and the entire specialist medical workforce for the nation are employed8.
For most suspected TB cases in Solomon Islands there is no access to laboratory confirmation of the diagnosis9. In resource-poor countries, there exists great difficulty obtaining accurate clinical data that reflects the community as a whole10. This is true in Solomon Islands where the ability to measure clinical outcomes outside of the NRH is particularly limited.
This clinical audit on TB management in a remote provincial hospital setting was performed to gain baseline information regarding the current state of TB diagnosis and hospital-based care in an indicative remote province in Solomon Islands. The published data on currently achieved health outcomes can be inaccurate. A recently published study has documented that the current perinatal mortality rate in Kirakira Hospital (KKH) is more than double what is reported by the WHO as it monitors the progress of the Millennium and Sustainable Development Goals11. The desired outcome of the audit was to provide data from which future clinical quality improvement implementation projects might be performed to assist the people of Makira-Ulawa to not be left behind the global community’s quest to achieve the goal of eradicating TB by 2030.
Context
Kirakira is the provincial capital of Makira-Ulawa Province in Solomon Islands. It is a small town of approximately 3500 people and is located 200 km south-west of Honiara12. It is accessible by air and boat. The provincial population was measured at 40 000 in 200913. KKH is the provincial hospital and main healthcare facility of Makira-Ulawa Province. The main Island of Makira is 100 km long and 40 km wide. A steep mountain range runs along the spine of the island, which rises to 400 m above sea level. The terrain is thick jungle.
The one gravel road along the northern coast line runs for 40 kilometres. Public transport consists of a small flat-top truck that runs back and forth along the gravel road. People often must walk long distances to get to the road so they can catch the flat-top truck. About a dozen people can fit on the back of the truck at any one time. People can climb aboard to get a lift to Kirakira. Kirakira sits in the middle of the one road of Makira-Ulawa Province.
To access KKH, patients on the coastline will travel by boat, which is usually a small open vessel with an outboard motor. Those living inland will often walk for 1–2 days through the jungle before catching the truck into Kirakira in order to visit the hospital. The financial cost of transport is very expensive in terms of time and money for the people in Kirakira and it is an impediment to being able to seek care, and makes coordinated follow-up of cases like TB very difficult.
Bacillus Calmette–Guérin (BCG) vaccination is included as part of the immunisation schedule in Solomon Islands. In 2017 the estimated coverage for BCG was 79% according to WHO and UNICEF estimates14. BCG testing is not available in Makira-Ulawa Province.
The provincial health service is staffed by 2 doctors and 60 nurses. Approximately half of the nurse workforce is stationed at smaller rural health clinics and nurse aid stations across the province8. The hospital is a 40-bed facility that includes an emergency department, male and female wards, a children’s ward, a maternity unit and an isolation ward where TB patients are admitted. The KKH health service employs a registered nurse who has responsibility for the management of suspected TB patients in the province. Up to 2017, the diagnosis of TB was made based on clinical suspicion confirmed on X-ray or based on the patient living in the same house as the index patient. In KKH there are two rooms, one male and one female, for the treatment of adult patients with a diagnosis of TB in the hospital. The children are managed in a back room of the children’s ward and ideally there are no children alongside them without TB. This part of the children’s ward is adjacent to the two TB treatment rooms. The separation of the affected children is the best that can be achieved with the facilities available.
The immediate household contacts and the children of the index case are also admitted for treatment. It is amongst this group of patients that there was a very low level of clinical documentation. It is likely that most of the cases recorded by the TB nurse for whom there were no recorded admissions came from this group of patients.
KKH does not have the capacity to perform standard microbiological facilities to allow for bacteriological assessment for infection. There is no capacity to perform blood, urine, cerebrospinal fluid or skin cultures (Mantoux testing). The only pathology tests that can be performed include a full blood count, blood glucose level, urine microscopy, thick and thin film analysis for malaria, serology for hepatitis, syphilis and HIV and blood group cross-matching. Extrapulmonary TB can be diagnosed radiographically (if there is X-ray film in stock) for suspected osteomyelitis. Meningitis is solely a clinical diagnosis in KKH.
Up until April 2015 there was the capacity to confirm a suspected diagnosis of TB in KKH using a Zeil-Nielsen stain that could confirm the presence of acid-fast bacilli. Due to lack of resources, personnel and equipment becoming unserviceable, there was no capacity to perform sputum testing again until 2017. From August 2017 the capacity to perform sputum smears for acid-fast bacilli was restored. In the next 12 months there were 26 positive smears identified from 69 patients who were tested for TB because of clinical suspicion. It is hoped that KKH will have an operational GeneXpert test to allow for the detection of multi-drug resistant TB (MDR-TB) by 2019.
There are no other microbiological or DNA diagnostic capabilities available in Kirakira.
TB treatment in Makira-Ulawa Province follows the WHO guidelines15. The intensive phase consists of combination therapy with four drugs: isoniazid, rifampicin, pyrazinamide and ethambutol (HRZE), administered by directly observed therapy whilst the person is an inpatient in the TB ward of KKH for a period of 8 weeks. Patients are then discharged home and required to take a further 4 months of maintenance treatment with isoniazid and rifampicin (HR). The TB nurse follows up the care of these patients in the community supported by the nurses based at the various rural and area health centres to help ensure compliance with treatment. Directly observed taking of medication for the maintenance treatment of TB is not part of the current management practice of TB in Makira-Ulawa Province. Previously, the names of all patients managed by the TB nurse were recorded in an exercise book that was used to help coordinate follow-up and monitoring of these patients.
The families admitted for TB (or close household exposure with TB) are required to live in the TB rooms in the hospital for the duration of their intensive phase treatment. This is done as a quarantine procedure to prevent the spread of disease. Another benefit of this procedure is that patients are compliant with their medication while in hospital. Following admission to hospital, there is little daily medical input involved in the care of these patients, who are predominantly fully independent with all their personal cares whilst in hospital.
In Solomon Islands all individuals carry with them a small exercise book, which is their own personal medical record. It contains the written notes made by each of the nurses and medical staff that have seen the patient. These notebooks are invaluable resources when clinicians are seeing an individual patient and trying to work out the next stage of treatment they require. There are however, major limitations of the system. There are no formal records of clinical consultations retained by the health service. The fact that a patient has been seen is recorded, but there are no means to document or audit any of the clinical details or outcomes achieved to measure the effectiveness of any of the treatments. In Solomon Islands only 2% of deaths are registered, which makes it even more challenging to estimate what might be the real outcome for the patients being managed. These facts mean that claims of what the actual outcomes might be are unlikely to be supported by detailed clinical audits and remain very approximate estimates16.
Methods
The hospital files of patients identified as having TB treatment by the TB nurse over the 2-year period (between 2015 and 2017) were retrieved from the hospital medical records department. The files were then assessed by final-year medical students from Bond University as part of a 1-month clinical placement at KKH.
For the duration of the audit, a patient with a chronic cough and night sweats with associated abnormal X-ray findings was considered to have TB. The cough was considered chronic if it was recorded in the admission that the patient had daily symptoms of cough. If the admission record stated the presence of haemoptysis, fever of any kind and weight loss the symptom was regarded as present. There was no data to indicate the frequency or volume of coughing up blood, how high the fever was or how much weight had been lost.
Ethics approval
The study was approved by Bond University Human Research Ethics BUREC 15097 and by the KKH Medical Administration committee.
Results
The results of the study are summarised in Table 1. From June 2015 to June 2017 there were 78 patients recorded as having TB by the TB nurse. Detailed inpatient clinical data were available for 54% (42 of 78) of TB patients. There was no documented reason for no available data recorded on the remaining 36 patients identified as having TB.
The most common presenting complaint for tuberculosis identified by the audit was chronic cough (90%), followed by fever (59%). At KKH, chest X-rays were performed in 83% (35 of 42) of patients with suspected TB. There is only one radiographer based at KKH. If the radiographer is on leave during this time, patients are admitted to the ward without performing an X-ray. Eighty-six percent (36 of 42) of patients complied with completing the full 8-week admission to hospital. Only 14% (6 of 42) of patients did not comply and were admitted for 4 weeks or less. The average length of stay for each patient was 51 days. The average number of patients on the TB ward for whom data were collected was 3.8 on any given day during the 2-year period.
In Solomon Islands it is estimated that each admission to hospital for TB costs US$592517. This should not be surprising given the average length of stay identified by this audit was 51 days at KKH. Thus, with approximately 39 cases per annum being managed by the TB nurse, US$231,000 is being spent on the management of TB at KKH each year. This equates to 15% of the available healthcare resources in Makira-Ulawa Province being allocated for the treatment of TB18.
Table 1: Summary of medical records of tuberculosis patients admitted to isolation ward of Kirakira Hospital, July 2015 – July 2017.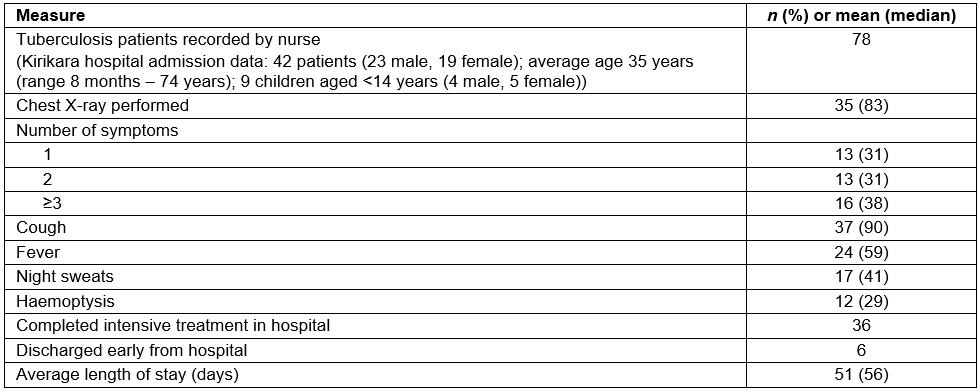
Discussion
This audit provides a snapshot of the current care and clinical practice with respect to the management of TB in Makira-Ulawa Province between July 2015 and July 2017. It confirms that the treatment of TB consumes a significant portion of the scarce resources available for health care at KKH and within the Makira-Ulawa Province of Solomon Islands19. A total of 15% of the budget allocated for all health care for Makira-Ulawa Province in 2017 (including KKH and all outreach stations) of US$1.5 million is spent on the inpatient treatment of TB patients in KKH.
There are many limitations to this audit. Written data were available on only 42 of 78 patients. There is no microbiological confirmation of TB, and the outcome of any of the cases and how often patients completed the full course of TB treatment are unknown. The written documentation on each patient is limited. There are new cases and recurrent cases included in this audit. It was not possible to identify which was which. It is not possible to make any estimate of the incidence and prevalence of TB in the community or to measure the effectiveness of current treatment protocols.
The quantitative data in this study has limitations: almost 50% attrition, lack of follow-up and no information about patient adherence beyond 2 months. Unless these data are reported, the reality of the limitations that confront clinical practitioners in resource-poor communities around the world will continue to go unnoticed. The concern is that the reported WHO statistics, with calculations based on estimates often made at a distance from their subject, that currently measure improvements in progress towards meeting the Millennium Goals, are accepted as accurate; the real data that this audit presents suggests that is most likely not the case. The global community might believe we are closer to eradicating problems such as TB in the Pacific than what is happening where 80% of the population of Solomon Islands live.
The population of Makira-Ulawa Province at the last census in 2009 was recorded as 40 90011. This means that if the KKH TB nurse is recording all cases of treatable TB in Makira-Ulawa Province, then the current estimated incidence (consisting of new and recurrent cases each year) of TB) identified in this audit is 97 cases per 100 000. This statistic is just above the 2017 WHO estimated range of new and recurrent cases of TB in Solomon Islands of 76 (range 58–96)18. The population is very dispersed in extremely remote communities across Makira-Ulawa Province. It is difficult to imagine that all known cases of TB have been identified by the single coordinating nurse. Given the recent experience of seeing many Laboratory confirmed cases in the time since the capacity to perform sputum analysis for acid-fast bacilli, it is most likely that the number of cases is indeed higher and that there is an ongoing epidemic of TB in this community.
There is no way of knowing if the patients who have been treated for TB really had TB and what happens to them on follow-up. In Solomon Islands the provincial health services do not carry a record of the clinical details of outpatient consultations. Instead, patients have their own personal medical record book. It is a valuable resource that certainly provides much-needed data to guide clinical interactions; however, there is no system to allow the health service to collect clinical data about these patient encounters. Therefore, the clinical outcomes achieved through outpatient follow-up are unknown in the Makira-Ulawa Province in Solomon Islands.
Data collection systems for hospital inpatients are also limited. There are three possible reasons that inpatient data was only available for 42 of 78 patients. First, the inpatient notes confirm that 100% of patients who received a formal medical admission had at least one clinical symptom of TB. No asymptomatic patients appeared to receive a formal medical admission for intensive treatment. This is despite many symptom-free community members being at high risk of contracting TB (eg having close household contacts). Second, there is the potential that several records might have been lost and unable to be found at the time of the audit. Third, the nurse may not have recorded patient details.
There exist readily available tools that would substantiate the diagnosis of TB at KKH and have been successfully utilised in other resource-poor settings around the world. The acid-fast bacilli test is one of the quickest and most cost-effective modes of diagnosis19. Until April 2015, acid-fast bacilli tests were performed at KKH. A combination of equipment maintenance, staff expertise and limited funding appears to be responsible for this loss of diagnostic capacity at KKH.
In the developing world, the WHO recommends the use of new diagnostic testing such as GeneXpert, a molecular test that can use a sputum sample to detect the DNA in TB bacteria and determine if the strain is likely to be MDR-TB and provide a result in less than 2 hours20. Whilst economical by Western standards, the high cost of diagnostic equipment, at US$17,000 (an individual test costs US$9.98), and the need for staff training and equipment maintenance mean such an investment in resources has been unattainable at KKH20. This is not surprising when the total budget for health care in Makira-Ulawa Province is just US$30 per person per annum for all primary and secondary hospital health services17. MDR-TB is an infection that causes significant concern to public health physicians around the world. A growing reservoir of partially treated and new cases of TB would certainly increase the risk of an outbreak of this infection in nearby wealthy countries like Australia and New Zealand. Not only is there an imperative to improve the management of TB in Makira-Ulawa Province for the sake of the local population, failing to appropriately manage this epidemic has the potential to cause far greater harm in the future to the entire regional population of Oceania.
The lack of current investment in the treatment of TB at KKH suggests that the gains achieved through the Millennium Development Goals may be at risk in the provinces of Solomon Islands. An almost 50% reduction in expenditure used for TB management between 2012 and 2016 is a concern21. Although Makira-Ulawa is a remote province, the reality is that there is a substantial risk of disease spread to adjacent countries given the relative ease of international travel in 2017. The problem of having inadequate resources to manage the TB epidemic is a global health problem where investments need to be made so that accurate identification, treatment and follow-up can be documented in rural communities, where so much of the population lives in the developing world.
The medical and nursing staff do their best in very challenging circumstances. They identify suspected cases of TB based on history, clinical symptoms and plain X-ray findings. They have achieved a commendably high rate of compliance, with 86% of patients remaining as inpatients and completing 8 weeks of observed treatment to ensure full compliance with the intensive phase of TB treatment. However, key weaknesses identified in this audit are the lack of any laboratory-based confirmation of TB diagnosis at the time of admission and the absence of data available on patients at the time of completion of their treatment.
Makira-Ulawa Province is the fourth largest of nine in Solomon Islands. The care provided in KKH is likely to be consistent with the care offered in other small and resource-poor hospitals across the Pacific. Publication of this data, despite its limitations, highlights that there is a current TB epidemic, and gives voice to isolated communities so they can access the resources required to meet the challenge of eliminating TB.
Conclusion
This audit confirms that the diagnosis and treatment of TB remain a common problem that is encountered at KKH in Makira-Ulawa Province in Solomon Islands. The audit highlights that despite TB’s apparent prevalence there is a great deal of uncertainty about the diagnosis of TB in KKH and there exists no effective means of being able to be confidently reassured that affected people have been successfully cured of the disease. This report should serve as a wake-up call to those who may feel reassured at the reported progress achieved in the era of Millennium Goals. Just as we have seen recently with malaria rates of detection increasing, TB remains a major threat to the global community22. There needs to be comprehensive support provided to allow for accurate data collection systems, equipment and staff training if the goal of eradicating TB from Makira-Ulawa Province is to be achieved by 2030.
References
You might also be interested in:
2019 - Social and community networks influence dietary attitudes in regional New South Wales, Australia






