Introduction
Maternal and neonatal health are core focus areas in fragile and conflict-affected areas1. More than 30% of maternal deaths worldwide occur in such areas and more than half of these deaths occur in three countries: Nigeria, Democratic Republic of Congo (DRC)2 and Afghanistan3. Apart from having disparities in rates of maternal death between countries, there are also large disparities within countries and between women living in rural and urban areas4.
DRC has one of the highest maternal mortality ratios in the east and central African regions (846 maternal deaths per 100 000 live deaths), with huge disparities within the country; in some rural areas the rate is more than 1000 maternal deaths per 100 000 live births5,6. The proportion of deliveries occurring outside health facilities is estimated to be 20%7.
DRC has a long history of conflict and crisis. Ituri Province (the study setting) is mostly rural and is going through sustained sociopolitical crises and wars. From 1999 to 2003, Ituri experienced ethnic clashes resulting in the deaths of approximately 60 000 people, with displacement of hundreds of thousands of people and severe destruction of infrastructure. In December 2017, a new ethnic clash started in Djugu Territory, causing over 60 deaths and more than 100 000 displaced people. Thousands of buildings were burnt, including health facilities and schools, and disruption of harvest resulted in severe food insecurity8,9. More recently, an Ebola outbreak has spread across DRC, including Ituri Province. Violence and civil unrest have hampered efforts to contain the disease.
Decades of political instability and wars since the early 1990s have resulted in the health system in DRC being severely underfunded. User fees are the main source of financing service delivery. There is a severe shortage of qualified skilled birth attendants, with only 1.05 physicians, nurses and midwives per 1000 population in 2012, compared to the Sustainable Development Goals index threshold of 4.45 per 1000 population10,11. The shortage of midwives is particularly striking: 0.06 midwives per 1000 population in 201512, and especially in rural areas5,12-15. As a consequence, there is low uptake of health services, including maternal health services5,16,17.
Midwives in DRC have a critical role in providing maternal health services: they are a bridge between the health system and community members in fragile, rural and underserved communities2. In DRC, midwives are deployed in different levels of care settings, from health centers to regional referral hospitals. Nurses are also considered skilled birth attendants in DRC. Their curriculum includes modules on midwifery allowing them to manage pregnancy and delivery12,18. However, there is very little evidence about midwives’ experiences working in this rural and fragile setting. Understanding what motivates midwives to train, stay in their roles or move to other employment, as well as the challenges they experience and the coping mechanisms they use, is essential in order to develop strategies to better support midwives so that they can continue to provide vital services, and at the same time attract midwives to work in these areas. This article explores the experiences of current and ex-midwives of their work through time, from initial choice of midwifery to future career aspiration in rural Ituri Province, north-eastern DRC19,20.
Methods
Design
A qualitative research design was used to enable exploration about experience, meaning and perspective in participants experiencing a phenomenon21, in this case midwives’ experiences and perceptions of their careers. Two qualitative methods were used. Life history (LH) interviews enabled midwives and ex-midwives to provide a detailed and chronological personal account using their own words of their life and career over time, from childhood up to the current day19,22. Focus group (FG) discussions brought midwives together, which supported group discussion of the challenges they face and coping strategies they have adopted23.
Setting
The research was carried out in Ituri, one of the 26 provinces of DRC, a large province located in north-eastern DRC with a population of 5 440 02124. It is approximately 1700 km from Kinshasa, the capital of DRC. Ituri is made up of five administrative territories and 36 health districts24. Ituri Province faces challenges in attracting and retaining midwives in rural districts, and has a very high maternal mortality ratio, far beyond the national average of 846 per 100 000 live births24,25. Within this province, three study districts were selected by the research team, in collaboration with the Provincial Health Division, based on rural and urban characteristics, as this provides a range of perceptions and experiences of midwives. The authors used the Provincial Health Division’s categorization of districts24 to select the three districts: the urban district, where the provincial capital is located (Bunia); a peri-urban district, where there is a concentration of people, with some facilities in remote areas (Aru); and a rural district, where all facilities are in rural and remote areas (Adja). In addition, the Pan African Institute of Community Health (IPASC), a faith-based organization where some of the authors work, organizes community health related interventions in the three health districts, and therefore the authors already understand the context and have relationships with the district health management, which facilitated access to these areas.
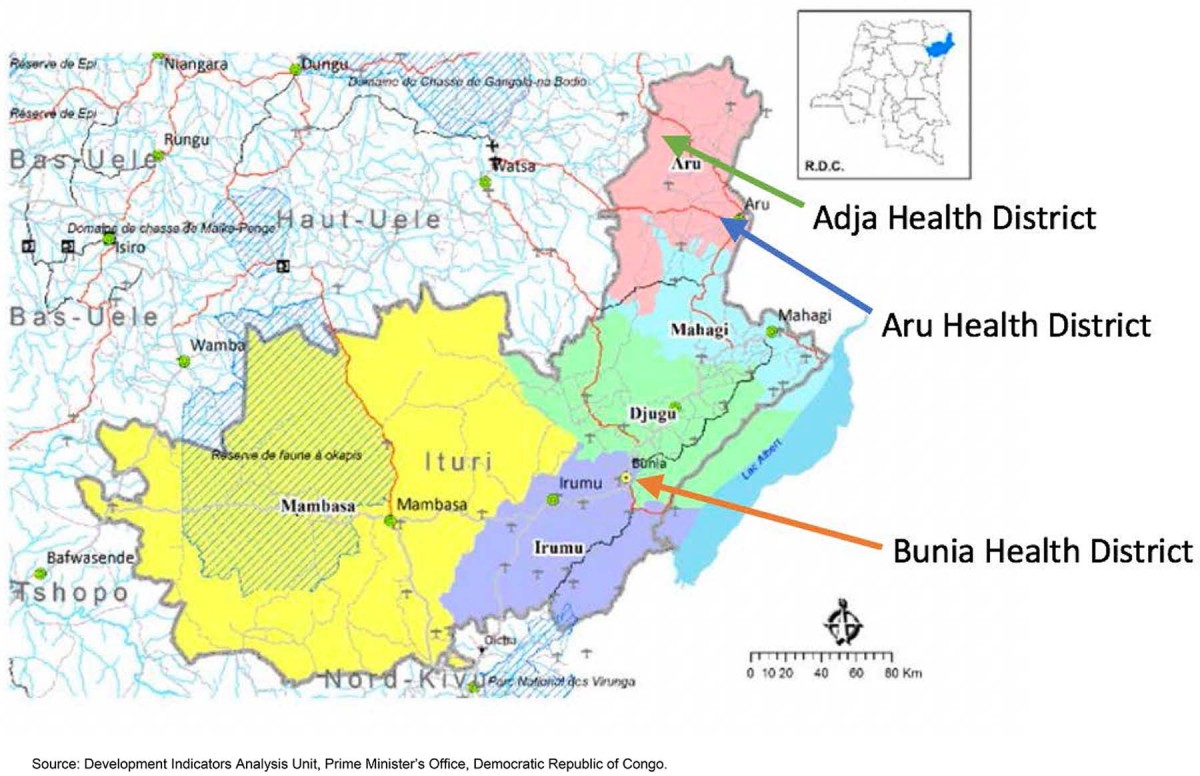 Figure 1: Ituri Province map with locations of the three study districts26.
Figure 1: Ituri Province map with locations of the three study districts26.
Recruitment and participants
Purposive sampling was used to recruit midwives in each of the districts Bunia and Aru. The purposive sampling technique is the deliberate choosing of participants on the basis of features or characteristics that will enable a detailed understanding of the topic. The researcher sets out to find people who can and are willing to provide the information by virtue of knowledge or experience27,28. Participants were selected using these criteria: sex (male and female), working or having worked in rural Ituri Province, place of work (health centers and hospitals), and current or previous employment as a midwife. Both midwives and ex-midwives were included in the LH interviews. The district health offices hold a list of the midwives working in the facilities in their district. The research team (AB, AP, MMN) visited facilities where they worked and identified potential participants using the criteria described above, and recruited them to the study. In Bunia and Aru, 10 midwives were recruited to the study. In rural Adja district, there are only six qualified midwives working and all were recruited. The snowball technique for sampling ex-midwives was used: the research team asked the midwives to identify ex-midwives in that area, and then the research team asked the ex-midwives to identify other ex-midwives. Six ex-midwives were recruited to the study. In Adja district, there were no ex-midwives, probably due to their migration from Adja to another district for employment. Current midwives who were selected for the life histories as described above were invited to participate in the FG discussions. In Adja, all six midwives participated, whereas in Aru and Bunia districts only eight in each district were available for the FG discussions. Study participants are described in Table 1.
Table 1: Characteristics of research participants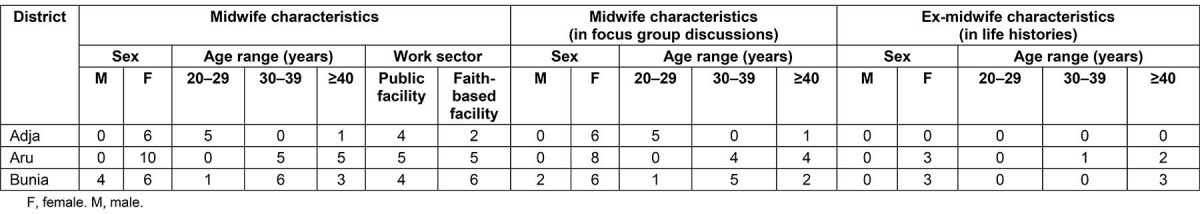
Data collection
Prior to data collection, two research assistants (male and female) were trained about the study. Data collection took place from January to May 2018. The topic guides were developed by the research team following a review of the literature on attraction and retention of midwives in rural areas. The LH topic guide covered how and why they became a midwife, description of their career path, their work experiences, career aspirations, and reasons for leaving (for ex-midwives). These were translated into French, being the language used in administration in DRC. LH interviews with midwives (n=26) and ex-midwives (n=6) were conducted by the research assistants (MMN, AP) and lead author (AB) in a place chosen by participants such as their homes or a private room in their workplaces.
Three FG discussions were conducted, one in each district, respectively with eight, eight and six participants. AB conducted the FG discussions in private rooms in the district health offices or IPASC office. A topic guide was used to facilitate the discussion, which focused on the challenges that participants faced working as midwives, strategies that supported their work, and possible solutions to these challenges. The research assistants were observers, responsible for recording and taking notes.
At the end of each FG discussion and LH interview, emerging themes were highlighted by the researcher and cross-checked with participants for accuracy. The recordings of the LH interviews and FG discussions were kept in a password-protected computer, transcribed verbatim, translated into English by an external translator from the Teaching College of Bunia and cross-checked by another external translator.
Data analysis
Data were analyzed using the thematic framework approach, which facilitates rigorous and transparent analysis29. It uses both deductive and inductive approaches29-31. A coding framework was developed based on the areas explored in the LH interviews and FG discussions, but also on themes emerging from the data such as insecurity in rural areas. This coding framework was applied to all transcripts, charts were developed for each theme, and these charts were used to describe the themes. NVivo v11 (http://www.qsrinternational.com/nvivo) was used to support the analysis.
Ethics approval
Ethics approval for this study was granted by the Liverpool School of Tropical Medicine (Research protocol 17-024) and the Multidisciplinary Research Centre for Development in Bunia, DRC (018/2017). A rigorous informed consent process was followed: all participants were given verbal and detailed written information about the nature and purpose of the research before taking part; participants were made aware of their right to decline to answer questions and were assured that measures were in place to anonymize responses. All participants gave written consent. All data were anonymized.
Results
The results are presented in three interlinked sections as described in Figure 2. The first section describes the journeys that midwives and ex-midwives made from childhood to the present day, using the narratives from the LH interviews. The second section presents the key challenges of their work and how these have been exacerbated by conflict and instability, using data from the FG discussions and LH interviews. These challenges have affected their journeys as midwives. To cope with these challenges, midwives have adopted a range of strategies, which are reported in the third section. Despite these strategies, some of these challenges remain.
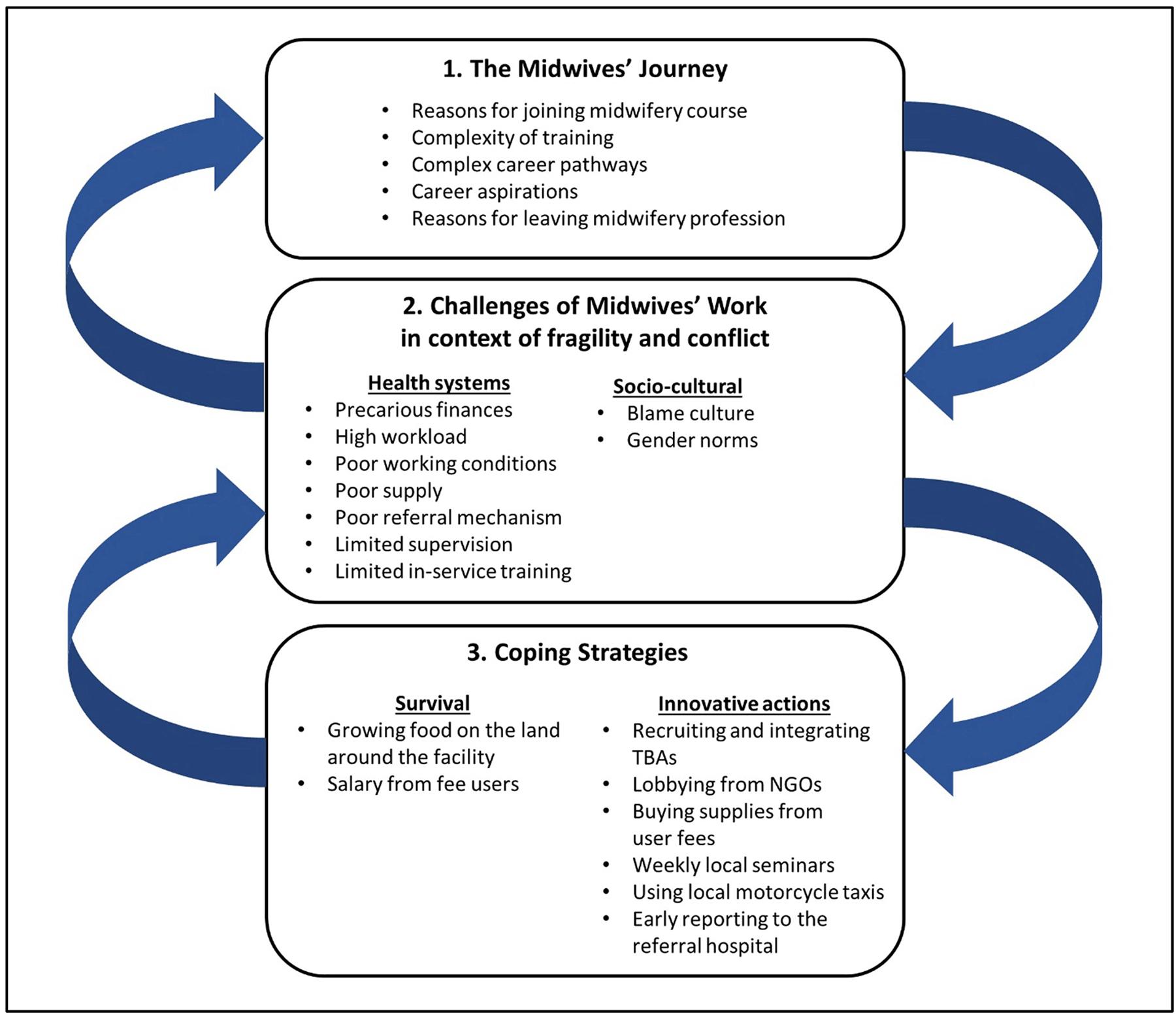 Figure 2: Overview of results: journeys, challenges and coping strategies.
Figure 2: Overview of results: journeys, challenges and coping strategies.
The midwives’ journey
Reasons for joining midwifery, midwifery training, job progression, career aspirations and reasons for leaving midwifery were explored in LH interviews with midwives and ex-midwives. The timeline for midwives is summarized in Figures 3 and 4.
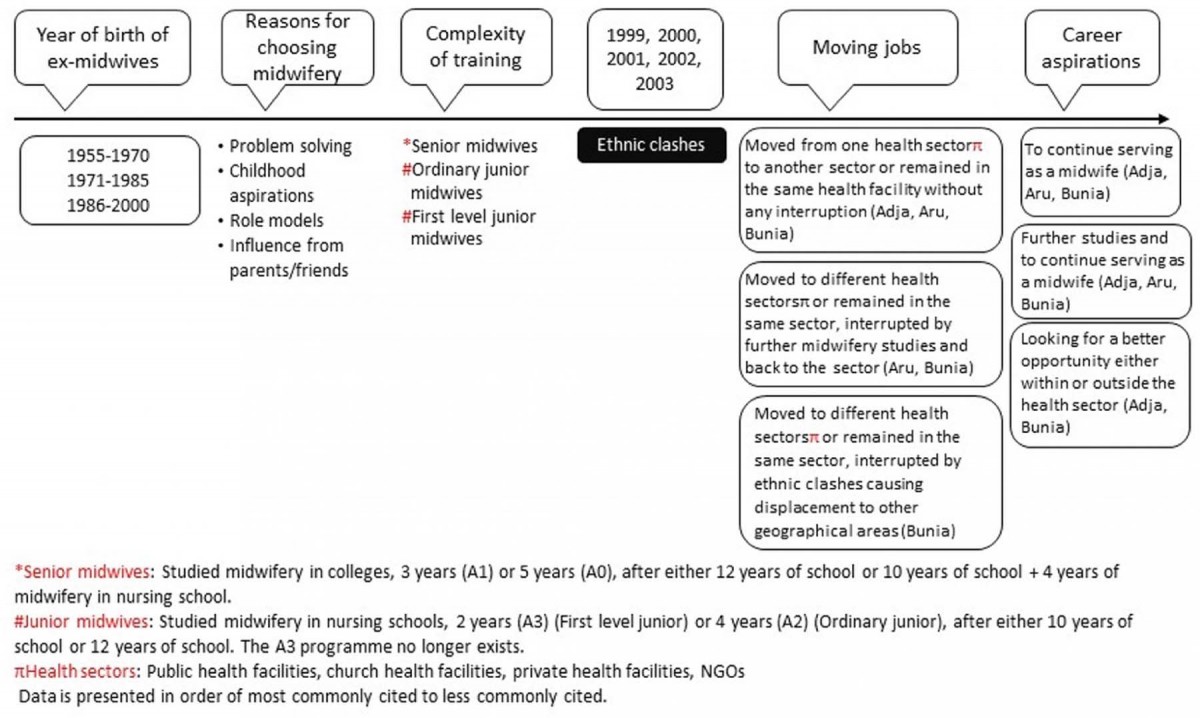 Figure 3: Timeline from life histories of working midwives.
Figure 3: Timeline from life histories of working midwives.
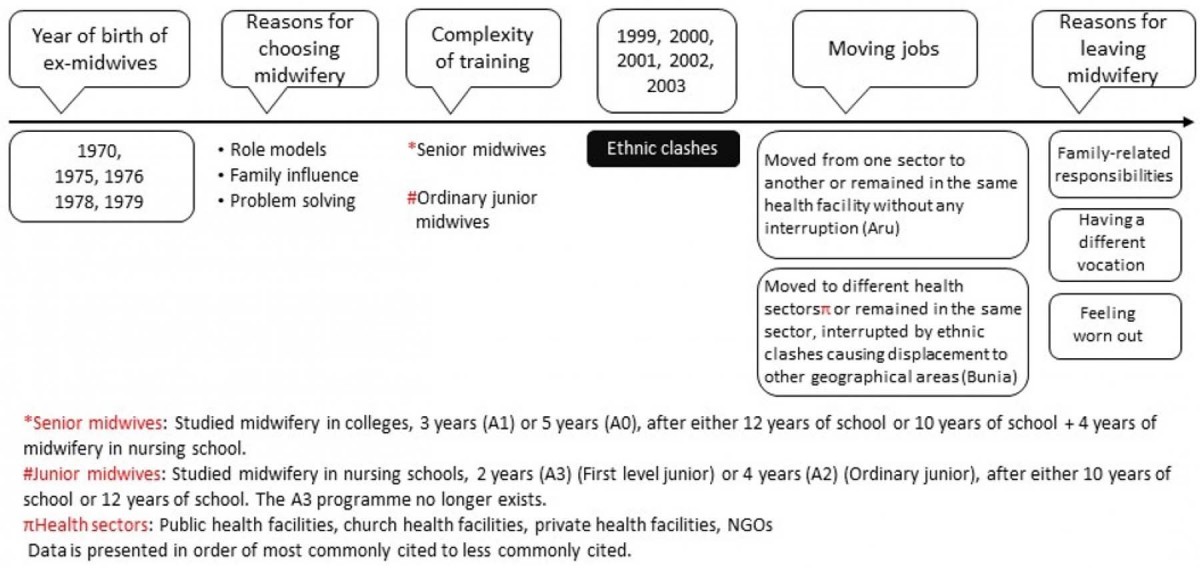 Figure 4: Timeline from life histories of ex-midwives.
Figure 4: Timeline from life histories of ex-midwives.
Reasons for joining midwifery: Midwives from Aru and Bunia districts mainly joined midwifery because they wanted to support women and solve health problems. However, those from rural Adja district said they joined because the midwifery profession had always been their aspiration since childhood: they wanted to be able to wear the uniform and help pregnant women during their pregnancy and delivery. They were motivated by practicing midwives, who they saw as role models.
I became a midwife because it has always been in my mind since my childhood. (Female midwife, 20–29 years, LH interview, Adja)
Many of the female midwives from the three districts described a role model as being the key motivating factor for becoming a midwife. The male midwives from Bunia district joined midwifery to be able to solve problems.
My aunt was a midwife, and seeing the way she was working and considered by women in the community, I was inspired and told her that I would like to become a midwife when I grow up. (Female midwife, ≥40 years, LH interview, Bunia)
Some female midwives joined midwifery due to personal experiences they went through, such as the death of a baby.
When I completed my secondary school, I decided to have a child, so I got pregnant and I had a child. Unfortunately, after 9 months the baby died. So, I decided to find the answer to that problem, and I needed to know myself as well. (Female midwife, ≥40 years, LH interview, Aru)
Parents and friends influenced some male and female midwives from Bunia district and ex-midwives from both Aru and Bunia districts to choose midwifery as a career.
… it was with the influence of friends that I had left the teaching, there were friends who came and wanted me to go for health sciences training. (Male midwife, 30–39 years, A1, LH interview, Bunia)
Complexity of midwifery training: A range of midwifery training courses in DRC have been adapted over the last decade, resulting in different levels and training experiences of midwives. ‘First level junior midwives’ have completed 10 years of school plus 2 years of midwifery (A3), ‘ordinary junior midwives’ have completed 10 years of school or 12 years of school plus 4 years of midwifery in nursing school (A2) and ‘senior midwives’ have completed junior midwifery plus 3 or 5 years at college) (A1 or A0). The first level junior midwifery program (A3) no longer exists.
While there were more senior midwives in the urban Bunia district, nearly all midwives in Aru and Adja districts were ordinary junior midwives. Two of the three nursing colleges (where midwifery training takes place) in Ituri Province are located in Bunia, so Bunia midwives can more easily access the colleges. The college in Aru only opened in 2010.
So, my parents sent me to Kisangani [a city located 750 km from Bunia] where I studied for 5 years, and completed my midwifery training in 2009. (Male midwife, 30–39 years, LH interview, Bunia)
Moving jobs: Most midwives from rural Adja and semi-urban Aru districts either moved from different sectors (eg from public facility to church facility) or remained in the same facility for many years. Most midwives in Bunia district started working as midwives in their rural native districts. Conflict broke out in these areas during the period of 1999–2004, and their homes and health facilities were looted and burned. They made their own way to Bunia district where it was seen as being safer, and where they have remained to this day.
… there was war around Jiba, this ethnic war in 1999, I had to leave Jiba. (Male midwife, ≥40 years, LH interview, Bunia)
Those midwives who were working in church facilities in the rural conflict-affected areas were supported in their move to Bunia district by the Church Medical Coordination Office, as described by this midwife.
I was affected at Drodro hospital [a Catholic health facility] where I worked for 3 years as a midwife. Then, the ethnic war started in 1999, we first fled to Bunia where I was transferred to work at Muzi Maria Health Centre [a Catholic health facility]. (Female midwife, ≥40 years, LH interview, Bunia)
Some midwives from Aru district and many from Bunia district, who had been working as ‘ordinary junior midwives’ for several years, went for further midwifery studies in nursing colleges in Bunia or Aru, and then rejoined the service. Ex-midwives from Aru and Bunia districts worked for 3 to 10 years in either the same facility or in health facilities belonging to different sectors. All ex-midwives in Bunia district originated from rural districts affected by ethnic clashes, which brought about their migration to Bunia district.
… when I was in Mongbwalu, I worked at the Mongbwalu Referral Hospital … During the events Ituri went through [ethnic clashes], we had to leave Mongbwalu [80 km north of Bunia]; we fled to Bunia, as displaced people, my husband and our two boys. (Female ex-midwife, ≥40 years, LH interview, Bunia)
Career aspirations: Most midwives in all three districts would like to continue serving as midwives and provide vital services to their communities.
My aspiration is to continue working as midwife and helping women in relation to their pregnancy and delivery and health. (Male midwife, ≥40 years, LH interview, Bunia)
Midwives reported that it is difficult to change profession as they get older.
I am very old to have career aspirations. But, I will keep on working as a midwife until my last breath. (Female midwife, ≥40 years, LH interview, Bunia)
Most midwives in the three districts who would like to go for further studies and come back to serve as midwives are ordinary junior midwives and are aged less than 35 years. They reported that study helps them service the people better and increases opportunities for promotion and being recruited to organizations where they provide better salary.
I would like to continue with my studies at the college in midwifery and then come back to help women. (Female midwife, 20–29 years, LH interview, Adja)
Some male midwives from Bunia district did not want to continue working as midwives and were looking for better opportunities outside the health sector.
I would like to serve Congolese nation with all the qualities I have. And I think the best way to help this country and yourself, it seems that it is in politics. So I would like to stand as a member of parliament ... (Male midwife, 30–39 years, LH interview, Bunia)
Reasons for leaving midwifery: Some midwives found it difficult to juggle caring for their children, family and sick relatives and work as a midwife, and made the difficult decision to give up their work.
Three years ago, my husband had a very serious stroke that unfortunately left him completely paralyzed. I have to be with him for most of my time, as he cannot help himself. I really have to take complete care of him; you know he is my husband. (Female ex-midwife, 30–39 years, LH interview, Aru)
Some midwives talked about the stress and workload as a midwife becoming too much and wanting to try a new job that was less demanding and allowed more time for themselves and their families. One midwife described how midwives gave up their jobs, as they were held responsible by the community for the death of a mother.
… if a woman dies during delivery, then you will be in trouble with the whole community, as everyone in the village will be pointing at you that you are the person who killed their mother, their sister … (Female ex-midwife, ≥40 years, LH interview, Bunia)
… some just leave because they feel that it is time they do something different, less stressful, and you have enough time for yourself and the family. (Female ex-midwife, ≥40 years, LH interview, Bunia)
Insecurity in the area was another reason pushing some midwives to leave their profession in rural areas and to move to Bunia to start something different.
I left Mongbwalu because of the war, ethnic clashes; otherwise I was happy working as a midwife. When I fled to Bunia with my family, I was working in a private clinic. I left there again because of the war, as bombs were falling … Then, I started the business of working with NGOs, and I do not wish to work again as a midwife. (Female ex-midwife, ≥40 years, LH interview, Bunia)
Challenges of working as a midwife
The midwives identified many health systems and sociocultural challenges that they faced in doing their work. These are problems related to an underresourced health system, but some are clearly exacerbated by fragility and conflict.
Health system challenges: The midwives reported that there was a severe shortage of midwives; some facilities had one or two midwives, whereas other facilities had none. This created a huge workload for the existing staff, high levels of stress and exhaustion. This has been exacerbated by conflict, as midwives and other staff do not want to work in these areas, and where possible move to safer places.
You know in most of our health facilities, apart from the referral hospital where there are two midwives, there is either no midwife or just one … it is massive if you are the only qualified midwife. (Female midwife, FG discussion, Adja)
All midwives reported precarious financial situations. They are supposed to receive a monthly salary (estimated at US$55–80 per month) as well as a monthly risk allowance (US$20–50 per month). None received the salary, and only a few received the risk allowance, which they perceived as being inadequate. This is a key reason why most midwives as well as nurses do not wish to work in these settings.
… the other challenge is about our financial incentives, we do not receive anything from the government, we are just paid from the income locally generated … (Female midwife, FG discussion, Adja)
Midwives and ex-midwives from the three districts described working conditions in the government facilities as very poor. Most facilities were struggling with basic supplies such as gloves and delivery kits, which increases the risk of infection for women and midwives. There are no reliable means of transport for pregnant women who need to be transferred to a referral hospital. The shortage of drugs and supplies as well as the referral challenges have been exacerbated by conflict. The midwives reported that the few supplies in the facilities were often looted by the militia. Travelling to and from the facility was fraught with danger as the militia patrolled the roads and attacked midwives, women and their families. They also reported feelings of helplessness when there were women with complications, as they struggled to manage complications because of lack of medicine, supplies and equipment, and were reluctant to refer them as the roads are so dangerous.
Sometimes you work with torn gloves, if there are any surgical gloves, I was using it just in case [to protect from infections]. There was a problem of transfer of difficult cases, as you know our referral hospital was at Biringi – it’s really a distance, and road conditions are not so good. (Female midwife, ≥40 years, LH interview, Aru)
… there were some pregnant women with obstructed labour, and they were to be transferred to the referral hospital, but they could not, as the area before reaching the referral hospital was already occupied by the other militia group. So, the midwife and the nurse who were there tried to help, but as they did not have enough equipment, they lost those women and their babies … (Female ex-midwife, ≥40 years, LH interview, Bunia)
In contrast, the faith-based health facilities were reported to be better equipped with staff, supplies and drugs, and midwives felt better supported. The Church Medical Coordination take an active role in supporting health workers in the church facilities.
Where I have been working, there was not much challenge related to equipment and supports as they were Catholic health facilities, and they were really well organized … (Female midwife, ≥40 years, LH interview, Bunia)
Midwives, mainly from the rural district, reported that they received little in-service training and supervision, which negatively affected their work. Most training is organized in the urban areas, and they could not attend as they were asked to pay for their own transport, which they cannot afford, and travel is risky given that the militia was patrolling the roads. The scheduled monthly supervision rarely happened and, when it did, it only included the head nurse of the facility.
… if there is organized training for midwives, or for capacity building or in-service training, most of it is limited in urban areas and midwives in rural districts are less well trained than midwives in urban areas. (Female midwife, 20–29 years, LH interview, Adja)
Women are reluctant to disclose their pregnancy in the early stages, especially in Adja and Aru districts, as they believe the baby will die during pregnancy or birth, and so they access antenatal care services late in pregnancy. Women in labor often come to the health facility on their own as they do not want others to know that they are in labor – they believe that this will cause complications and result in the death of the mother or baby. This is challenging for midwives who rely on the family to support the women during childbirth, and particularly if complications arise and referral is needed.
… Because in our environment here, declaring oneself pregnant is not easy, it must first take time. (Female midwife, ≥40 years, LH interview, Aru)
Midwives from rural and peri-urban health districts reported that they were held responsible by the local community when a woman died during childbirth.
Midwives from Bunia and Aru districts described the gender norms of male midwives not being accepted in rural communities (most male midwives work in urban areas), and married female midwives not being allowed to work due to family responsibilities. In addition to this, women were less likely to choose to work in conflict and unstable areas.
… In a community like ours here, especially in remote and rural areas, having a male midwife in the health facility that means that women will not attend services, as they will feel that they do not respect them. (Female midwife, 30–39 years, FG discussion, Aru)
Coping strategies used by midwives
Despite these resource limitations and difficult conditions, midwives demonstrated agency by developing both survival and innovative strategies to address these challenges. This enabled midwives to continue playing key roles in linking communities to health systems. For their survival, in order to look after their family and generate income, some midwives grew food on the land around the health facility. The local authorities allowed midwives to use this land whilst they worked at the facilities.
We have got land around the health facility, and we cultivate and grow food, I have for instance a farm which is around 3 km2. So, we live on the food we grow and sell some, and that money also helps. (Female midwife, ≥40 years, LH interview, Adja)
Health facilities in all districts used a percentage of income generated from user fees to pay health workers. They also allowed the service users to pay in kind if they had no money.
… we do not receive anything from the government, we are just paid from the income locally generated, and what we receive does not really help us. (Female midwife, FG discussion, Adja)
Where people cultivate a lot, they bring food, and they estimate the value and nurses consider it. (Female midwife, ≥40 years, LH interview, Aru)
Midwives also developed innovative strategies to address their challenges. To deal with the small number of midwives in rural health facilities in Aru and Adja, traditional birth attendants worked in the health facilities. The traditional birth attendants play an important role in communities, as they attend nearly 50% of deliveries and are trusted by women and families. The head nurses, with the district health officer, identify the attendants working in their communities, train them in pregnancy, delivery and community awareness, and then integrate them into the health facilities to support the existing health workers. The traditional birth attendants escort women in labor into the facilities and assist the staff during labor, delivery and the postnatal period. The attendants are paid from the income the facility generates from user fees.
The head nurse, in partnership with the health centre committee, and the midwife organized a census where they identified different traditional birth attendants in their area, recruited them for a training on basic midwifery practices, and after they completed, they were integrated to support the midwife in the health centre maternity services. (Female ex-midwife, 30–39 years, LH interview, Aru)
To address the issue of limited equipment and supplies, midwives used the income generated from user fees and lobbied local organizations or the district authorities to buy basic equipment and supplies. In addition, midwives asked pregnant women in the antenatal care clinic to bring basic supplies for delivery.
… from the small amount they generate, they make for instance 15% for buying basic supplies such as gloves, and others, 40% for buying medicine, 40% for financial incentive to staff, ‘salary’ and 5% for administration. (Female ex-midwife, 30–39 years, LH interview, Aru)
Some women bring their own basic elements, such as razors, and other simple supplies as we normally tell them during antenatal clinic. (Female midwife, 30–39 years, LH interview, Aru)
Concerning professional support, midwives, especially from Adja and Aru districts, organized local weekly seminars where a topic was presented and discussed.
… we used to have local sessions here at the health centre once a week where there was a talk on different subjects related to health, it was very good … (Female midwife, ≥40 years, LH interview, Aru)
To deal with transport challenges, midwives and ex-midwives explained that they organized motorcycle taxis to take women with complications to the referral hospital. Relatives were responsible for paying the transport fee. Transport is particularly challenging in the rainy seasons when the roads become difficult to pass, and travel time becomes much longer. Midwives advised women who had signs that they may develop complications to go early to the referral hospital.
… especially in rainy seasons … we just advised head nurses, once they identify risk factors, they had to organize themselves to transfer those women early enough, as the risk signs would be identified during antenatal care clinic … (Male midwife, 30–39 years, LH interview, Bunia)
Discussion
Data of this study were presented in two different ways. The first is through a chronological approach, which makes sense of the life history approach deployed. This shows through time the aspirations to become a midwife (eg service to community, personal experience of death of a baby, vocation and family expectations/role models); the different experiences of midwives (challenges were particularly pronounced for rural midwives because it is in these contexts where staff shortages are the most severe); and future aspirations. Second, the experiences of these critical frontline midwives who are working in extremely poorly resourced and undersupported environments were looked in depth and as such arguably acting as an interface between poor rural/semi-urban and urban communities and the health system. Three areas will now be discussed: how midwives’ working experiences match their initial aspirations to become a midwife; midwives’ resilience and coping mechanisms; and how to better support these critical health workers.
Aspirations versus realities of working as a midwife
The aspiration to become a midwife revealed trends identified elsewhere: experiencing personally or witnessing tragic events around pregnancy and childbirth32; midwife role models33, caring roles, childhood aspirations and family expectations34; and the influence of parents/friends35,
As the data show, the reality of working as a midwife is incredibly challenging, and insights from ex-midwives show the difficult choices some made to leave the profession they were initially committed to. Fragility, conflict and rurality exacerbated these challenges and was a key overarching theme. The current Ebola outbreak will bring additional risks and concerns for themselves, their families and their relationships with communities. Moving to safer areas was a decision made by some midwives, and this is documented in other studies of health workers in fragile and conflict-affected settings1,36,37, leaving these communities with even fewer health services. Those who left midwifery did so mainly because of additional family responsibilities and in some cases for personal reasons, echoing studies in fragile and conflict-affected states1. Those who remained as midwives had aspirations to continue serving, following further education in the hope that this would provide better salaries and employment opportunities. Others saw this role as a stepping stone to other career pathways.
Resilient, brave and innovative – characteristics of a rural Ituri midwife
It is clear from the data that midwives have a critical interface role between the health system and communities in the challenging contexts of Ituri Province. This has parallels with theories of interface positionalities such as street-level bureaucracy38,39, which places the spotlight on agency and coping strategies of people linking between communities and institutions or systems. The lack of supervision, support and regular remuneration means that the experiences of midwives are more on a par of those of volunteers or community health workers in other contexts40. All categories of midwife (current and ex, all districts, and women and men) found work environments challenging, although this was particularly acute in rural contexts and those with active conflict, as found in other studies37. The key factors shaping their experiences included work environment, social-cultural components, personal belief and family (lack of) support. Despite these challenges, midwives innovated and showed agency in coping as in other rural settings of Africa, for example lobbying local NGOs to buy basic equipment and supplies, and organising motorcycle taxis for referrals41. However, growing food on land provided by the facility and organizing local weekly seminars to update knowledge were specific innovations of these groups. It is important to understand midwives’ coping strategies to recognize their resilience but, importantly, to find ways to better support them within the realities of the challenging contexts in which they work. Within DRC, Ituri Province experiences a very high number of maternal deaths, and DRC has one of the highest maternal mortality rates in the world. It is critical to hear these stories in order to address the constraints midwives experience, and build on supporting them in developing new coping strategies, so that they can fulfil their vital role in addressing maternal mortality.
Supporting midwives
Understanding the career pathways of midwives is important to understand the support they need when they are working in rural, fragile and conflict-affected settings and in poorly resourced health systems. Given the human resources for health shortages, training and development of additional midwives is a key priority, as is ongoing in-service training for existing midwives to update their skills and demonstrate their value. This is particularly important for rural midwives who are more isolated, find it harder to access materials due to lack of resources and conflict. Improving living conditions, such as housing close to the facilities, and better modes of communication, will help attract and retain qualified midwives in rural and remote health facilities. Supporting midwives with supplies and equipment will enhance their ability to perform well, improve their relationships with communities and build trust. This involves supporting district health teams to be able to negotiate for additional resources from the government or NGOs and use them wisely. Supervision and support for this critical cadre from both health systems and communities need further investment, particularly in contexts of chronic insecurity. A range of actors such as government, churches, NGOs, civil society, associations of nurses, association of midwives and nursing training institutes can be brought together at the annual Provincial Health Review to discuss the issues faced by midwives and come up with plans that are context specific.
Midwives are acting as street-level bureaucrats who are frontline workers interfacing with very poor and marginalized communities38. They adapt policies and make choices about how to provide services, developing routines and simplifications that help them to deal with dynamics such as the chronic shortage of resources and the often high demand for their services39,41. Midwives innovate and share strategies and resources, and these initiatives need to be supported. Initiatives at community level to recognize and value rather than blame this cadre need to be encouraged, such as radio announcements, awareness-raising at markets, churches, schools or community gatherings. Social media can be used to provide opportunities for peer support and sharing of ideas, as seen with health workers during the Ebola outbreak in Sierra Leone35. They created a WhatsApp group about Ebola fighters, encouraging each other to continue to work, stay safe and follow precautions through daily messages35. Health facility committees, which develop plans and budget of facilities, mobilize the community to use health services, ensure the availability of drugs and equipment and make sure that health facilities deliver quality healthcare services42, can have an important role in fostering support from communities for their health staff. They can explain the important role of midwives, confirm the challenges that midwives face, and explore possible solutions and support for their staff. The contribution of midwives who continue to serve during periods of conflict should be recognized and celebrated, through for example, awards for ‘midwife of the year’, communicated through radio announcements and at community events43. Regular remuneration will support productivity, reduce costs and opportunity costs of finding other ways to survive, and it means that user fees can then be used to upgrade facilities and directly benefit users.
Strengths and limitations
The strength of the approach is that research was conducted by a DRC team embedded within the context of fragile rural Ituri Province, bringing their tacit knowledge to the study. This team was best placed to capture the perspectives of current and ex-midwives through time (using life histories) and explore the coping strategies of this cadre whose voices have never been heard. There were challenges, however: in rural Adja district the researchers were not able to obtain views of ex-midwives living in rural areas because they were no longer within the district. The focus was on the experience of midwives, and it would be important in future studies to include the community perspective.
Conclusion
DRC is one of three countries that together constitute 50% of maternal deaths worldwide. Rates of death are particularly high in rural fragile areas such as Ituri Province. Midwives have a critical role in attempting to support women to deliver babies safely. Data from this study show the immense challenges they face and their bravery and resilience as they navigate the interface position between underresourced health systems and poor, marginalized communities. But resilience should not be taken for granted; it should be supported. If women’s lives really matter, then this situation requires a call to action: donors need to prioritize these contexts; and the government and other stakeholders such as the churches, civil society, NGOs and association of nurses and midwives, in DRC, need to invest more in improving security conditions as well as working conditions and professional support for midwives in rural Ituri Province. Only then will midwives, at the interface between health systems and the communities, be able to provide the critical services that women and their families need, and therefore contribute to achieving universal health coverage.