Context
Japan has a specialist-driven medical system with a disproportionate distribution of medical practitioners, concentrated in urban areas1,2. This presents a number of challenges in Japan, where there is an ageing population and over 7000 small islands3. Over 50% of the rural and remote population of Japan is elderly3. The maldistribution of physicians in Japan has been a concern to medical educators and policymakers for a long time1. Significant efforts have been made to address this, including the establishment of at least one medical school in each prefecture in the 1970s and 1980s3, the foundation of the Jichi Medical School in 1972 (now Jichi Medical University) and the Chiikiwaku rural training quota policy established in 20091,3.
There have also been significant efforts to increase the overall physician supply in Japan. Between 1998 and 2008, physician numbers increased nationally by 13.6% compared to a population increase of only 0.95%4. Recent workforce projections have indicated that the overall demand and supply for physicians in Japan will be in balance by 20245. However, the geographic maldistribution of the medical workforce has continued and, with the expected decrease in younger physicians practising in rural areas, there is concern that this will worsen5. Even a positive projection of physician supply for the Hokkaido prefecture undertaken in 2017 concluded that, despite a forecast balance for 2019, areas within the region will remain at risk of physician undersupply2.
The problem of an inadequate rural workforce is exacerbated by the lack of an effective dedicated pathway for rural generalist training. Primary health care has only recently been recognised as a medical specialty in Japan, with the establishment of the Japan Primary Care Association in 2010 and the new board-certified training program commencing in 20183. The lack of awareness of the role of primary care practitioners, coupled with a shortage of available training posts, is part of the challenge faced by primary health care as it continues to develop1,6. However, there has been a more recent focus in the literature on the potential for the role of the rural generalist as part of a strategy to address the physician maldistribution in Japan1,3,6-8.
A recent scoping review exploring the question ‘What is documented on rural generalist medicine?’ identified 102 relevant articles internationally. The authors noted contextual differences and similarities in a variety of themes including the definition of rural generalist medicine (RGM), the training pathways and programs, the scopes of practice and service models, the enablers and barriers to recruitment, and retention and recommendations for reform. Despite variations, the authors observed RGM has been a feature of the healthcare system in countries with substantial rural and/or remote populations for some time9.
The review authors further highlighted that, while most of the literature originates from Australia, Canada and the USA, which have developed relatively mature models of RGM, more recent literature is emerging from countries such as Japan, Kenya, Uganda, Rwanda, Ethiopia and India. They note efforts to coordinate and strengthen RGM pathways and models of care as a response to the issues faced globally by the health sector in rural and remote areas. They also call for ongoing research and publication of evidence related to RGM training and health outcomes. They conclude that dissemination of evidence and experience through publication and forums such as the world rural generalist summits is now required to support best practice outcomes as this momentum continues to build9.
The Cairns Consensus Statement, developed at the first world summit in 2014, describes RGM in the following terms10:
The provision of a broad scope of medical care by a doctor in the rural context that encompasses the following:
- Comprehensive primary care for individuals, families and communities;
- Hospital in-patient and/or related secondary medical care in the institutional, home or ambulatory setting;
- Emergency care;
- Extended and evolving service in one or more areas of focused cognitive and/or procedural practice as required to sustain needed health services locally among a network of colleagues;
- A population health approach that is relevant to the community;
- Working as part of a multi-professional and multi-disciplinary team of colleagues, both local and distant, to provide services within a ‘system of care’ that is aligned and responsive to community needs.
The concept of a rural generalist is well developed in Australia, where there are many underserved rural and remote areas due to its vast geographic area and relatively small dispersed population. Rural generalists typically work in primary care clinics and hospitals as general practitioners, with additional skills in emergency medicine and public health. Rural generalists also have one or more extended skills in disciplines such as anaesthetics, obstetrics and gynaecology, general surgery, internal medicine and Indigenous health. Their work settings may include private practice, rural hospitals or a mix of the two, or with other organisations such as Aboriginal Community Controlled Health Services and the Royal Flying Doctor Service. Irrespective of the mechanism of employment, the focus is on meeting the needs of the community, with development of appropriate training pathways and vocational recognition11.
Australia is embarking on a national roll-out of a rural generalist pathway. The Queensland Rural Generalist Program is a mature example, developed in 2007 to meet the needs of Queensland’s rural and remote communities via a supported career pathway for junior doctors to train in rural and remote medicine12,13. A 2013 report notes ‘the pathway joins evidence with policy to achieve professional recognition, credentialing, and industrial recognition’13.
From an initial 30 trainees in 2007, by 2019 a total of 350 registrars were supported by the pathway, with 124 Fellows having completed their training. Of these, 64% have remained in Modified Monash Model locations (remote communities and small rural communities with population <15 000) for more than 5 years. The growth of the pathway points to the deficit in workforce that needs to be addressed and the substantial capacity to train in rural practice14.
A 2014 report described three interdependent pillars of rural workforce. All three pillars – supply, training and the working environment (closely linked to retention) – must be strong to ensure that the structure does not collapse. This analogy has implications for other jurisdictions, such as Japan, seeking to develop rural generalist models appropriate for local needs15.
Issue
A Japanese organisation, GENEPRO, established the Rural Generalist Program Japan (RGPJ) to support medical training in rural areas and remote islands, with the first cohort of seven registrars enrolled in 2017. The training scheme and curriculum were based on best practice and lessons learned from Australia, Canada, Norway, the Philippines and Taiwan. The Australian rural generalist model was instrumental in the initial design and delivery of the RGPJ. The program’s founder experienced vocational training for rural doctors in Australia during the initial phase of RGPJ development, and was immensely inspired by the remote supervision model.
The program was developed by an emergency physician with both institutional and individual support from numerous partners in Australia: the Australian College of Rural and Remote Medicine (ACRRM), the Royal Australian College of General Practitioners Rural, the Rural Doctors Association of Australia, the Remote Vocational Training Scheme (RVTS), James Cook University and Queensland Country Practice (QCP), Darling Downs Health. These groups all collaborated with the RGPJ, sharing their expertise in rural education and training. QCP and RGPJ signed a memorandum of understanding to enable an observership for the elective placement in Queensland. The program has been certified by ACRRM. Registrars who completed training requirements and the assessment program are awarded the Certificate of Completion of Training of RGPJ jointly by ACRRM and RGPJ.
The program was developed to ensure it was tailored to regional and local contexts, focusing on provision of a broad scope of clinical care with a unique combination of abilities and aptitude to respond to community needs. This brought together various members of the healthcare team including general practitioners or family physicians with community-based primary care roles, hospitalists, emergency physicians and a range of consultant medical specialists.
The global standards in postgraduate medical education developed by the World Federation for Medical Education (WFME) will be used to describe the RGPJ in more detail. These standards define nine categories (Box 1), designed to be applicable globally. The World Organization of Family Doctors (WONCA) Working Party on Education has developed specific educational standards for family medicine around this framework16.
The following section is organised according to the WFME standards outlined and illustrate how RGPJ strives to meet the WFME educational standards.
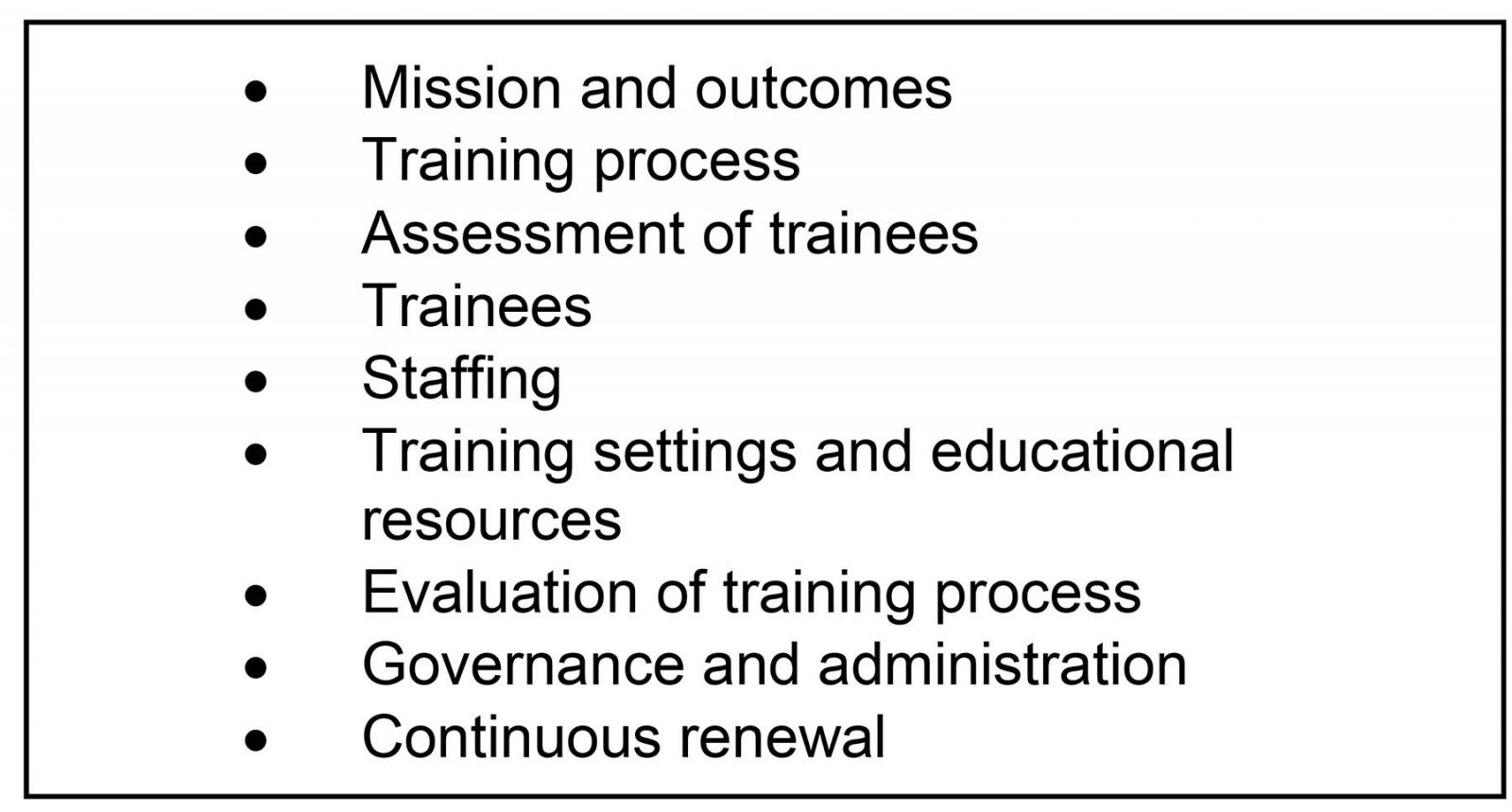 Box 1: World Federation for Medical Education standards in postgraduate medical education.
Box 1: World Federation for Medical Education standards in postgraduate medical education.
Mission and outcomes
Efforts made by national and local governments and the introduction of chiikiwaku, a regional quota scheme in medical schools, have contributed to increase the number of physicians prepared to work in rural and remote Japan17. However, the discussions have shifted from satisfying target numbers of physicians to the quality of education and clinical training specifically addressing the needs of rural and remote contexts3. Takamura et al (2017) asserted that political interventions such as student-recruitment systems are essential, but medical school curricula have become more important than ever, with an urgent need to refine and expand clinical training in rural areas3. Annual survey findings from the Ministry of Education, Culture, Sports, Science and Technology also raise the lack of career pathways and workforce development as concerns in the current educational system 18.
The RGPJ’s mission directly responds to such needs addressed in the policy and academic arena in medical education and public health. The mission specifically underscores the importance of practice and training to address:
- improved access to health care and health outcomes for rural and remote areas in Japan
- increased rural medical workforce
- increase in appeal and interest in doctors pursuing careers in rural medicine
- introducing the concept of rural generalism and establishment as a specialty19.
No definitive outcomes are available at this stage but an evaluation strategy is underway.
Training process
The RGPJ commenced as a 15-month training program, which includes local and distance supervision of registrars, onsite training at training hospitals, webinars and elective placements. There are three components of registrar training: onsite domestic training in a rural or remote hospital for 12 months, webinars featuring online discussions and lectures by rural generalists, and elective training for up to 3 months19. The program length was set in accordance with requirements of other specialist training programs in Japan, but may evolve in the future. The RGPJ will incorporate best practices from international models, incorporating learning modes feasible in the Japanese postgraduate certified general practice training scheme and educationally beneficial for the registrars.
The RGPJ’s training program is designed to allow registrars to develop their knowledge and procedural skills without leaving remote locations. In-practice supervision is provided both by local supervisors and remotely, using principles drawn from the Australian RVTS20. Online discussions, lectures and self-study utilising ACRRM’s online learning platform overcome distance and time constraints. Australian rural generalists and Japanese instructors are responsible for online discussions and lectures. For procedural techniques, hands-on training is provided through combined workshops twice a year.
Objectives of the elective placement are to gain experience of other healthcare systems, broaden the mind about roles and achievements with global perspectives, and bring global health to life by exposure to different research and policy environments. Many registrars undertake an elective observership in rural Australia through the partnership with QCP, while others undertake global health training in developing and developed countries such as Nepal, Vanuatu, Mongolia, the Philippines, Taiwan and Norway. Some registrars undertake short-term training within Japan in specialised fields such as obstetrics, anaesthetics and orthopaedics.
The program is designed for registrars to acquire English language skills as part of their elective training, sufficient to allow participation in English in clinical work and academic conferences. Registrars are further encouraged to build their network of rural and island medicine doctors worldwide and to develop their broad knowledge of rural and remote health, workforce development and training programs19.
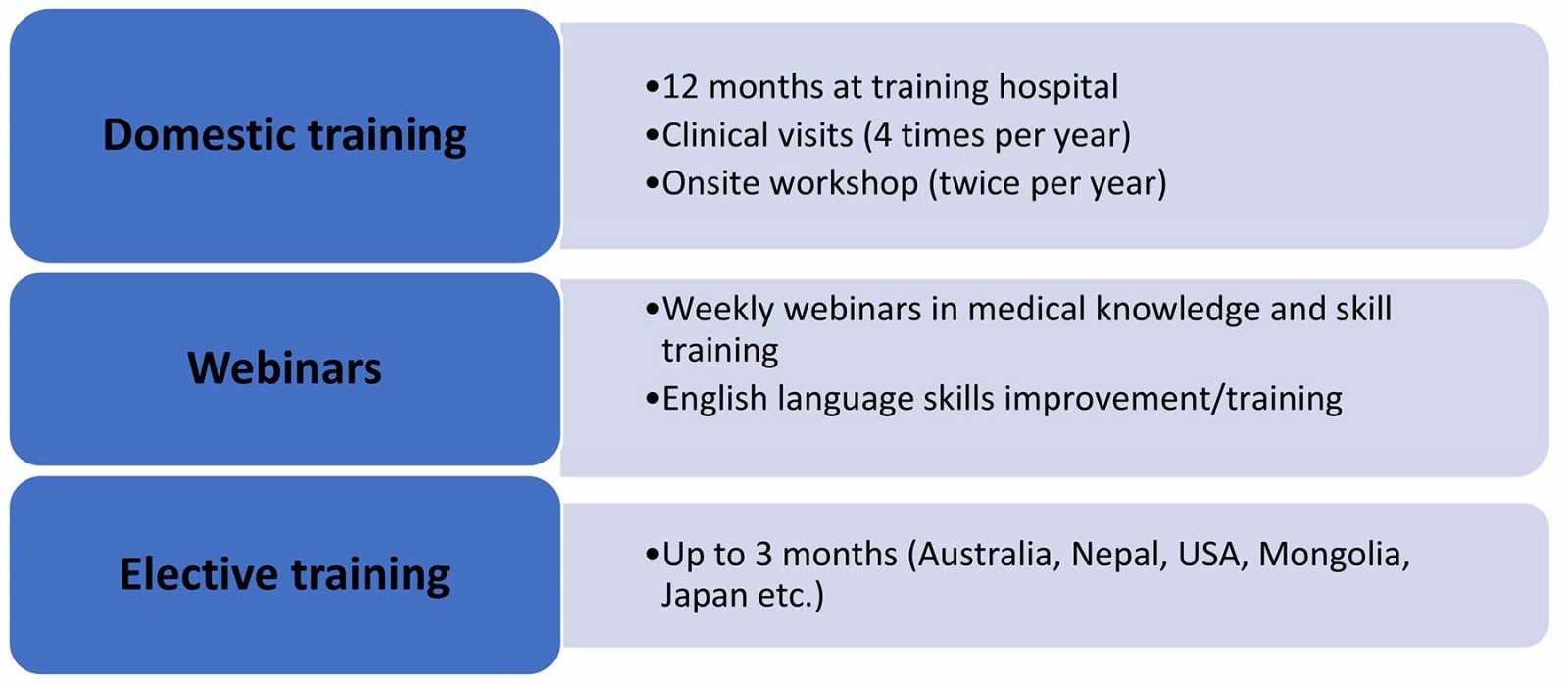 Figure 1: Overview of the Rural Generalist Program Japan.
Figure 1: Overview of the Rural Generalist Program Japan.
Assessment of trainees
Assessment of trainees (called registrars in the RGPJ) is based on the approach developed by ACRRM for its Fellowship exam21:
- MiniCEX (mini clinical evaluation exercise)
- Case-based discussions
- supervisor feedback reports.
The RGPJ is certified by the ACRRM, and registrars who complete training requirements and the assessment program are awarded the Certificate of Completion of Training of RGPJ jointly by ACRRM and RGPJ.
Trainees
A prerequisite for entering the training program is completion of 2 years of postgraduate internship and commitment to rural/remote medicine. Recruitment seminars are scheduled regularly in locations such as Tokyo, Osaka, Yokohama and Fukuoka. Applicants need to submit their resumes to GENEPRO. They then undergo a selection interview and visit their prospective training hospital for an interview with the director of the hospital. Final decisions are made by GENEPRO staff in consultation with directors of the training hospitals.
As summarised in Table 1, registrars have substantial prior experience. The inaugural class had a median age of 38 years and were in postgraduate years 4–13. Most had achieved specialist status, including four in emergency medicine.
Table 1: Registrar demographics for Rural Generalist Program Japan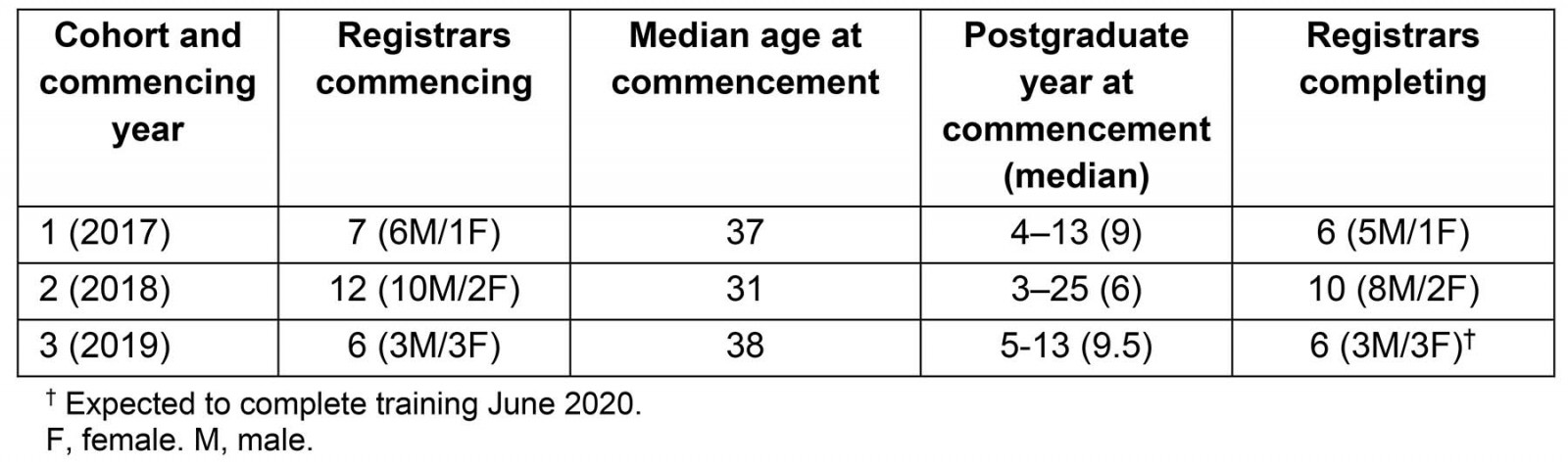
Staffing
The program director is supported by staff skilled in administration, business management and human resources, and is responsible for the overall management of the program and external representation and advocacy. He also liaises with supervisors at training hospitals, and other educational staff, and undertakes clinical visits to monitor the training environment and support participants in the program. Registrars are supported with three levels of supervisors: one onsite in the local hospital, another in the community and a third available for online support. Figure 2 summarises the overall organisational structure.
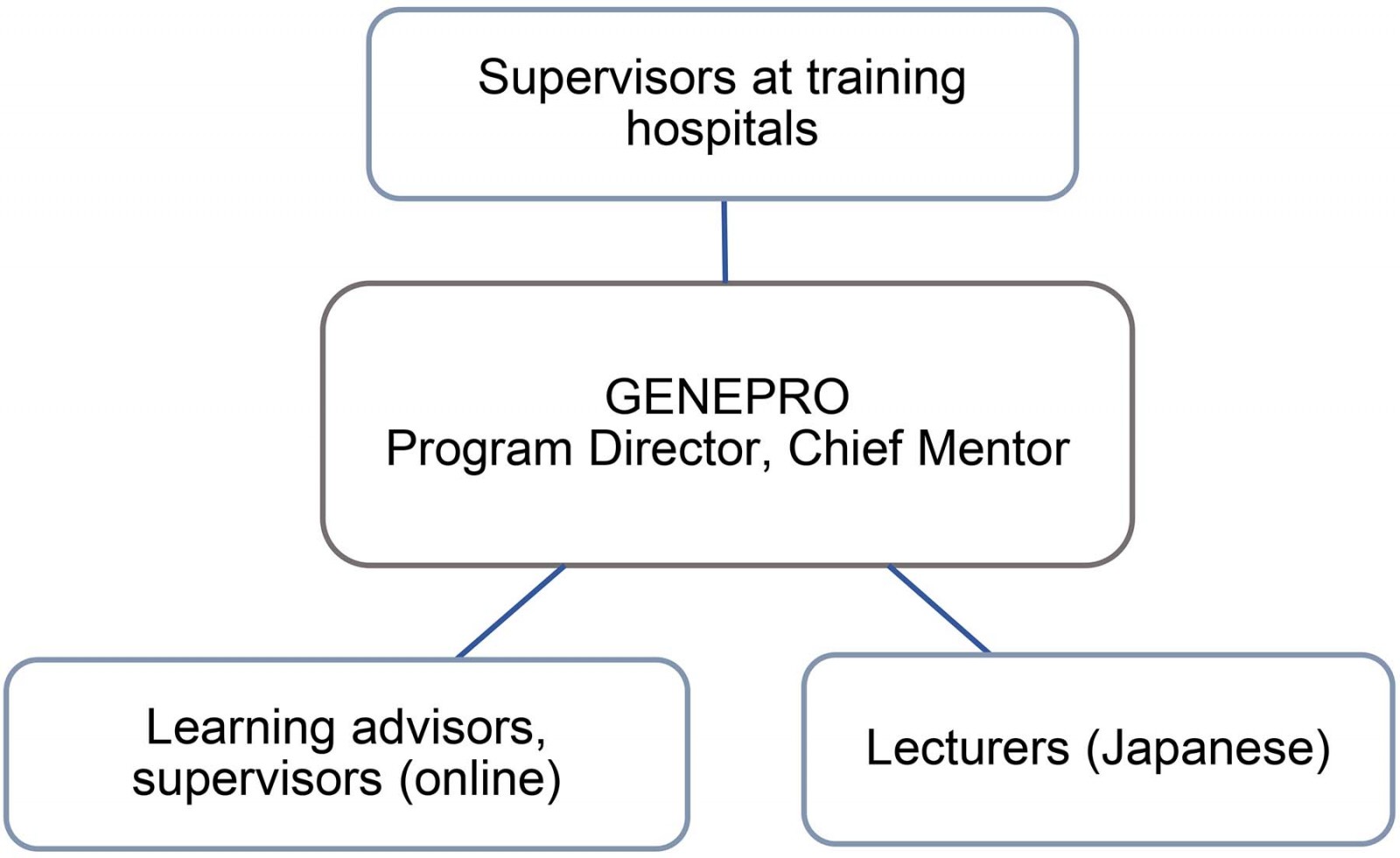 Figure 2: Rural Generalist Program Japan organisational structure.
Figure 2: Rural Generalist Program Japan organisational structure.
Training settings and educational resources
Registrars undertake training at six hospitals including two of the more than 400 inhabited Japanese remote islands (Fig3).
GENEPRO’s training hospitals are selected based on the following criteria:
- rurality/population
- deep and acute understanding of issues surrounded the rural medicine
- dedication to solving workforce shortages
- commitment to training young doctors as future investment/collaborative endeavour rather than treating them as temporary human resources at their hospital.
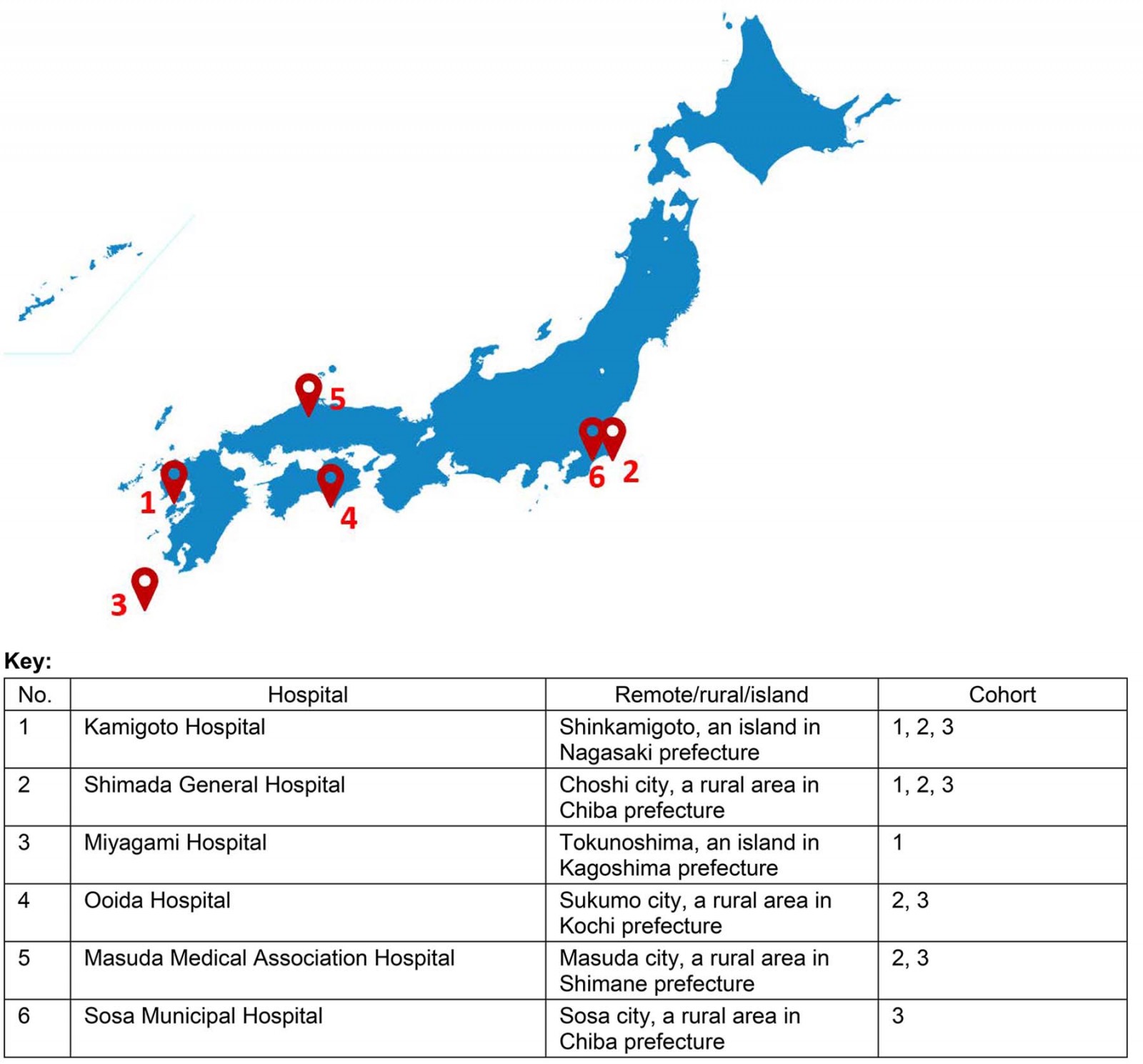 Figure 3: Rural Generalist Program Japan training locations.
Figure 3: Rural Generalist Program Japan training locations.
Evaluation of training process
GENEPRO has conducted a program evaluation supported by a professional external evaluator in 2019. The evaluator reviewed the first 2 years of the program with a focus on registrars from the first and the second cohorts. Other key stakeholders included directors at training hospitals, administrative staff, mentors and learning advisors. Because most stakeholders were Japanese, surveys and interviews were conducted in Japanese. The scope of this evaluation included needs assessment, lessons learnt from the first two cohorts of registrars, organisational and management systems to support the registrars, and refining and improving the training program.
The evaluation results indicated that early experience of the program has been positive. Findings and key themes are briefly described below and have been presented at internal meetings22 and academic conferences23.
- increased career aspirations and confidence – the RGPJ program stimulated and reaffirmed registrars’ interests in rural generalist practice.
- increased activities in advocacy, research and policy discussions
- developed competencies in leadership and management at both individual and team levels
- lessons learned transferred to Japan in everyday practice.
Given the program is in its infancy and the number of registrars is small, there are limitations to the sample size and the depth of analysis. However, the evaluation may well inform program development and subsequent evaluations in the future.
Governance and administration
The RGPJ is certified by ACRRM and is based on training approaches developed by ACRRM and the RVTS. The program director consults with representatives of ACRRM and RVTS regularly to maintain quality and accountability in the program development and implementation processes. Further support has been provided by the Japanese Primary Care Association Rural and the Japanese Medical Association.
Continuous renewal
Early experience of the program is positive, suggesting it is meeting a need and is attractive to registrars and training hospitals. Further work needs to be done in concert with the strengthening of Japanese primary care, and international developments in RGM, to ensure a sustainable program that will deliver health care to rural and remote Japan. The program continues to improve indicators for assessment and measure impact of the training outcomes, including cost analysis and longitudinal study of program effectiveness.
Lessons learned
The Japanese experience to date suggests there is a need for a rural generalist program, developed for the local context. Differences in general practice/family practice systems, as well as diverse geographical characteristics and demographics, mean that training should be tailored to meet local needs. The international literature supports this view, with the Japanese program benefiting from international collaboration.
Allocating doctors to remote areas to satisfy workforce numbers does not necessarily fulfil the objective of producing a sustainable workforce. Japan’s challenges of a shrinking labour force, health inequalities and disappearance of cultural heritage, which provides a unique social, economic and political environment, are being addressed by the Japanese government and medical associations, which are developing general practice training24,25.
Strategies such the RGPJ, with other measures such as locum support, are needed to enable rural/remote practitioners to take annual leave and attend continuing medical education activities. Provision of short-term training in remote areas is needed for urban practitioners so they too can provide locum relief. An effective national program needs to focus on connectedness with local communities, understanding local culture and providing appropriate specialist care.
GENEPRO intends to work on evaluating academically whether an increased supply of doctors has improved the quality of medical care in remote areas. The training program will incorporate academic research and evaluation, thereby hoping to contribute to the improvement of the quality of medical care both in rural and urban areas. Results of such efforts will contribute to the discussions on the rural–urban divide and inform future medical education and health policy.
More needs to be done to strengthen the other pillars of rural workforce – supply and the working environment – in order for the RGPJ to meet its vision.
References
You might also be interested in:
2022 - Factors associated with adolescent birth in Indonesia: a national survey
2008 - Clinical placement and rurality of career commencement: a pilot study




