Dear Editor
Pediatric burns are a leading cause of childhood injuries, having significant physical and psychological impact on both parents and children1. Although scald injuries remain the most common mechanism of pediatric burns, several studies in Australia have observed a rising trend of vehicle exhaust system-related burns in children. Motorbikes are a frequent cause of the exhaust burn and many occur outside of metropolitan regions, where motorbikes remain a common and readily available mode of recreation and/or transport2.
Although their size tends to be small, exhaust burns are known to be deeper, require longer inpatient stays in hospital and have more complex sequelae with poorer outcomes compared to other burns2.
The predominance of scald and flame injuries in children has directed focused prevention projects and campaigns. These have reduced the incidence and severity of, and improved outcomes for, various burn injuries3. However, no clear legislation or safety instructions are available in Australia to regulate motorbike use by children. Given the potential effectiveness of prevention strategies, it is essential to provide comprehensive and contemporary information to guide preventative interventions. We aim to raise awareness and provide insight to inform focused prevention strategies in childhood exhaust burns.
Data were extracted from the Queensland Pediatric Burns Registry to perform a retrospective analysis of children who presented to Queensland’s tertiary referral centre for pediatric burns between 1 January 2013 and 31 December 2017. Demographic information retrieved included age, gender, residential postcode and postcode where injury was sustained. The Accessibility and Remoteness Index of Australia was utilised to classify geographical location of injuries as metropolitan or non-metropolitan.
Overall, 243 children were identified as having sustained an exhaust-burn injury (Table 1). Compared to other burns, exhaust burns were more likely to occur in non-metropolitan regions (26.0% v 11.7%, p<0.001). Exhaust burns sustained in metropolitan regions were more likely to involve younger age groups (40.1% v 8.5%, p<0.001). Higher proportions of burns occurring in non-metropolitan areas resulted in a full-thickness wound (30.5% v 12.5%, p=0.003), required one or more theatre visits (49.1% v 31.6% p=0.002) and grafting (58.8% v 34.0%, p=0.002) when compared to exhaust-burns occurring in metropolitan areas. Significantly higher proportions of exhaust-burn injuries occurring in non-metropolitan areas involved motorbikes (93.2% compared to 79.2% in metropolitan areas, p=0.014).
Exhaust burns sustained outside metropolitan regions were more severe and more likely to have longer recovery periods. Hospital visits or admissions can impose a high burden on families, especially for those residing in rural and remote regions.
The provision of adequate first aid can decrease the depth of burn and risk of skin grafting; however, children in non-metropolitan regions of Queensland are less likely to receive adequate first aid by caregivers4,5. The decreased adherence to first aid in combination with increased risky behaviour could contribute to a higher risk of incidence, severity and subsequent morbidity for children in rural and remote regions.
Considering the associated morbidities with exhaust burns in rural and remote areas, prevention efforts should consider a combination of manufacturing modifications, the environment, raised parental awareness and protective clothing to reduce the number or severity of exhaust burns in children.
Table 1: Study demographics and exhaust-burn characteristics for metropolitan and non-metropolitan children recorded in Queensland Pediatric Burns Registry, January 2013 – December 2017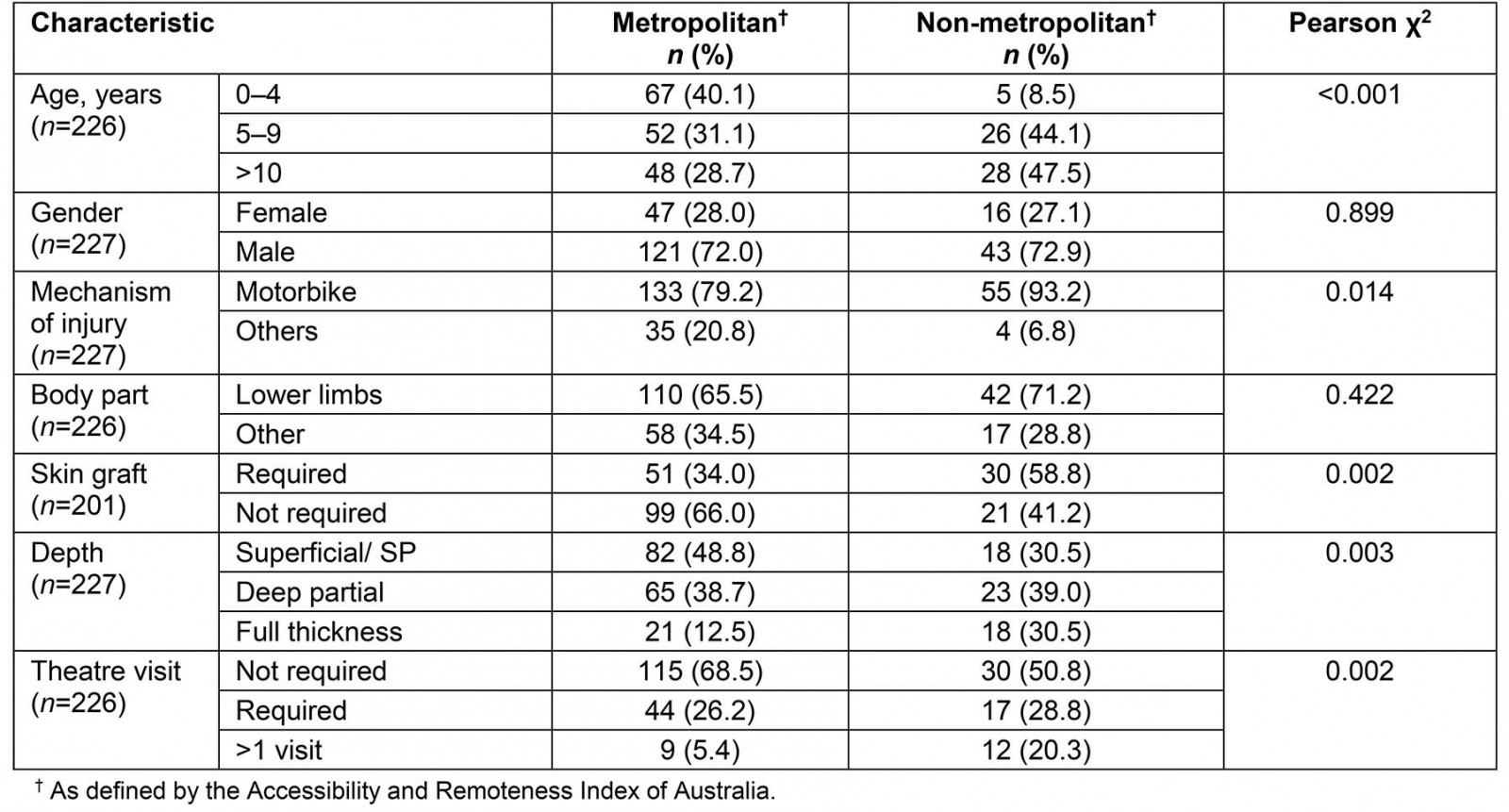
Acknowledgements
Thanks to the patients and clinical staff of the Pegg Leditschke Children’s Burns Centre for their time helping us collect this information.
Bronwyn R. Griffin, Faculty of Health, The Queensland University of Technology
Angelin Ooi, Faculty of Medicine, The University of Queensland
Roy M. Kimble, Faculty of Medicine, The University of Queensland; Faculty of Health, The Queensland University of Technology
References
You might also be interested in:
2014 - Dental practitioner rural work movements: a systematic review

