Context
This article describes the development of a new model of care (MOC) for the rehabilitation of rural and remote paediatric burns patients. The MOC was developed at Townsville University Hospital (TUH), a tertiary referral hospital in northern Queensland. Among TUH specialist services is the North Queensland Paediatric Burn Service (NQPBS) treating approximately 170 children a year who sustain burn injuries. Approximately 29% of the children treated by NQPBS reside in regional communities, 20% in remote or very remote communities across northern Queensland and the remainder from the Townsville region. The NQPBS is not a dedicated burns unit. Rather, it is a burns service within the paediatric ward at TUH, which also provides other specialty services.
Burns are a common injury in children. Deep-partial or full-thickness burns often require hospitalisation and surgical intervention followed by complicated post-surgical rehabilitation to achieve optimal functional performance, minimal scarring and full range of movement1. Optimal outcomes following severe burns are best achieved through specialist multidisciplinary team interventions.2. Within these teams, occupational therapists (OTs) have a major role. OT interventions after burn injury include the management of hypertrophic scarring, joint range of motion, pain and functional ability2. Specialist OT burn services, located in tertiary referral hospitals, are rarely available in rural and remote areas. Thus, patients from rural and remote communities have limited access to these services3,4.
Children from rural and remote areas have a higher likelihood of complications following burn injuries. Complications mean they may require longer length of stay in hospital due to the limited availability of burns resources, specialist knowledge and outreach services in rural areas3. An in-house audit of paediatric burns patients at TUH confirmed rural and remote burns patients received fewer reviews than their Townsville region counterparts. Therefore, the OT-Led Paediatric Burn Telehealth Review Clinic (OTPB Clinic) was developed with the aim of addressing the gap in access to burn rehabilitation services for rural and remote children.
The OTPB Clinic is an expanded scope model of care for the OT. In this model, the paediatric surgeon delegates the role of primary treating clinician to monitor and treat children undergoing active burn rehabilitation to the OT. Recommendations on expanded scope models of care, outlined by the Allied Health Professions Office of Queensland, were incorporated in the development of the model5.
Issues
The model was developed to address some recurring issues that occur in rural health service delivery. First, an in-house audit was conducted to describe service delivery to rural and remote children with burn injuries. The audit revealed clear differences between Townsville and rural and remote children, with the latter having increased complications and receiving fewer follow-up services. The in-house audit conducted between July and December 2016 showed children from rural and remote areas were reviewed on average every 20 weeks by an occupational therapist. Comparatively, children with burn injuries living in Townsville were reviewed at 6–8-week intervals. A range of administrative, clinical, geographical, technical and workforce-related concerns contributed to this inequity (Table 1).
Innovative healthcare models for rural and remote residents often fail because of lack of procedures, guidelines and evaluation6,7. To ameliorate this risk, an experienced OT was employed as the project officer via external funding obtained from the Allied Health Professional Office of Queensland. The dedicated time allowed the OT to develop the new model of care, which included comprehensive guidelines regarding all aspects of service delivery.
Implementing practice change in health services is complex. Therefore, an advisory committee was established consisting of paediatric surgeons, paediatric outreach nurses, a specialist OT in paediatric burns, remote-area OTs and telehealth coordinators. A literature search of previous paediatric burn telehealth services to examine salient design features for translation to the northern Queensland context was conducted8-11. The committee developed service guidelines and pathways using an established e-Learning package12, with the aim of improving access to burn rehabilitation for rural and remote children.
Eligibility criteria for the OTPB Clinic were developed:
- undergone surgical intervention such as debridement, grafting or reconstruction because of their burn injury
- prolonged time to definitive wound healing (>14 days) as documented in the medical record
- identified as high risk of scarring (eg family history of significant hypertrophic or keloid scarring, high-risk ethnicity groups, comorbidities that may be associated with significant scarring)
- ongoing monitoring required by NQPBS (eg patients requiring surgical intervention following dog bite injuries).
Patients were eligible for referral to the OTPB Clinic if they were a patient of the NQPBS and been reviewed by an NQPBS surgeon on at least one occasion.
A specialist OT, working in an expanded scope role, was the lead clinician for the burn review. Paediatric surgeons were no longer involved with clinical reviews unless children met clinical criteria. Clinical criteria for re-engaging the paediatric surgeon were developed by the advisory committee in case further surgical intervention such as reconstruction, releases and steroid injections were required (Table 2). A multidisciplinary approach was adopted for complex patients. This enabled joint telehealth consultations with nurses and/or physiotherapists to address issues such as ongoing wounds or reduced range of motion after complex burn injuries.
Pathways for burn rehabilitation were customised to individual family situations. Children within a 30-minute drive of TUH continued via the usual care pathway (ie face-to-face visits with the paediatric surgeon). Children discharged to hospitals visited by the NQPBS surgeons (Cairns and Mackay) were referred to their local OT including face-to-face review by the visiting surgeon. Children from rural and remote areas were reviewed via telehealth by the Townsville-based OTPB Clinic.
Family choice was incorporated into the service design and delivery. Therefore, a range of service models to deliver the OTPB Clinic were developed to account for differences in family access to telehealth and local health professionals. The OTPB Clinic uses existing telecommunications technology available in families’ homes and includes an expansive network of telehealth technology in hospitals and primary health clinics in rural and remote sites. Appointments could be delivered to the family home using video-conferencing software (for smart devices) or the Queensland Health Telehealth Portal (on a household computer) using a collaborative meeting room. Infrastructure and hardware to support telehealth is highly variable in rural and remote areas, which meant that, for some families, home consultations were inaccessible. Alternatively, the family could choose to attend their local rural hospital, community health service or clinic to access Queensland Health telehealth services.
Review appointments in rural settings were scheduled to include local clinicians. The models to include local clinicians were the same profession, if a local OT was available, or a different profession (eg clinical nurse, Indigenous liaison officer or other allied health professional) if no local or visiting OT services were available12. The local health professional assisted in several tasks for the review and in turn they were upskilled in burns rehabilitation by the OTPB Clinic’s OT (Table 3). Clinical reviews were completed solely by the OTPB Clinic if no local services were available.
Efficient and timely service delivery was sought through the support of allied health assistants (AHAs)13. Delegation of clinical tasks to an AHA (Table 3) were developed using the Calderdale Framework14,15. Educating families to use the technology to enable home consultations was completed by the AHA prior to appointments.
Table 1: Root cause analysis of inequity of service delivery for paediatric burn injuries in rural and remote northern Queensland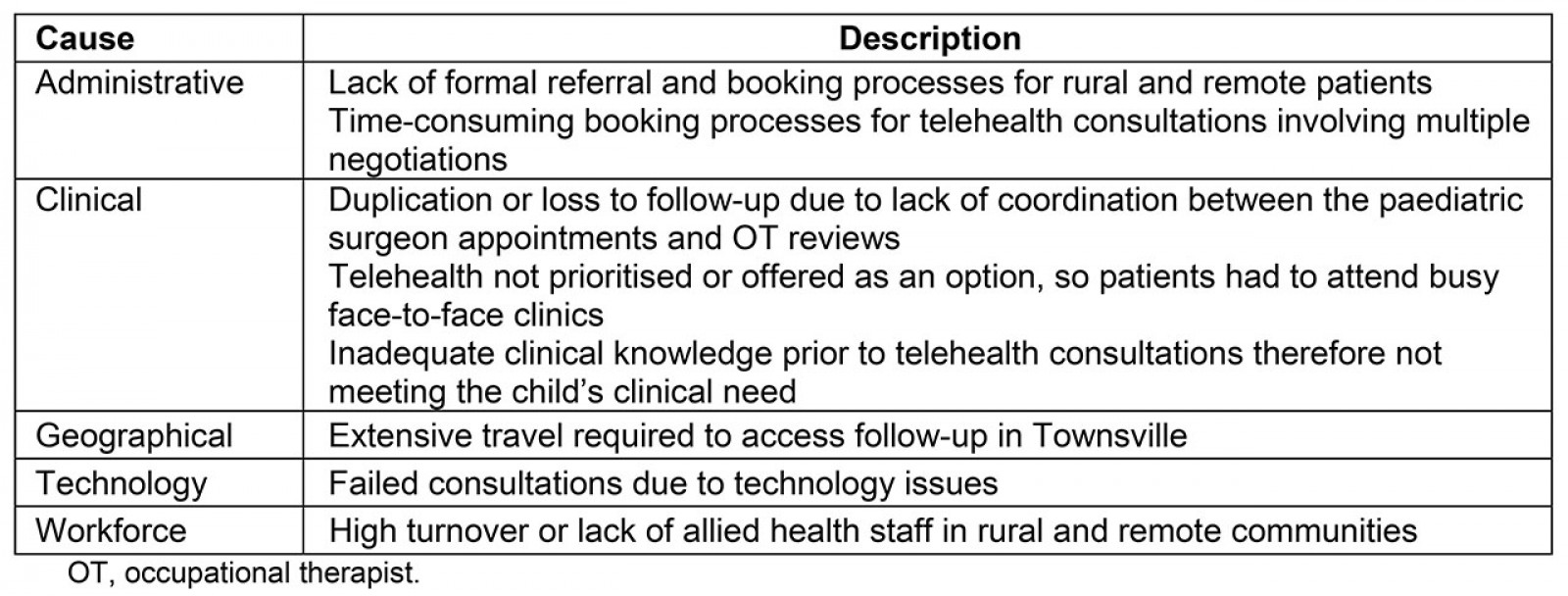
Table 2: Clinical criteria for re-engagement with paediatric surgeon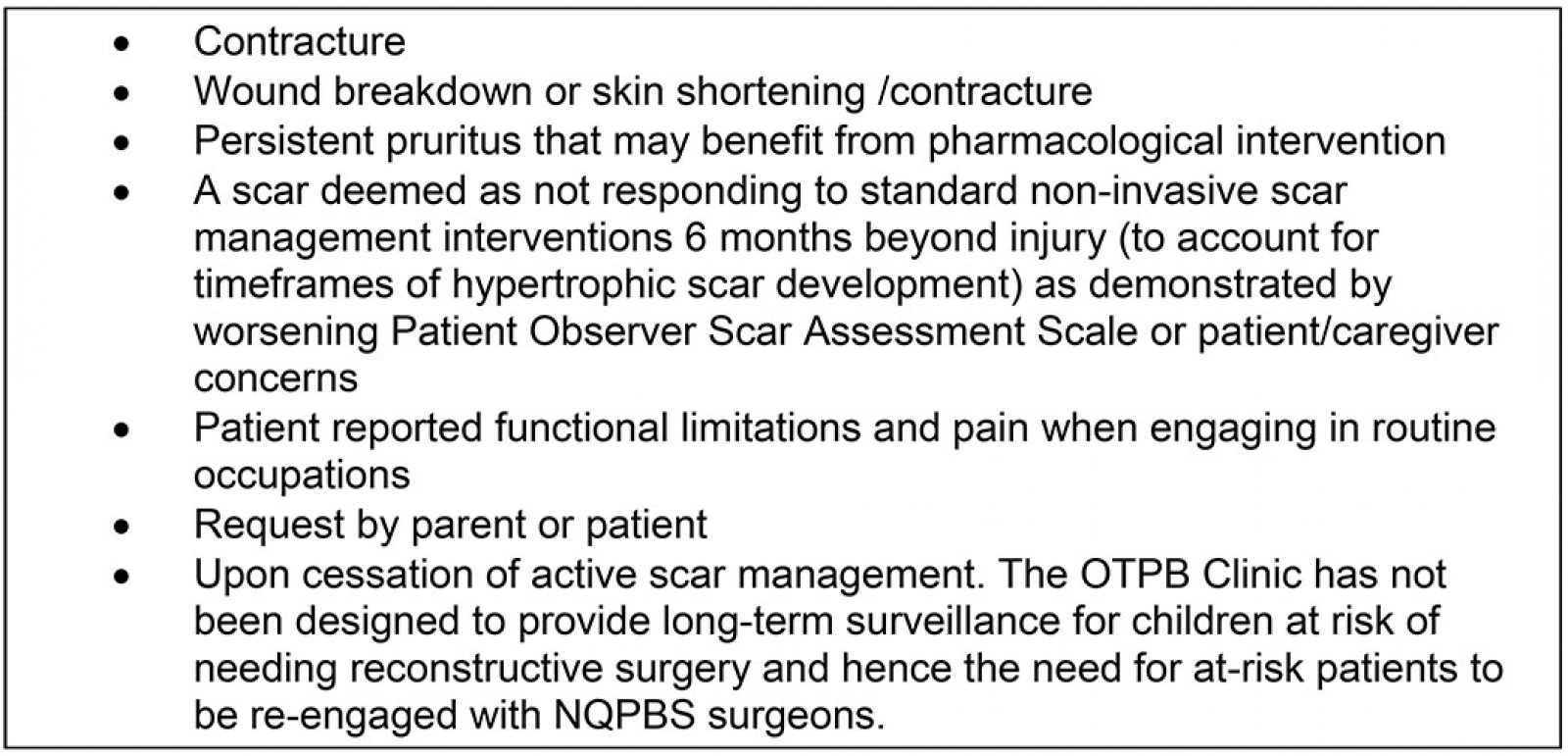
Table 3: Tasks performed by community occupational therapist or delegated to alternative health professional to assist Occupational Therapist-Led Paediatric Burn Telehealth Review Clinic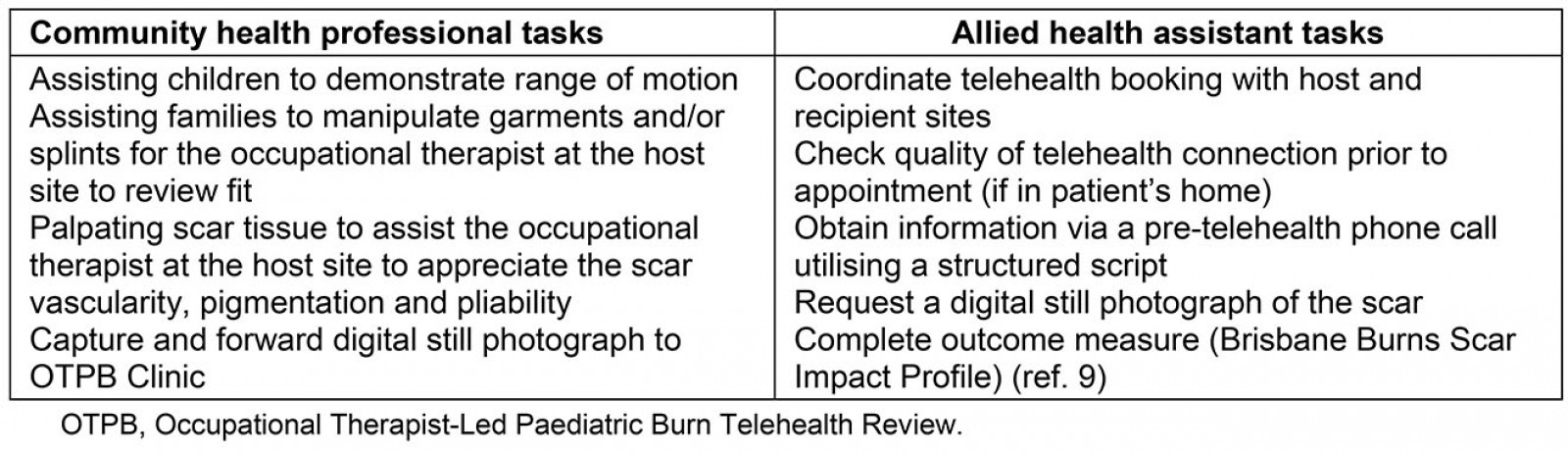
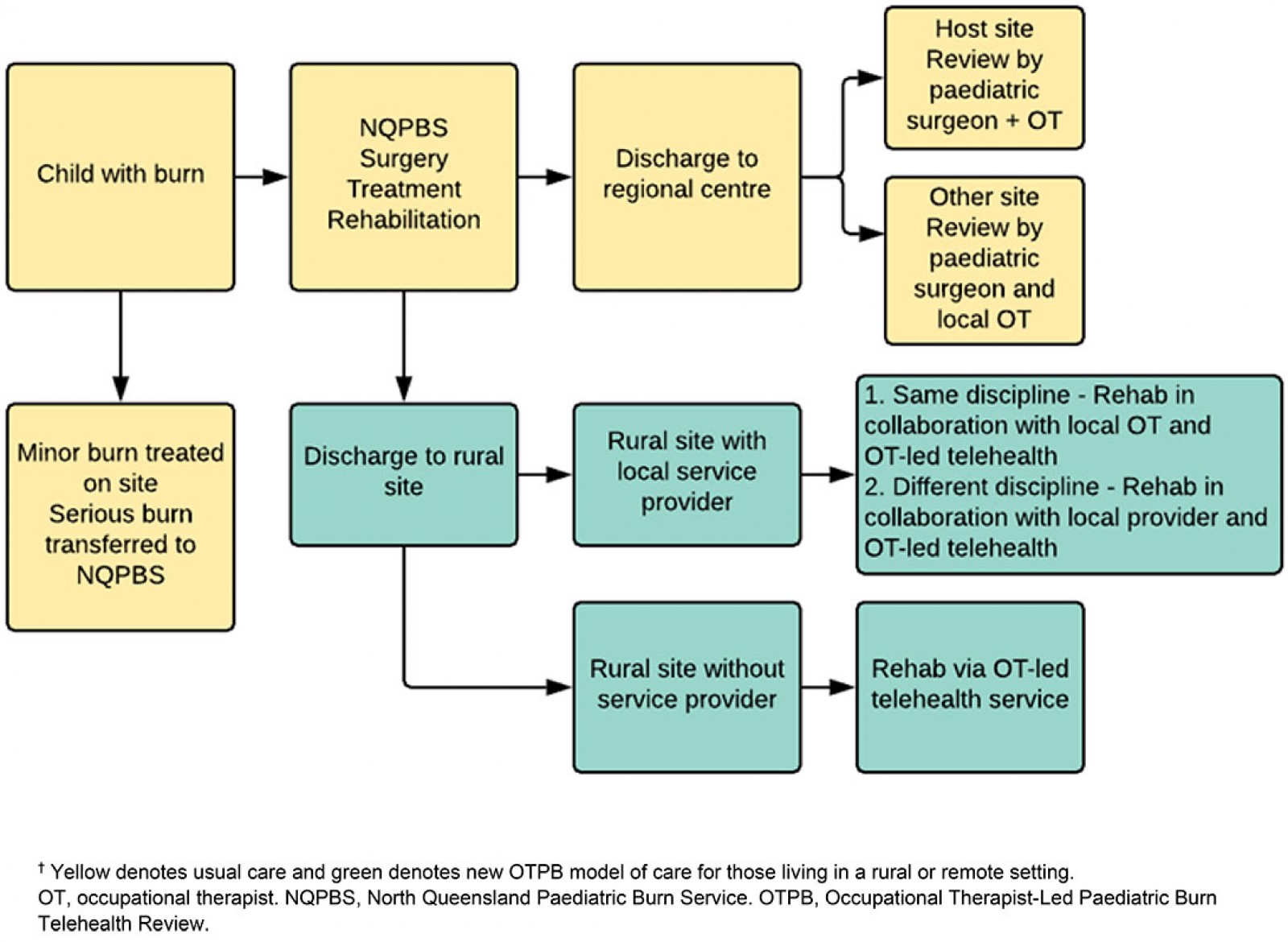 Figure 1: Model-of-care pathway for children with burns in northern Queensland.†
Figure 1: Model-of-care pathway for children with burns in northern Queensland.†
Ethics approval
Evaluation of this model of care was endorsed by the Townsville Hospital and Health Service Human Research Ethics Committee (reference number HREC/17/QTHS/147).
Lessons learned
A concurrent evaluation was planned alongside the development of the clinic. Quantitative and qualitative data were collected to measure effectiveness and acceptability of the OTPB Clinic. Data were collected by the project officer via the integrated electronic medical record (ieMR), and a survey specifically designed for this service evaluation was conducted by an AHA.
Twenty-eight children attended the clinic between January and June 2017. Each child received between one and three consultations for a total of 76 occasions of service for the period. Children from rural and remote settings were reviewed on average every 8 weeks during the trial phase, representing a substantial increase from the period prior to the introduction of the service. The OT led the clinic, which meant that 76 occasions of service were released for the paediatric surgeon to see other children on the waiting list. A median travel time of 12 hours per consultation was saved for the families. Travel time savings were calculated from the published duration of commercial transport, drive times when commercial transport was not available or a combination of both, depending on the location of the patient.
Survey responses completed by families involved in the trial phase were positive. The survey consisted of 17 questions, including open questions asking respondents to state advantages and disadvantages of the new model of care. Advantages included time saved, added convenience because of not travelling to TUH for appointments, reduced need for caregivers to take time off work, and children did not miss school. Families valued the continuity of having the same knowledgeable therapist involved for the duration of their child’s care, positive interactions between the child and therapist, and the support local clinicians received during the reviews. Disadvantages included difficulty in assessing the thickness of the child’s scar when compared to a face-to-face appointment.
During the trial period, one child required surgical review (<4% of patients). Re-engagement of the child to the paediatric surgeon was initiated by the OT performing the OTPB Clinic review as per clinical criteria for re-engagement.
There are numerous benefits to the OTPB Clinic model. It embraces multidisciplinary collaboration and integrated care across the continuum to aid recovery and improve outcomes16 by including rural clinicians in the telehealth review where possible. By delegating tasks to an AHA, the OT was able to work successfully in an expanded scope role17. Additional benefits are likely to accrue to patients and the health service18 because of reduced transport costs19. Despite the demonstrated benefits, further evaluation of the OTPB Clinic is recommended. A larger evaluation incorporating more participants and multiple sites would provide greater insight into the success of the model. An evaluation of the access, cost and outcomes of children undergoing burns rehabilitation through the OTPB clinic is planned. A qualitative research study is underway to explore the experiences of families and clinicians who have interfaced with the OTPB Clinic.
In summary, a new model of care has been developed for the follow-up of rural and remote children after burn injury via telehealth. The model includes an expanded scope role for the OT, freeing up appointments for paediatric surgeons to see patients on their waiting lists. To date the model has successfully increased the frequency of follow-up appointments for rural and remote paediatric patients and is well received by families, and rural and remote health service staff. This model can be translated to tertiary burn services in other health services.
Acknowledgements
Funding from the Allied Health Professions Office of Queensland supported planning, implementation and evaluation of the OTPB Clinic at TUH.
References
You might also be interested in:
2013 - Retraction

