The rehabilitation of elderly people can contribute to both enhancing their activities of daily living (ADL) and the individual’s realization of their actual improvement1. An aging society influences which conditions patients admitted to hospitals have, and more people are being admitted to hospital with various complications and frailty, thereby changing the demands on rehabilitation2. Elderly people’s backgrounds vary, and rehabilitation should be tailored to each patient’s needs3. As in young people, optimal nutrition and early intervention with rehabilitation are vital to prevent a deterioration in ADL2,4. The preservation of ADL during hospitalization is critical because elderly people tend to lose their ADL more quickly and take more time to regain previous ADL levels than younger patients5. The effects of aging on the lives of older people in rural societies are more pronounced than on those people in urban areas because of the lack of healthcare resources, such as the number of healthcare professionals, medical institutions and care facilities that can accommodate and support them temporarily at home6. As rural older people have to sustain their ADL, rehabilitation can contribute to rural elderly patients’ discharge to home after hospitalization for various causes.
The quality of rehabilitation can vary between urban and rural contexts because of differences in medical resources. In urban areas, specialized rehabilitation hospitals ensure a high quality of rehabilitation that improves the ADL of admitted elderly patients with heart failure and stroke. Effective collaboration between different specialized urban hospitals drives the smooth treatment and discharge of elderly patients to their homes7-9. On the other hand, rural community hospitals have to provide various treatments, such as acute therapy, rehabilitation, and transitional care under one roof because of a lack of medical resources. There are few studies on the effectiveness of rehabilitation at rural hospitals in general, and a lack of evidence on the effectiveness of such rehabilitation in enabling home care6,10. Consequently, the effectiveness of rural rehabilitation in facilitating home care has to be questioned.
The quality of rural community hospital rehabilitation is vital for aging societies, especially in Japan. The need for sustainable home care and palliative care is high in rural Japan11,12. Improvement in their ADL can facilitate elderly people’s living at home and enable the continuity of home care13,14. Both motor and cognitive factors of ADL have been studied in urban settings, and the results varied15-17. Various social conditions and norms, such as faster aging and the increasing number of nuclear families, may make continuity of home care difficult. The aims for their ADL should be discussed in relation to the background of rural elderly people, such as their living conditions and previous dependency levels on others. After considering these factors, the requirements for improvement in ADL to enable discharge to home will allow the setting of exact goals of rehabilitation, and the degree to which they are achieved may predict discharge to an elderly person’s home.
The authors’ question was, ‘Do improvements of the cognitive and motor factors of ADL in rural elderly patients through rehabilitation contribute to their discharge to home?’ Previous studies have shown evidence of the effectiveness of rural and home-based rehabilitation in the discharge to home18,19. However, the factors focusing on ADL related to discharge to home, especially among the elderly, have not been clarified in rural communities. Investigating the effects of the improvement of ADL on discharge to home in rural community hospitals can not only drive adequate provision of rehabilitation in rural settings, but also inform and guide how to improve the efficacy of rehabilitation in better resourced settings.
The purpose of this study was to clarify whether the improvement of ADL as per the functional independence measure (FIM) can enable elderly hospitalized patients to be discharged to their homes in a rural community.
Methods
Design
This was a retrospective cohort study based on medical file reviews.
Setting
Unnan city is one of the most rural cities in Japan, located in the south-east of the Shimane Prefecture. In 2020, the total population of Unnan was 37 638 (18 145 males and 19 492 females), with 39% aged over 65 years, which is expected to reach 50% by 2025. There are 16 clinics, 12 home care stations, 3 visiting nurse stations and only 1 public hospital (Unnan City Hospital). The hospital staff comprises 27 physicians, 197 nurses, 7 pharmacists, 15 clinical technicians, 37 therapists (22 physical therapists, 12 occupational therapists and 3 speech therapists), 4 nutritionists and 34 clerks20. There was no other medical institution with a recovery rehabilitation unit.
Recovery rehabilitation unit
The recovery rehabilitation unit of Unnan City Hospital had 30 rehabilitation beds during the time of the study. The unit accommodated patients motivated to return home after their rehabilitation. The underlying diseases requiring rehabilitation were mainly in the field of internal medicine and orthopedics. Individual patients and their family settings were discussed by a physician and a chief nurse, who were charged with the recovery rehabilitation unit. The decision to move from acute care to the recovery rehabilitation unit was taken collaboratively. Rehabilitation was performed on average twice per day (60–90 minutes per session) by physical and occupational therapists. If the patient had swallowing and speaking problems, speech therapists were included. The discharge timing and place were decided based on discussions among patients, their families and one specific team consisting of the charged physician and nurse, and social workers. The team was specialized for the discussion of the support and decision-making for patient discharge.
Participants
Patients aged over 65 years admitted to Unnan City Hospital with acute diseases and transferred to the rehabilitation unit were eligible for participation in this study. All consecutive patients who were admitted during the 4 years from 1 April 2016 to 31 March 2020 were included in this study.
Measurements
Patient information was extracted from the electronic medical records kept at Unnan City Hospital. Age, sex, body mass index (BMI), serum albumin as an indicator of nutrition status, reasons for admission (diagnosis on admission), number of medications (including antidepressants and sleeping medicine) for the assessment of polypharmacy, the Charlson Comorbidity Index (CCI) calculated from the patient’s medical histories (the score of which shows the severity of the patient’s medical conditions21), living conditions (with families or alone) before admission for the assessment of the abilities of care12,13,16, duration of disease from the onset of symptoms to the start of rehabilitation, duration of rehabilitation, care level based on the Japanese long-term insurance system (numbered from 1 to 5, where 1 is ‘least dependent’, 5 is ‘severely dependent’), cognitive and motor components of the FIM at both admission and discharge (measured by therapists as an indicator of patients’ ADL), change in these components of the FIM between admission and discharge, and place to which patients were discharged (home or facility) were recorded. Patients’ reasons for admission were categorized as orthopedic, internal or surgical disease.
Two groups of patients were distinguished based on their discharge to home or to a facility.
Statistical analysis
The student’s t-test was performed on parametric data, and the Mann–Whitney U-test was performed on nonparametric data. Based on previous studies and the average of variables, numerical variables were dichotomized as follows: CCI (≥5 and <5) 21, care level (≥3 and <3) based on the burden on caregivers and families22. A logistic regression model was used to assess whether discharge to home as opposed to a facility was associated with age, sex, BMI, albumin levels, care levels, the CCI, duration of disease from the onset of symptoms to the start of rehabilitation, duration of rehabilitation, and the cognitive and motor components of the FIM before rehabilitation and at discharge, as the covariates were chosen based on the previous studies, which showed the factors related to the discharge to home15,16,18,19. The variables with statistically significant differences in the logistic regression were further analyzed to calculate sensitivity, specificity and likelihood ratio for predicting discharge to home with describing the area under the curve (AUC). Cases with missing data were eliminated from the analysis. Statistical significance was defined as a p<0.05. All statistical analysis was performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (R Foundation; http://www.r-project.org).
Ethics approval
Anonymity and confidentiality of patients’ information were ensured. They and their families were informed about the usage of their clinical data in studies in this hospital and for publication, and informed consent was acquired. The research information was posted on the website of the hospital without any information about patients. The contact information of the representative of the hospital was listed there, such that it was possible to answer any questions about this research at any time. All procedures of this study were performed in compliance with the Declaration of Helsinki and its later amendments. The Unnan City Hospital Clinical Ethics Committee approved the study protocol (no. 20200023).
Results
Participant demographics of the participants
Figure 1 shows a flowchart of the study population selection process. Between 1 April 2016 and 31 March 2020, 951 patients were admitted to the rehabilitation unit. Among them, 845 were aged >65 years. Sixty-two patients were excluded because of death during the admission and the lack of the data regarding independent variables (Fig1).
The total number of participants was 783. The average age and male rate of the groups of discharged to home and a facility were 81.91 years and 83.12 years, and 33.5% and 39.1%, respectively. In the comparisons between the two groups of patients discharged to home or a facility, statistically significant differences were found for albumin levels, care levels, nature of disease, duration of disease from the onset of symptoms to starting rehabilitation duration of rehabilitation, CCI, and the two scores of the FIM (Table 1).
Table 1: Demographics and clinical characteristics of rural elderly patients in Japan undergoing rehabilitation (n=783)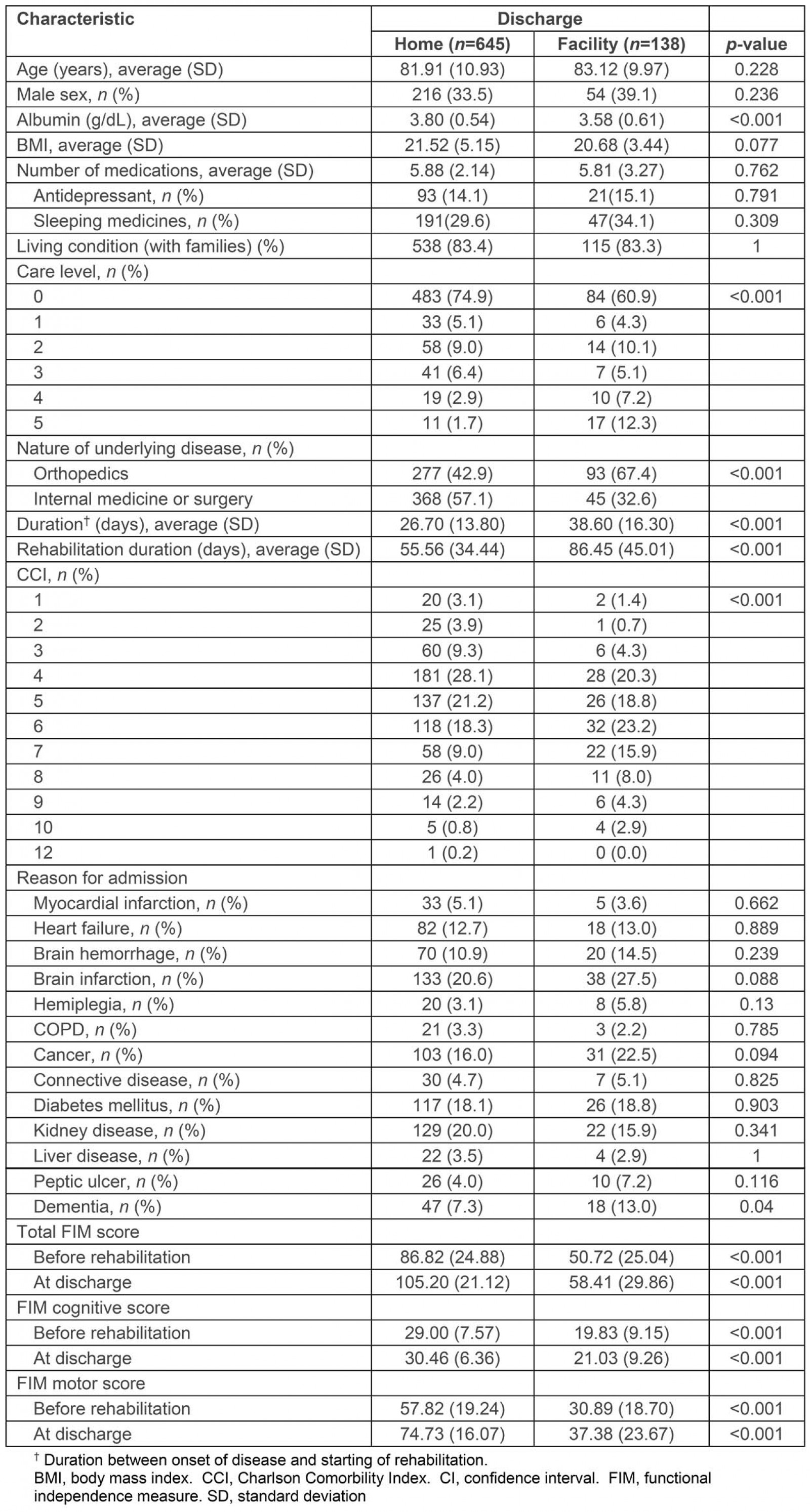
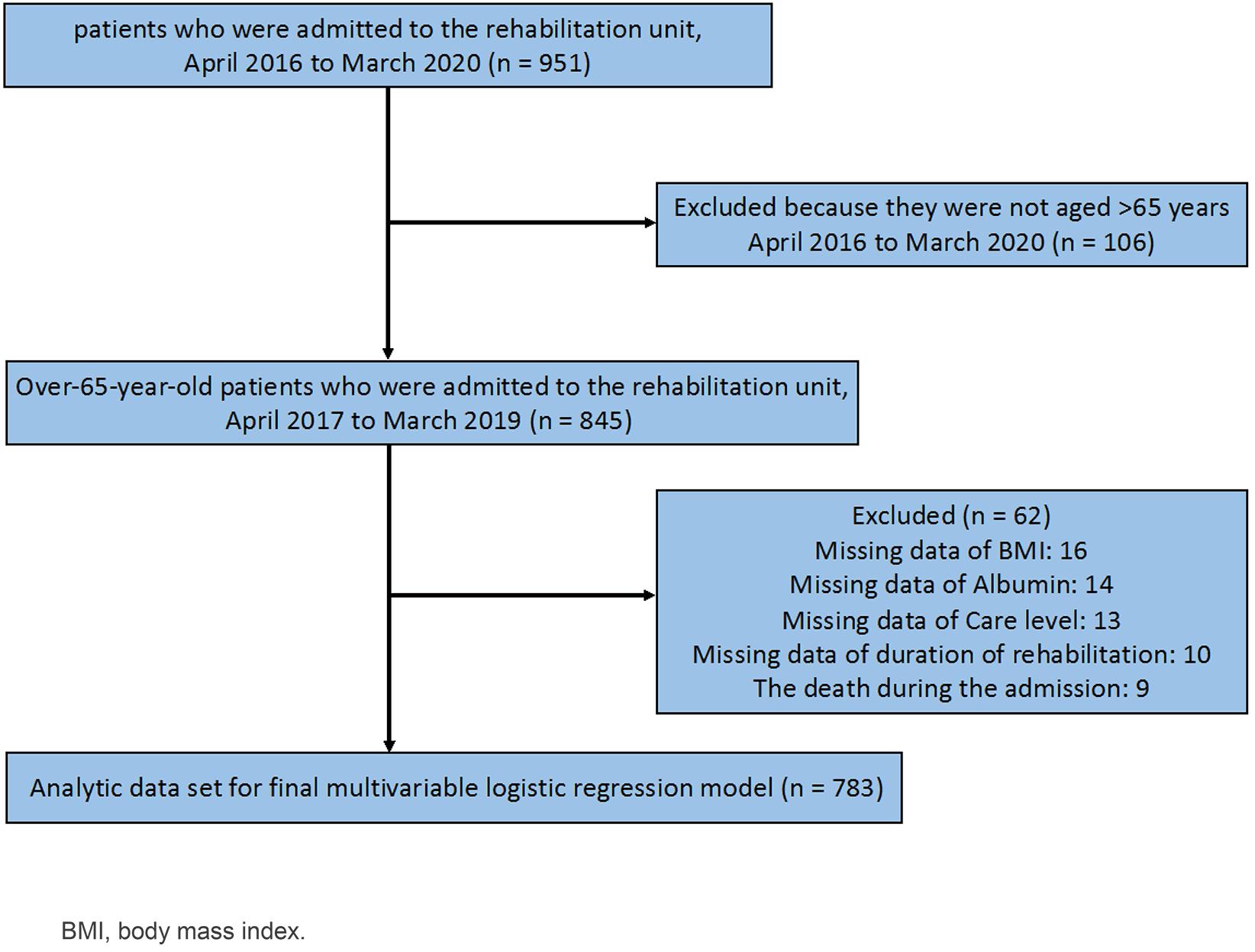 Figure 1: Flowchart of study population.
Figure 1: Flowchart of study population.
Relationship between place of discharge and patient characteristics
A high score on the motor component of the FIM after rehabilitation (odds ratio (OR) 1.07; 95%confidence interval (CI) 1.05–1.09, p<0.001) was statistically significantly associated with discharge to home. A longer duration of rehabilitation was statistically significantly associated with discharge to a facility (OR 0.99; 95%CI 0.98–1.00, p<0.001). No relation was found for the cognitive component of the FIM, and the changes in either of the scores before and after rehabilitation were not associated with discharge to home (Table 2).
The AUC for the motor FIM score after rehabilitation was 0.898 (95%CI 0.869–0.926). The AUC for duration of rehabilitation was 0.715 (95%CI 0.667–0.763). The cutoff point calculated for the motor FIM score, based on the Youden index, was 60.0 (specificity, 0.78; sensitivity, 0.86; positive likelihood ratio, 4.00). The cutoff point calculated for the duration of rehabilitation, based on the Youden index, was 66.0 (specificity, 0.37; sensitivity, 0.32; negative likelihood ratio, 1.84) (Fig2).
Table 2: Relationship between rural elderly patients’ characteristics (n=783) and discharge to home after rehabilitation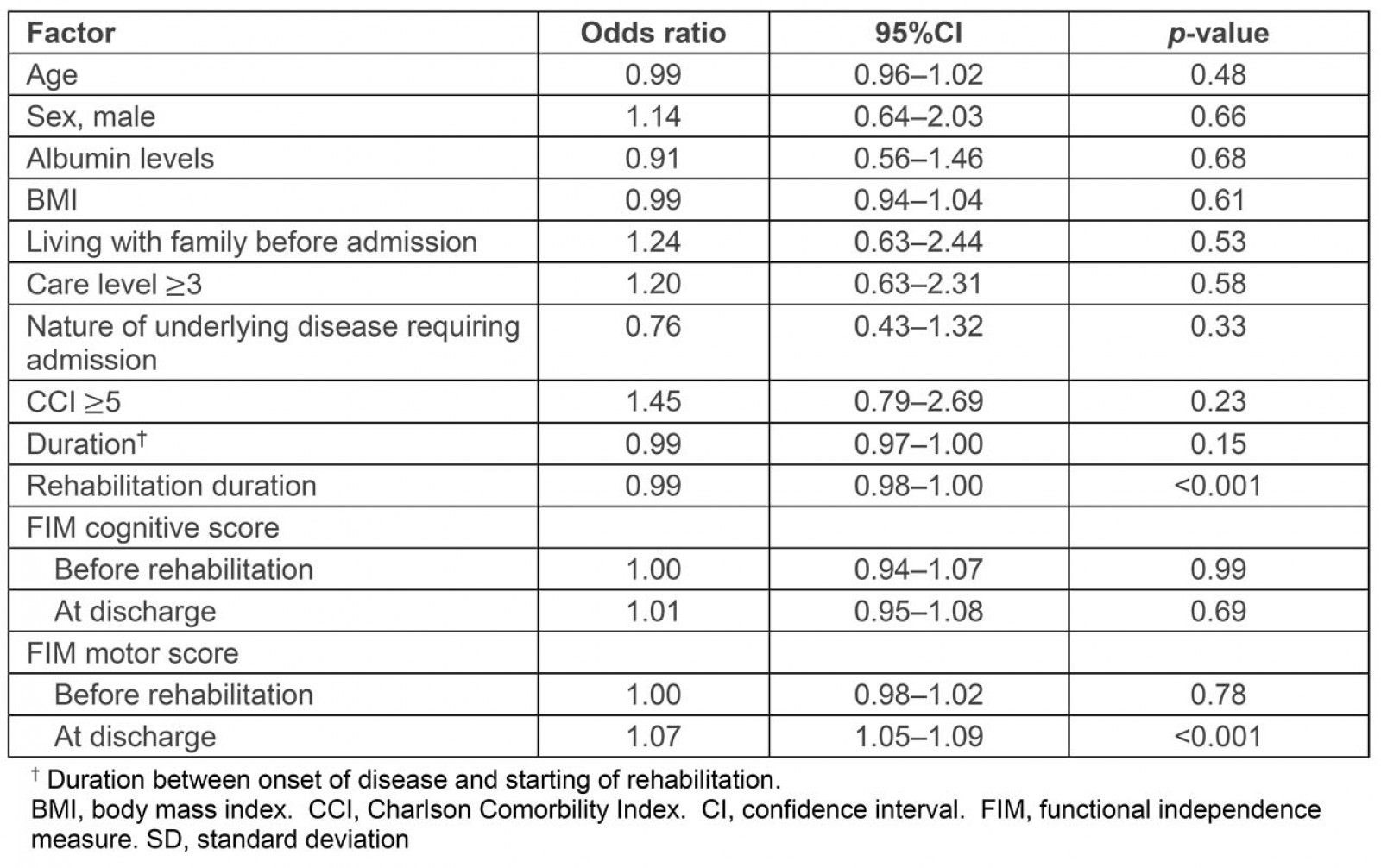
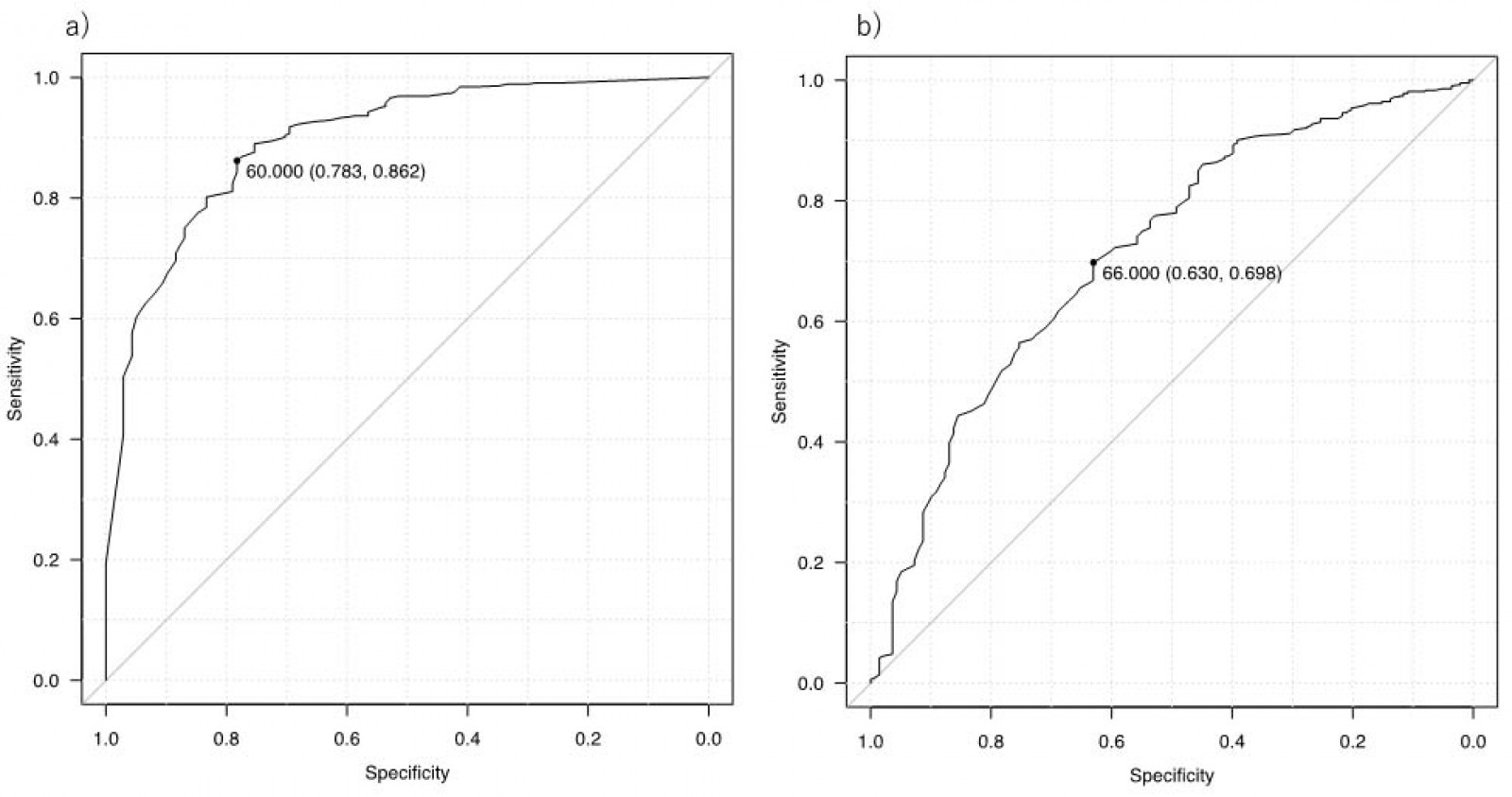 Figure 2: Area under the curve for (a) motor functional independence measure and (b) rehabilitation duration in rural elderly patients (n=783).
Figure 2: Area under the curve for (a) motor functional independence measure and (b) rehabilitation duration in rural elderly patients (n=783).
Discussion
This study showed that rehabilitation at rural hospitals may improve ADL of elderly patients as measured by the improvement of the FIM score, leading to their discharge to home. The motor component of the FIM after rehabilitation and the duration of intervention of rehabilitation were related to discharge to home, whereas none of the other variables, including the cognitive component of the FIM, previous living conditions, and comorbidities, was related.
This study showed the effectiveness of active rehabilitation of elderly frail patients to prepare them for living at home after discharge. Generally, frail patients have difficulties in living at home independently2. In rural areas, there are often problems in people’s home designs. As their homes were constructed when they were young, the setup may not fit their present physical capabilities and may limit their independent living at home12. Rural healthcare resources are limited, resulting in elderly patients not being supported appropriately by home-care physicians and workers23. According to previous studies, elderly people’s poor nutritional status, low cognitive functions, and multimorbidity may hinder discharge to their homes24-26. This study showed that these factors do not have to be an obstacle to discharge to home, which should encourage healthcare professionals to support the rehabilitation of elderly frail patients to enable home care in rural areas.
Furthermore, the results demonstrated that the post-rehabilitation motor FIM is critical in enabling discharge to home in rural patients. The duration of the rehabilitation also played a role. For living at home, elderly people need various motor functions supporting their ADL, which can be enhanced by a short period of rehabilitation27. Cognitive functions also affect the ability of elderly patients to live at home and manage their daily lives. Previous studies have suggested that cognitive impairment affects the continuity of home care in elderly patients28. In this study, even though the average cognitive FIM score was lower in patients discharged to facilities, logistic regression analysis did not show a statistically significant relationship. The lack of a statistically significant relationship between discharge to home and the cognitive FIM score may be explained by the specific sociocultural setting in rural areas12,29. People in rural areas tend to have a strong desire to die in their homes, surrounded by their relatives. Although society has changed, and such desire may have weakened lately, the preference for home care remains strong. Additionally, living at home in rural areas does not require complex cognitive functions such as structure of homes and relationship with others, which may enable the elderly with low cognitive function to live at home30. In the rural population, motor FIM improvement enabled elderly frail patients with cognitive dysfunction to be discharged to their homes. The following study questions the cognitive function requirement differences between rural and urban areas for the elderly to live in their homes.
Another finding of this study was that the effect of rehabilitation was independent of the biosocial circumstances. Living at home has been related to elderly people’s dependence on living with their families and multimorbidity in previous studies31. This study did not find any statistically significant relationships between discharge to home and patients’ living conditions and medical histories. Multimorbidity mainly assesses the number of diseases but does not consider the severity31. Currently, rural elderly in the rehabilitation unit have mild symptoms because medical staff, the patient and their families estimated the discharge to home with the timing of unit transmission. In addition, the social support from neighbors in rural areas can enable the elderly to live at home32. Social capital, cultivated as an effective relationship with neighbors in rural communities, can improve the quality of life among elderly people33. This aspect cannot be conclusive in the aspect of social capital and social support, which can be investigated in future research. The findings of this study suggest that elderly frail patients with various social backgrounds can be discharged to their homes after active rehabilitation34. However, this research did not investigate patients’ and their families’ perceptions of living at home and their desire to return home. Patients’ preferences to return home can affect their motivation for rehabilitation35. Future research should examine the perspectives of not only the elderly patients but also their families.
One of the limitations of this study was that the cause and effect relationship between home discharge and independent variables was not investigated. Future research should include prospective cohort and interventional studies to establish the relationship between discharge to home and related factors such as the FIM, nutritional conditions, and comorbidities. Additionally, this study did not investigate the relationship between precise categories of medicine and diseases, and the discharge to home. Other limitations are external validity and reliability. This study was performed at a rural community hospital, which could lead to less external validity. However, all consecutive patients who underwent rehabilitation were followed up over a period of 4 years and the setting was described in depth to show how the results may be applied. Other rural community hospitals may have comparable settings. The decision-making of discharge was based on the discussion between the patient and their families, and the discharge team without specific assessment of abilities to care in homes. This may potentially lead to less reliability. Future studies should investigate the relationship between discharge to home and multimorbidity and polypharmacy. Furthermore, more investigations are needed towards rehabilitation programs at multiple community hospitals to improve external validity and reliability for patients’ discharge. The investigation of abilities to care in home in rural settings should be progressed.
Conclusion
This study showed that elderly patients’ improvement of motor skills might predict the likelihood of their discharge to home in a rural setting. Rehabilitation can be effective in rural elderly patients with frailty and multimorbidity. The improvement in physical abilities was more important than cognitive function improvement to enable discharge to home. By respecting patients’ and their families’ desires, effective rehabilitation may enable elderly patients to live at home.
References
You might also be interested in:
2022 - COVID-19 fosters social accountability in medical education

