Introduction
Maternal mortality is disproportionally high in low-income countries, where almost all (99%) of the global pregnancy and childbirth-related deaths occur1,2. Effective antenatal care (ANC) reduces maternal morbidity and mortality both directly and indirectly, through the detection and treatment of pregnancy-related complications, provision of health education, and promotion of the use of future pregnancy-related healthcare services3-6. For this reason, in 2016 WHO recommended that women attend a minimum of eight ANC visits per pregnancy4. Nevertheless, it remains challenging for women in many low- and middle-income countries to meet even the previous global target of four ANC visits7. For instance, between 2011 and 2016, only 52% of women in sub-Saharan Africa attended the recommended four ANC visits7. Furthermore, within countries, there are inequities in ANC attendance across social and geographical gradients: women in the highest income quintile are more likely to attend ANC than those in the lowest income quintile, and urban women are more likely to attend ANC than rural women7,8.
In response, recent research has focused on addressing the inequities in ANC access and attendance, particularly in sub-Saharan Africa6,9. Recent reviews have identified several barriers to ANC attendance in sub-Saharan Africa, including health service fees, transport cost and availability, spousal and social support, distance to health centre, previous experience with health care, cultural beliefs, and gender norms10-12. Research is limited, however, on the ANC experiences of women across social and geographical gradients in East Africa, particularly for Indigenous women13,14. This research gap is striking, as Indigenous women experience higher maternal mortality and morbidity globally, coupled with substantial inequities in healthcare access, and lower maternal health services use compared to non-Indigenous women15-17.
Given the complex yet poorly understood factors that affect ANC attendance patterns among Indigenous communities in East Africa, the goals of this study were to: (1) characterise ANC attendance patterns at a hospital established to serve the local Indigenous population; and (2) identify and characterise the factors influencing ANC attendance among Bakiga and Indigenous Batwa women in Kanungu District, south-western Uganda.
Methods
Kanungu District, south-western Uganda
Kanungu District is located in south-western Uganda (Fig1). The population of Kanungu District is nearly 250 000 people, approximately 800 of whom are Indigenous Batwa18,19. The Batwa of Kanungu District are distinct peoples who have resided in the forests of central Africa for more than 6000 years, and self-identify as Indigenous and are recognised as Indigenous both locally as well as internationally by the United Nations. The creation of the Bwindi Impenetrable National Park in 1991 led to the forced and uncompensated eviction and relocation of the Batwa population in Uganda20. As a result, the Batwa were forced to transition from their hunting and gathering livelihoods and culture, to settled agriculturalists19,21. Compared to the national Ugandan average, the Batwa have lower life expectancies, and higher rates of child mortality, malaria, acute gastrointestinal illness, and food insecurity19,21,22. Relative to the Bakiga in the District, the Indigenous Batwa have less access to food, employment, shelter, safe water, and sanitation infrastructure19,21. The Bakiga population relies mainly on subsistence farming and local employment surrounding the gorilla trekking tourism industry23.
In response to these health inequities, in 2003 the Bwindi Community Hospital (BCH) was established to provide health services to the Batwa. BCH now provides comprehensive hospital services to a catchment area of 100 000 individuals, both Batwa and Bakiga. BCH aims to provide affordable and accessible health care through its community health insurance program, eQuality (introduced in 2010), with subsidised fees for Batwa patients24. The BCH Maternity and Family Planning department serves more than 250 patients monthly, providing ANC, health education, complication screening for high-risk patients, delivery services, and a Mothers’ Waiting Hostel that provides in-hospital accommodation for women awaiting delivery25. Between 2012 and 2017, a total of 3197 women delivered at BCH, 1% of whom were Batwa, which approximately correlates with the proportion of Batwa within the BCH catchment area26.
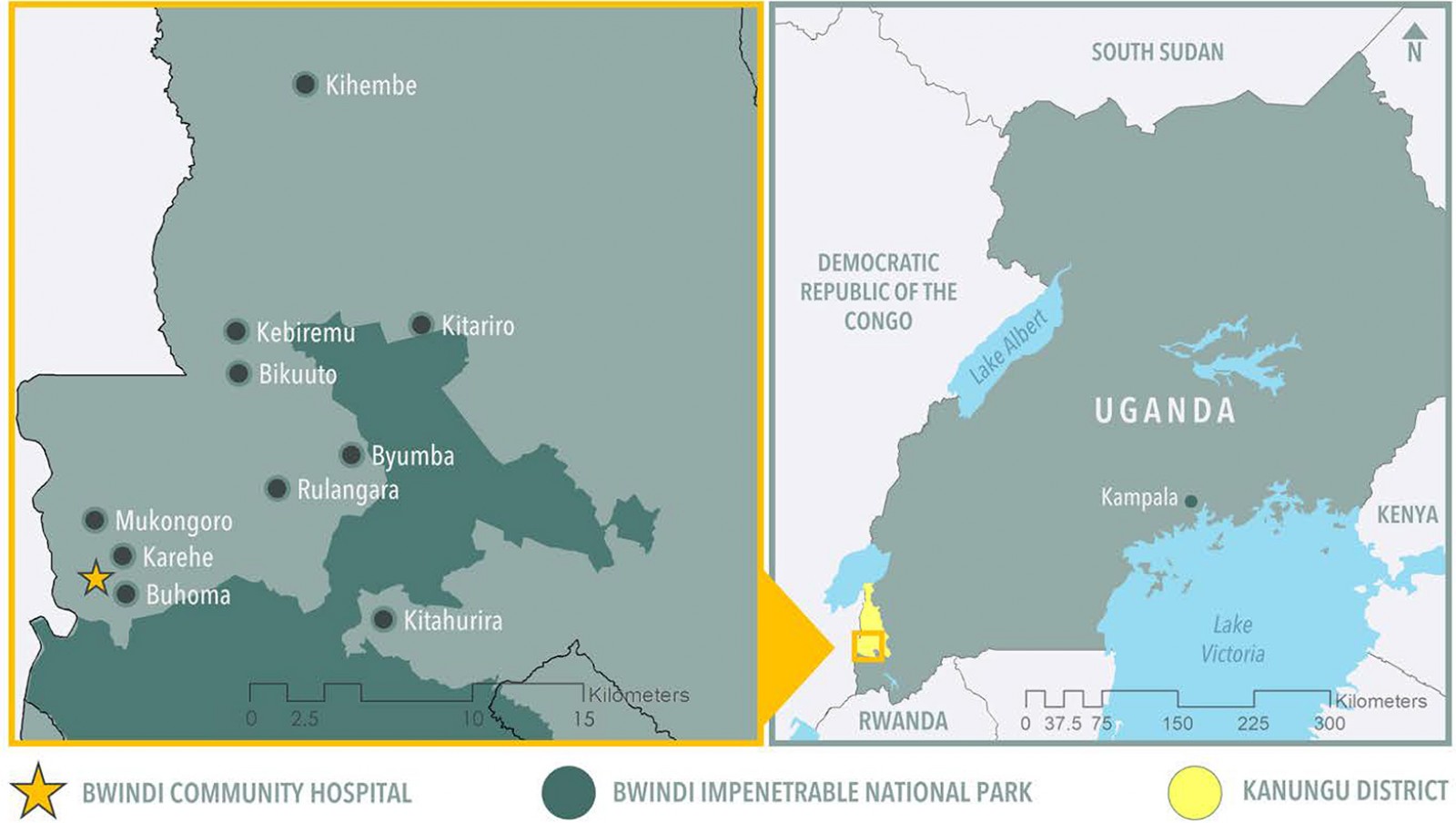 Figure 1: Map of communities in Bwindi Region, Kanungu District, south-western Uganda.
Figure 1: Map of communities in Bwindi Region, Kanungu District, south-western Uganda.
Research approach
This research was guided by a collaborative, community-based27 and ecohealth approach28, which integrated principles of participation, gender and social equity, and transdisciplinarity. BCH, the Batwa Development Programme, Makerere University, the Ugandan Ministry of Health, local researchers, and Batwa and Bakiga communities contributed to developing the research questions, study design, data collection, and interpretation of results.
Data collection and analysis
By following a concurrent triangulation mixed-methods study design, quantitative and qualitative data were jointly analysed and interpreted to understand the factors influencing Batwa and Bakiga ANC attendance29. A mixed-methods approach was employed because it is recognised as the most suitable way to contextualise patient experiences and understand the complexities of healthcare delivery, particularly within a global health context30,31.
Quantitative data collection and analysis: One year of ANC records (April 2013 – March 2014) was obtained from BCH and entered in Microsoft Excel spreadsheets. Data from ANC health records included information on patient age, subcounty of residence, visit date, gravidity (the number of previous pregnancies), parity (number of births to a fetus with a gestational age of 24 weeks or more), estimated delivery date, and gestational age.
Data from health records were imported into Stata v14.2 (StataCorp; https://www.stata.com) for analysis. The outcome variable of interest was whether a woman attended four or more ANC visits, which reflected WHO’s global recommendation for ANC attendance at the time of the study4. A multivariable logistic regression model was built to identify how demographic factors and maternal health history were associated with attending four or more ANC visits. Data on Batwa identity were not available; thus, quantitative data were not stratified by Batwa and Bakiga. First, univariable logistic analyses were performed to examine unconditional associations; independent variables with a p<0.2 were considered for inclusion in the multivariable model. The assumption of linearity was visually assessed by plotting continuous variables against the log-odds of the outcome by using locally weighted scatterplot smoothing. Independent variables that did not have a linear relationship with the outcome were categorised on the basis of biological plausibility. Based on the subcounty of residence, patients were classified as living at a distance close to, medium or far from BCH based on geolocation from the Human Rights Focus database32 and cross-referenced with the national map data33. Key informants from the region participated in the creation of these distance classification cut-offs and confirmed that they were appropriate. Collinearity was evaluated using Spearman’s rank correlation, with a cut-off of ρ=|0.80|34. The multivariable logistic regression model was built by using an iterative process: confounding was assessed by examining changes in the model coefficients, and likelihood ratio tests were performed to assess whether the full and reduced models were significantly different. The final model was evaluated for fit by using Pearson’s chi-squared goodness of fit test, and residuals were visually assessed34.
Qualitative data collection and analysis: Qualitative key informant interviews (KIIs) and focus group discussions (FGDs) were conducted from June to August 2015 in Kanungu District, Uganda.
Focus group discussions A total of 16 FGDs (n=120 women) were conducted with women in Batwa and Bakiga communities, as well as women at BCH’s Mothers’ Waiting Hostel (Table 1). Community chairpersons invited women who self-identified as being or having been pregnant living in Batwa and Bakiga communities to participate in FGDs. Separate FGDs were conducted with Batwa and Bakiga women. A semi-structured discussion guide was used to ask women to share their perspectives on ANC attendance. The FGDs were conducted in Rukiga (local language) and translated into English by two local researchers who had pre-established connections with the community, alongside one Canadian-based researcher. Each FGD was audio recorded, with permission, and transcribed. The FGDs lasted a total of 661 minutes and averaged 41 minutes per FGD.
Key informant interviews Eight KIIs were conducted with healthcare providers (n=9 individuals) (Table 1). Participants were purposively sampled based on their job involving the direct provision of antenatal care. A semi-structured interview guide was used to ask healthcare providers to share their views on ANC services in the region. Interviews were conducted in the language preferred by the participant: either English or Rukiga. Each KII was audio recorded, with permission, and transcribed. The KIIs lasted a total of 344 minutes and averaged 34 minutes per interview.
Qualitative data analysis A phenomenological approach guided the qualitative data analysis35,36, to provide an in-depth and contextual picture of ANC experiences in Kanungu District. Thematic analysis using a constant comparative method was conducted to identify key themes related to ANC access37,38. This process involved writing detailed memos during and following each FGD and KII39, as well as research team meetings after each FGD and KII to facilitate preliminary analyses by discussing and critically reflecting on participant responses to interview questions40. All audio-recordings, transcripts and memos were imported into NVivo qualitative data analysis software v12.6 (QSR International; https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home) to facilitate coding and theme development. A constant comparative method was used to identify and explore codes and themes from each interview in relation to other aspects of the interview and other interviews35. Through this process, themes and codes were expanded, collapsed, refined, adapted and defined to depict, summarise and contextualise participants’ ANC perspectives and experiences37,41, and a codebook was created to establish conceptual definitions for key themes35. To ensure the authenticity of the results, researchers conducted team debriefs, detailed data audit trails, and triangulation throughout the analysis40.
Table 1: Participants involved in focus group discussions and key informant interviews regarding antenatal care conducted from June to August 2015 in Kanungu District, Uganda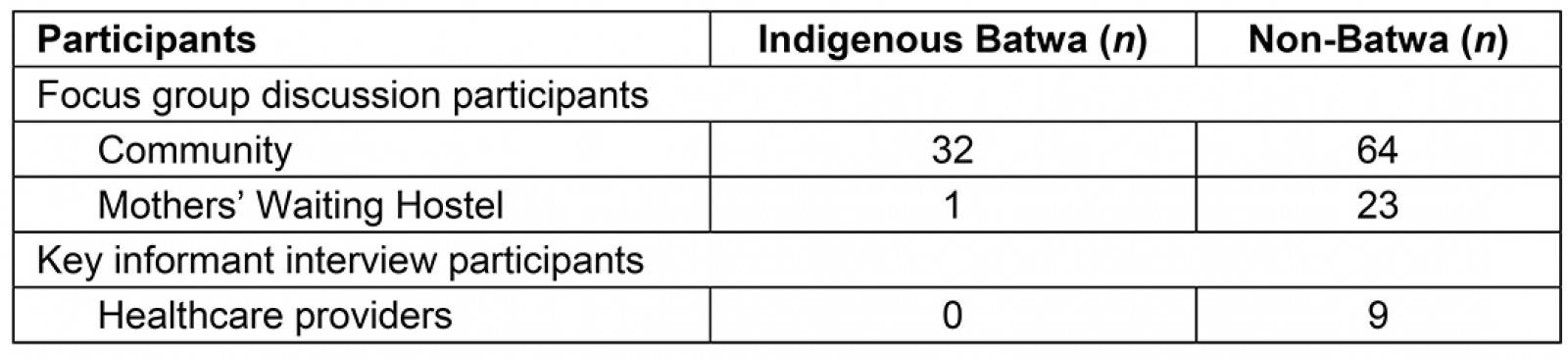
Ethics approval
McGill University and the University of Guelph Research Ethics Boards granted ethics approval for the project (REB File #461–0414). Permission to access and export health records data was approved by BCH with strict protocols to maintain confidentiality of patient information. Permission to conduct FGDs and KIIs was obtained from community chairpersons and BCH management, respectively. All participants provided informed consent to participate and audio-record the KIIs or FGDs.
Results
Most FGD and KII participants acknowledged the importance of attending ANC. As one Batwa participant described, ‘it’s good to go to the hospital so you will know how the baby is’. However, many participants felt that attending the four or more ANC visits recommended by WHO was unreasonable and/or challenging. A Bakiga woman explained, ‘they [healthcare providers] usually tell us to go for antenatal care, like, four times, and we find it’s too much’.
The hospital data reflected the sentiments expressed by women in the FGDs and KIIs. From April 2013 to March 2014, a total of 1360 patients attended ANC visits at BCH for a total of 2299 ANC visits. Most patients attended between one and three ANC visits (n=1259; 92.57%), while few participated in four or more visits (n=101; 7.43%) (Table 2). Patients’ ages ranged from 15 to 45 years, with an observed mean of 24.98 years (standard deviation (SD) 5.89). The number of previous pregnancies ranged from 1 to 17, with an observed mean of 2.95 (SD 1.96).
Throughout FGDs and KIIs, participants described numerous factors that influence ANC attendance, including distance to hospital, cost and availability of transport, ANC-related expenses, household responsibilities, spousal support, interactions with healthcare providers, traditional medicine use, advice from older women, and maternal age. These themes are explored in the following sections.
Distance to hospital was significantly associated with ANC attendance
Overall, most patients attending ANC lived relatively close to BCH (n=822; 64.98%), some lived at a medium distance (n=368; 29.09%), and few lived far (n=75; 5.92%) (Table 2). After adjusting for age and number of previous pregnancies, women who lived close to the hospital were 7.58 times (95% confidence interval 1.05–55.65) more likely to attend four or more ANC appointments during a pregnancy than women who lived far (Table 3). Participants from most communities described distance to the health centre as a major determinant of ANC attendance. As a healthcare provider explained, ‘those who are near the catchment area – they come [for more than one antenatal visit]; people who are coming from very far, they just come to have one antenatal visit’. For example, it was difficult for Batwa participants from Kihembe (a community located far from BCH) to reach BCH, for a variety of reasons, including physical distance and the increased costs of travelling long distances. As Batwa participants from Kihembe described, ‘the Bwindi Community Hospital is very far, and sometimes we can’t afford … to go to BCH when we are pregnant because we can’t walk there’.
Cost and availability of transport and poor road conditions influenced ANC attendance
Participants from FGDs reported using three modes of transport to reach the health centre for ANC: walking, taking a boda boda (local motorcycle), or hiring a car. Each mode of transport had advantages and disadvantages. Walking was challenging and time-consuming, as described by a Batwa participant: ‘if you don’t have pain from pregnancy, it can take like two hours to get to the health centre on foot, and if you have pain and you are weak, you take like three hours’. Although less physically demanding, travelling by motorcycle or car was more expensive than walking; as a Bakiga participant from Kitariro described, ‘we don’t have income, so we don’t have money to pay for a boda’. However, poor road conditions (eg rough and hilly terrain, flooding in the rainy season) were also identified as a barrier to ANC attendance; one Mothers’ Waiting Hostel participant stated, ‘most of the roads are not suitable for the boda’. The challenges posed by difficult terrain were more pronounced in the rainy season, as detailed by a healthcare provider: ‘it’s more difficult to get to the hospital during the rainy season because of the bad roads. There are a lot of floods and a lot of rocks possible on the roads’. There were no statistically significant trends in ANC visits between months or seasons (Table 2).
Financial constraints were an important barrier to ANC attendance
Batwa participants regularly highlighted ANC-related expenses as an important ANC barrier. As one Batwa woman explained, ‘we have challenges accessing the hospital when we’re pregnant because we don’t have money to go to the hospital’. The high cost of transport to get to the hospital, for instance, affected the decision to seek care. In addition to the cost of transportation, the associated costs of ANC (eg accommodation, medication, food for self while at hospital, and maternal supplies) affected attendance for many Batwa participants. Batwa participants explained, ‘what can stop me from going to antenatal care, is when I don’t have money to pay’, and ‘when we go to the hospital, the hospital needs money, yet we don’t have money. We don’t have food to eat at the hospital ... That’s why we decide to stay home’. Lack of maternity supplies required by the hospital (eg clean clothing in good condition) also limited women’s ANC attendance. As explained by a healthcare provider, ‘when they don’t have petticoats [undergarments] or they feel embarrassed when they have old petticoats or when [healthcare providers] examine them without a petticoat … it stops people from coming in for antenatal care’.
While both Batwa and Bakiga women were affected by financial constraints, Batwa women described the cost as a major and prohibitive barrier to care. Batwa women explained, ‘we are still very poor, and we can’t help ourselves’. Healthcare providers spoke generally of Batwa women’s lack of financial resources, indicating that money for ANC costs had to be spent elsewhere: ‘the Batwa don’t usually save. Most of their money is spent on eating food. So it’s bad, although we are trying to help them’.
Women’s household responsibilities limited ANC attendance
Participants explained how they were often obliged to complete home responsibilities, including manual labour for food and supervision of children. These tasks often limited ANC attendance. As one Bakiga woman explained, ‘we have got to look after the young ones at home, so that forces us to not attend antenatal care’. As a healthcare provider explained, ‘to get anything they have to go and dig. Maybe … the mother is having her ninth pregnancy, then, she has to work and get food for the other young children’.
Limited spousal involvement or support during pregnancy was common
Many Batwa and Bakiga participants described a lack of spousal support during pregnancy. Women explained that ‘the husband’s role during pregnancy is like almost nothing’; and ‘we have no support of our husbands’. According to several Batwa and Bakiga participants, many of their spouses were absent for most or all of their pregnancy, with some even leaving the house for years at a time: ‘I would not have any assistance because my husband was somewhere else’, and ‘sometimes a man leaves you with a pregnancy at one month … by the time he comes back, the child is already old. There is nothing he has helped you with’. According to FGD participants and key informants, the impact of spousal absence was more pronounced for Batwa women due to the intersectionality of being both Indigenous and an unaccompanied woman seeking medical care. Healthcare providers reported actively promoting spousal accompaniment to ANC. They reported that they advise the husbands to come to ANC ‘to help educate them both, let the husband know that the mother has been pregnant, what she’s supposed to do and not do [for a healthy pregnancy]’. But healthcare providers reported that spouses generally did not accompany their wives to ANC. As one participant described, ‘[the spouse] just takes the role of impregnating, and does not care for you, does not help you, does not advance you, nor escort you at least one day to the antenatal care’. Some women, however, reported having some spousal support during pregnancy. For instance, some Mothers’ Waiting Hostel participants had support from their spouse or other women, which allowed them to attend ANC, ‘[the children] are with their father, but sometimes they have even helpers, to stay with the kids’.
Many women described a lack of autonomy in decision-making about their health. Women explained that their spouse often had ‘final say’, not only in health-seeking decisions but in other household decisions as well (ie work during pregnancy, supervision of children, food preparation); as one women described:
… he’s making decisions about your life, and you are educated and you’re supposed to be the person who is deciding for yourself, but, traditionally, the man is having all of the authority in the home.
Interactions with healthcare providers influenced ANC attendance
Interactions with ANC healthcare providers had an impact on subsequent ANC service use for participants. Most Batwa and some Bakiga women experienced poor treatment from healthcare providers, who ‘talk to us badly’, ‘speak to us rudely’, ‘are not friendly to pregnant mothers’, and ‘shout at us’. A Bakiga participant noted that ‘when we go for antenatal, the nurses abuse us’. Of note, while Bakiga women reported a range of both positive and negative experiences seeking ANC, Batwa women almost homogeneously shared negative experiences.
Participants also described how the purpose of ANC services (eg routine testing and procedures) was not explained to patients. This reported lack of communication resulted in lack of understanding of service provision, and also generated fear, particularly among Batwa participants. One Batwa mother explained:
We used to fear going to the hospital because we had no understanding of what healthcare providers were doing. We feared to have our stomachs touched, and feared that having stomachs pressed would kill the baby.
ANC altered the use of traditional medicine and vice versa
Many Bakiga and Batwa women relied on consuming and/or applying traditional herbs collected from the forest to ensure a healthy pregnancy, but participants explained that these practices did not conform with standard pregnancy care provided at BCH. For instance, as a Bakiga participant explained:
… women fear to take traditional medicine because when you go to the hospital, the midwife and doctors usually know that you have taken traditional medicine and then they shout at you.
After their eviction from the forest, Batwa access to their traditional herbs was almost completely eliminated. According to a Batwa participant, ‘we no longer get those herbs because they chased us away from the forest’. Batwa participants, thus, expressed that their only option is to seek allopathic health care: ‘now we are out of the forest so we need to do things like the Bakiga are doing, so when they are pregnant it’s wise to go to the hospital’. Indeed, attending ANC was described as a relatively new healthcare-seeking practice for Batwa participants:
Nowadays we are going to the hospital for antenatal clinics, but in the past the services were not there and we were not aware of the importance of antenatal clinics. We would fear going because we thought … we would get abortions. But now, we are educated and know the importance of antenatal care. So, when we are pregnant, we go there.
Older women influenced younger women’s ANC-seeking behaviour
Participants reported that older women and/or mothers-in-law influenced the ANC-seeking behaviour of younger women by providing advice on traditional herb use, ANC attendance, and delivery location. According to a healthcare provider: ‘so now those are the ones considered to be the traditional knowledge bank regarding pregnancy and health’. Younger women referred to the knowledge and advice of other women in their social circle (ie mother, mother-in-law, and/or grandmother) prior to, or instead of, relying on information from health centres; as a healthcare provider described, ‘so, when a younger girl becomes pregnant, uh, the first social reference is not a health worker facility but those women who have done it before’. In many cases, it is expected that younger women follow the advice they receive from their spouse’s mother; for example, to deliver from home instead of at a health centre. Heeding the advice of other women on ANC-seeking behaviour can prevent women from attending multiple visits according to a healthcare provider:
So that [advice] ends up giving them some kind of false confidence that, the person who has been there who knows it all and then the advice they give is you can go there [ANC] once to check if everything is fine, otherwise you don’t need to.
Adolescent women experienced ANC differently
Adolescent women (10–19 years old) reported being generally unfamiliar with ANC and/or lacked confidence at ANC visits at BCH. According to a healthcare provider:
[Adolescent women] try to come, but they, it’s another group which has issues when they come for antenatal and when they come for delivery. Even when you are trying to counsel her she is like: ‘yes, yes’ to anything because she just doesn’t … have the confidence that develops later in life.
Adolescent women experienced unique challenges in pregnancy evident to healthcare providers at ANC and delivery, primarily relating to social norms around marriage and the ability to provide maternal supplies:
The young girls, when they come to deliver, they have so many social problems, they don’t have things to use, because most of them are not married. The parents are so rough on them, the girls are so stressed.
Healthcare providers expressed concern over the increased pregnancy complications associated with the high number of adolescent pregnancies at BCH (reporting that 25% of pregnant women in communities were adolescents), explaining ‘it’s a big number’. Participants also described adolescent ANC attendance as poor: ‘[adolescent women] do come to ANC, like twice’. Age was not significantly associated with the odds of attending four or more ANC appointments within the multivariable model (Table 3).
Table 2: Descriptive summary of antenatal care data from healthcare records at Bwindi Community Hospital, Uganda (April 2013 – March 2014)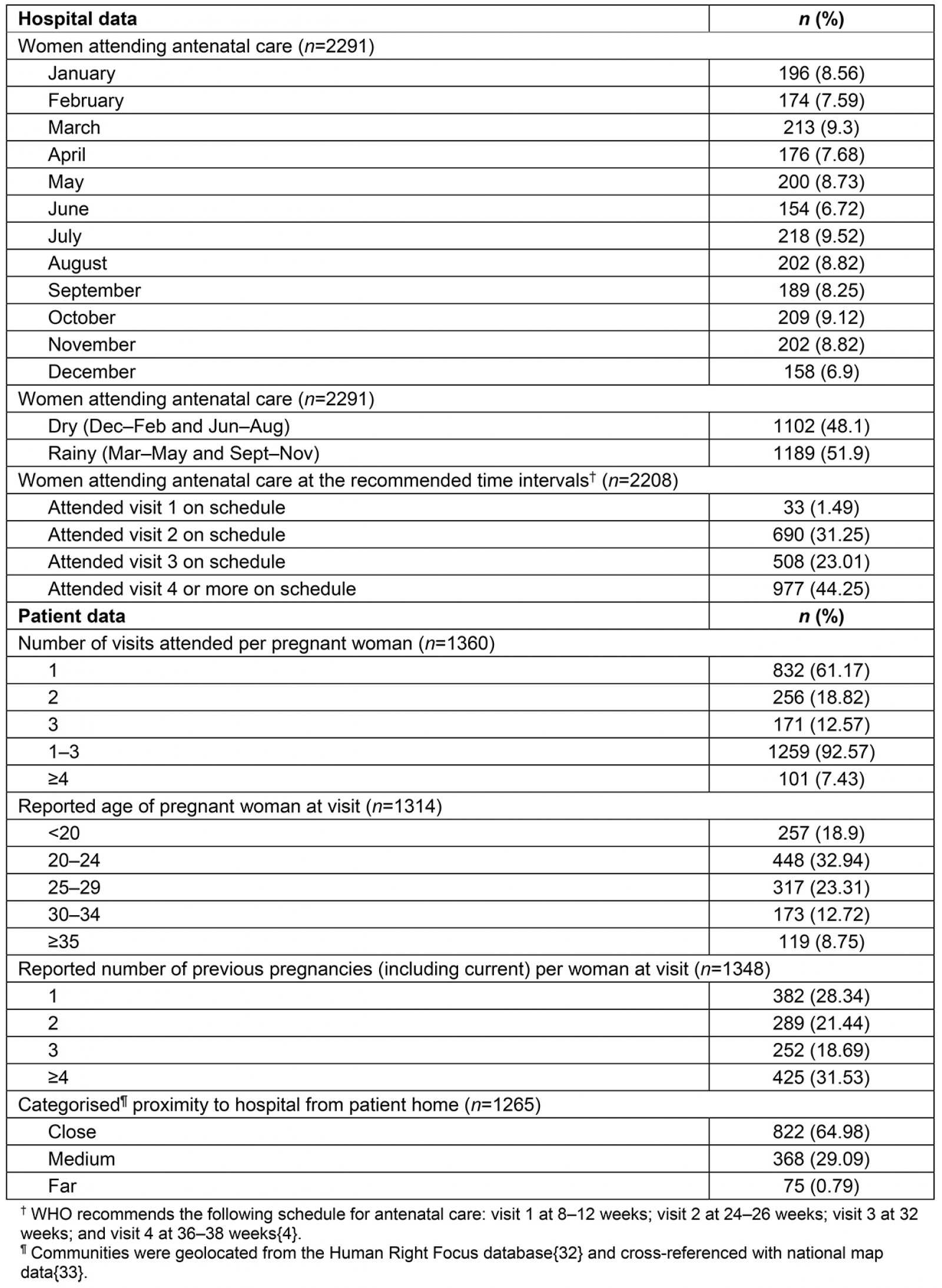
Table 3: Multivariable logistic regression results evaluating factors affecting the odds of attending four or more antenatal care visits for patients at Bwindi Community Hospital in Bwindi, south-western Uganda (April 2013 – March 2014)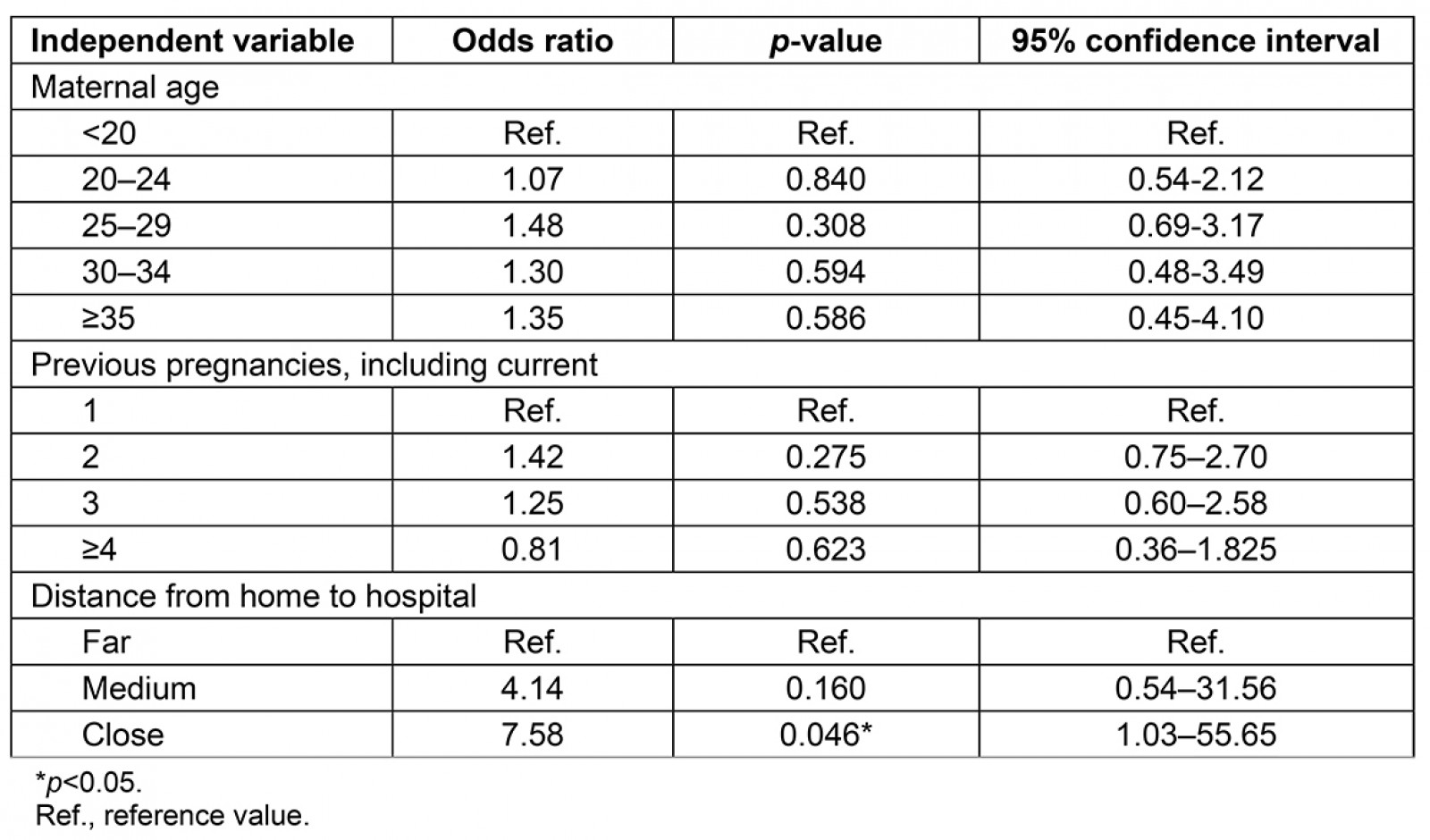
Discussion
ANC attendance levels were lower in Kanungu District than the internationally recommended four-visit minimum: only 7.43% of BCH patients attended four or more ANC visits, and most FGD and KII participants reported below-minimum attendance. This challenge is not unique to Uganda, and is prevalent across sub-Saharan Africa where only 52% of women attended four or more ANC visits between 2011 and 20167. It was evident from the qualitative results that several barriers influenced ANC access, and socioeconomic factors notably modified or exacerbated these barriers. Both Batwa and Bakiga women experienced obstacles to care, but some barriers reportedly had different, or more pronounced, effects for Indigenous women.
Both qualitative and quantitative results revealed that a long distance from a woman’s home to the health centre generally negatively influenced ANC attendance. In rural communities in Uganda, the barrier of distance to facilities is amplified by the time lost from domestic tasks, the physical burden of reaching ANC centres, and the high cost and low availability of transport42-44. Qualitative results demonstrated that in Kanungu District, no mode of transportation was universally accessible. As is the case in many rural communities in low- and middle-income countries, women are often unable to afford cars, taxis, buses and bodas to reach ANC45,46. Although travelling to ANC on foot or by bicycle are generally affordable modes of transport, the high time expenditure of both often makes a visit to a clinic for ANC impractical43,47. Further, participants from FGDs were influenced by external factors while travelling to ANC, including unpredictable weather and unreliable transport. Research from low- and middle-income countries confirms that challenging topography, poor road conditions, and seasonal changes in weather, particularly in the rainy season, hinder ANC attendance in rural regions46,48. Evidence from other rural regions of Uganda suggests there are effective interventions for improving transportation and reducing geographic inaccessibility, but these initiatives require substantial resources from the government or other sources49. In Kanungu District, an attempt by BCH to increase hospital access by implementing a motorcycle-ambulance was unsuccessful due to the difficult terrain and unpredictable weather in the catchment area. Nevertheless, qualitative results indicated that participants’ proximity to the facility or access to transport did not guarantee ANC attendance, suggesting that addressing geographic distance as the sole barrier to accessing care may not be sufficient to improve attendance in the presence of additional barriers to access48,50.
Direct (ie health centre fees) and indirect costs (eg transport costs, clothing, soap, meal purchases, labour lost and medication) were identified as important barriers to ANC; financial barriers limit attendance for women in other regions of East Africa as well51,52. Even when maternal health services are provided free or at a reduced rate, as is the case in many rural health centres in low- and middle-income countries, ANC attendance levels remain low as women must work at paid employment or subsistence activities through their pregnancies in order to afford both the direct and indirect costs of ANC53-55. Yet, women from low- and middle-income countries who work in subsistence farming, like participants in this study, earn little and struggle to accumulate sufficient savings to pay for ANC11,51.
Unmarried adolescent women in this study were reportedly less likely to seek ANC due to unfamiliarity with healthcare services, a lack of understanding of the pregnancy process, and a fear of social stigma. Global research confirms that adolescent women may experience social stigmatisation by peers, family members and healthcare providers when seeking ANC12,47,56. Indeed, despite being deemed a priority population by international organisations (eg WHO), providing appropriate ANC to adolescents remains a crucial international challenge12,13. Special programming and targeting is likely needed to meet the needs of pregnant adolescents57,58.
Beyond a woman’s individual decision to seek ANC, the realisation of her decision can be strongly influenced by her social sphere (peers, family members, spouse and community health providers)53,55,59; household responsibilities (eg child care, income earning, food provision, chores)53,60; and autonomy (ability to make independent health decisions)47,52. Although spousal support during pregnancy has been encouraged and there is evidence that it improves access to health services and ANC attendance61-63, results suggested that spousal involvement in pregnancy is uncommon. Qualitative results indicated that the impact of spousal absence was more pronounced for Batwa women, potentially providing another compounding factor that might contribute to lower ANC attendance rates.
This study has several strengths that merit mention. First, the validity of results was enhanced through the use of mixed methods, data triangulation, and member checking, which involved sharing preliminary results with community members to allow participants to verify findings and provide feedback64-66. Furthermore, by including both community members and key informants, this study captured various perspectives on factors that influence ANC attendance.
Nevertheless, this study also had some limitations. Conducting qualitative cross-language research introduces challenges that may influence a study’s accuracy67,68. An experienced local researcher was employed as a translator in an attempt to reduce these challenges65. Additionally, it was not possible to stratify quantitative data by ethnicity, as these data were not available. This information is collected in other BCH health records (eg general admissions), but was not collected by BCH for ANC records during the study period. Collecting this information for ANC attendance would be useful not only for research purposes, but also for planning, programming and policy-making69,70. Lastly, due to the nature of community-led research, many of the processes of co-analysis and co-writing take considerably longer71,72. However, while the initial data were collected in 2015, the authors have had ongoing discussions, member checking, and community input since then, as well as community co-authorship on this paper, with little to no changes reported in their experiences since then.
Conclusion
The most salient barriers to ANC access reported by participants included long distances to hospitals, high cost and low availability of transportation, ANC-related expenditures, lack of spousal support, and negative interactions with healthcare providers. The persistence of low ANC attendance levels for Batwa and Bakiga reflects a combination of poorly understood barriers to ANC access, particularly for Indigenous Batwa, as well as ongoing limitations of current health outreach programming. Additional efforts to improve access to care would benefit both Batwa and Bakiga women. Current community health programs have the potential to improve care access, but performance remains limited by several factors, including insufficient staffing and resources73. Continued efforts are also needed to increase the autonomy and decision-making power of women to improve access to health care generally and to ANC specifically. This research and further context-specific qualitative research focused on Indigenous women can inform the efforts of local health centres, such as BCH, to improve ANC attendance; for example, by increasing healthcare staff training and community outreach efforts. This research contributes to the collective body of knowledge on ANC access, and can ultimately help to enhance global efforts to achieve equitable, accessible ANC for every woman, everywhere.
Acknowledgements
The authors would like to thank Sarah MacVicar for her assistance with data collection and preliminary results sharing, Dr Kate Bishop-Williams for her help with preliminary results sharing, Carlee Wright for her creation of Figure 1, Rachael Vriezen for editing support, and Dr Birungi Mutahunga Rwamatware from BCH for his feedback on preliminary results. This research was supported by the Canadian Institutes of Health Research. The funders did not play a role in study design; data collection, analysis or interpretation; manuscript writing; or the decision to submit the article for publication.
References
You might also be interested in:
2019 - Satisfaction and limitation of primary health care nurses' work in rural areas
2015 - Obesity and obesity-related behaviors among rural and urban adults in the USA




