Introduction
The Health Resources and Services Administration of the US Department of Health and Human Services identifies and classifies health professional shortage areas (HPSAs) to mitigate healthcare accessibility and quality disparities among medically, economically, and geographically vulnerable populations. HPSA classifications identify and prioritize locations and populations with poor access to primary and preventative health services1. Often, there are overlaps in HPSAs and social determinants of health that include demographic, economic, and social factors predictive of health outcomes1.
HPSAs are identified as primary care, dental health, or mental health, and are stratified by geography, population, or facility2. A HPSA designation for a geographic area indicates a shortage in the number of specific providers per capita persons living within a defined geographic area2. HPSA designations for population groups consider specific populations within a geographical area, such as low-income members or migrant farmers. Facility designations are specific to such places as correctional facilities, state and county mental hospitals, Indian Health Service facilities, Federally Qualified Health Centers, and Certified Rural Health Clinics. Large expanses of the USA are depicted by these HPSAs3, regardless of whether a county encompasses a large urban center or not (Fig1).
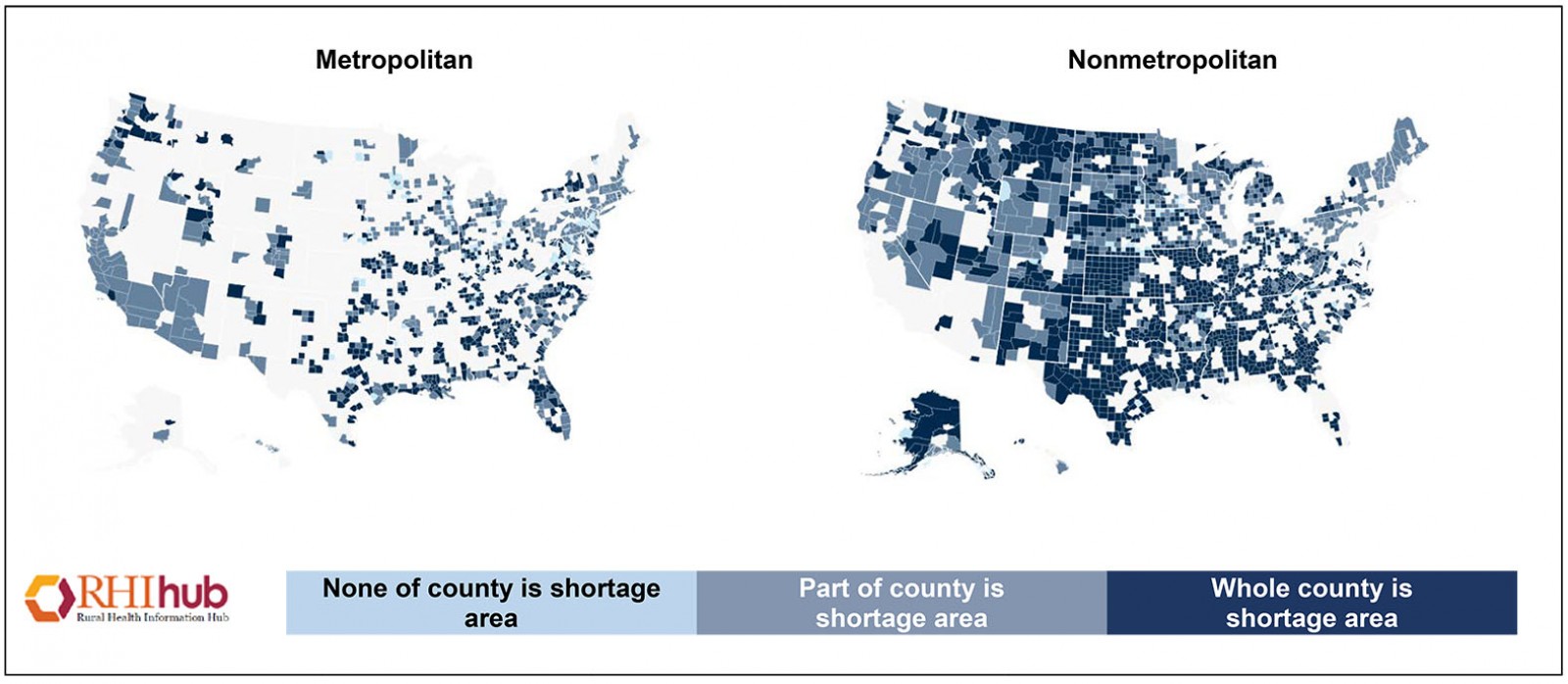 Figure 1: Health professional shortage areas: primary care, by county, 20202. (Reprinted with permission.)
Figure 1: Health professional shortage areas: primary care, by county, 20202. (Reprinted with permission.)
Rural healthcare setting recruitment and retention challenges
Healthcare provider shortages are often felt most acutely in rural areas4. Clinician recruitment and retention efforts in rural areas face unique challenges, including geography, which influence access to care and a greater amount of health disparity in comparison to urban areas5. Rural and partially rural geographic areas, population groups, and facility designations associated with primary HPSAs constitute 68% (rural 61.54%; partially rural 6.55%) of total healthcare provider shortages5.
Physical therapist (PT) shortages in rural areas are concerning, with 61.2% of rural CEOs reporting a need for PTs in their hospital/clinic systems6. The introduction in May 2019 of House Bills HR 2802 (Physical Therapist Workforce and Patient Access Act 2019) makes provisions that add PTs to the National Health Service Corps Loan Repayment Program in exchange for services provided in areas with limited access to health care. Materials distributed by individual states have also highlighted the scope of the problem. For instance, the most recently published PT workforce report from the Minnesota Department of Health7 provides geographic distribution information by rurality. For each PT located in a metropolitan area, there is a population share of 1216 people. In contrast, for each PT located in an isolated rural area, there is a population share of 2720 people7.
Strategies to recruit and retain rural healthcare professionals
Inequitable distribution of healthcare professionals between rural and non-rural communities may, in part, be addressed through purposeful hiring practices. Factors known to predict rural practice among health professionals include size of childhood town, completion of clinical education in a rural community, and older age at graduation8. Attributes of those most likely to gravitate toward accepting employment in rural communities include female gender, those with higher levels of maturity and experience, and those who embrace the positive aspects and challenges of rural healthcare provision, such as autonomy and practice diversity9. Expanding upon this appeal are flexible employment options and career development incentives9.
Healthcare workers who choose to practice in rural towns have listed community need, community size, financial aid, return to hometown, and rural training programs as important to their employment decisions8. Additional factors include the hiring of recent graduates from rural areas who specifically articulate an interest in general practice and those oriented toward service10.
Well-developed partnerships between rural clinics and educational program placement liaisons have demonstrated recruitment promise as a strategy toward augmenting the PT workforce in rural areas11,12. Health profession students who accept employment in rural areas at graduation often cite past positive experiences in these areas as well as a rural background as influential to their employment acceptance decision-making13.
Among physicians, rural field residencies highly influence the likelihood of an individual working within a rural community10. It has been shown that ongoing mentorship during student clinical affiliation experiences is a strong recruitment tool, leading new physicians into rural practice10. The long-term influence of incentives, such as scholarships, rural return of service agreements, and payment of direct financial incentives, on physicians’ choice of rural practice is less clear.
Incentives to practice in rural environments must offset professional barriers such as isolation, lack of consultant support, poor clinic infrastructures, poor locum relief, higher patient complexities, service access, overlapping roles, training constraints, and patient avoidance of care. Additional personal barriers exist, such as quality of schools, adequacy of employment options for spouse, and leisure lifestyle options6. Five factors are known to discourage medical students from accepting work in rural areas: lack of professional challenge, social segregation, sociocultural gap, hostile professional environment, and lack of financial incentives14.
On the other hand, medical graduates are more likely to accept placement in rural practice if there is a match between personal goals and career intentions15. Additional factors include lifestyle, proximity to friends and family, and employer reputation. Discouraging factors include social and geographical isolation and lack of employment opportunities for a life partner15. In general, higher retention and recruitment of healthcare workers have been associated with rural community cultures that are perceived as friendly, supportive, and healthy6.
Importance of access to physical therapy services
In 2000, the American Physical Therapy Association’s House of Delegates approved a strategic vision (Vision 2020) that included the elevation of the entry-level degree from a master’s degree to a clinical doctorate degree for all professional graduate programs by 2020. Among the incentives for elevating the degree were direct access privileges that permit PTs to practice as first-contact health professionals. Today, all 50 states, DC, and the US Virgin Islands have direct access, although provisions and restrictions vary by jurisdiction16. Granting direct access to PTs practicing in HPSAs reduces the evaluation and treatment burden among primary care professionals and situates PTs as movement specialists equipped to screen and differentially diagnose within their scope of practice. The expansion of professional roles to include PTs offers a solution that may ameliorate healthcare shortages while emphasizing quality care. Evidence shows that early access to PT saves annual healthcare costs17,18, decreases the need for prescription pain medication19, and decreases the need for outpatient physician care20. Furthermore, at a time when rural communities are disproportionately affected by the opioid crisis21, physical therapy serves a critical role in pain management22 and shows promises in helping to mitigate the abuse of prescription medications. The US Surgeon General has acknowledged that physical therapy plays an important role in changing the culture of pain management23.
Purpose
Identifying the incentives that attract PTs to underserved areas is a first approach toward utilizing PTs and addressing primary healthcare shortages. A high percentage of pcHPSAs are designated as rural. Mindful of the need for PTs in rural and underserved medical areas, insight into factors that lure PTs to rural facilities is valuable. The purpose of the current study was to examine values or incentives that differentiate PTs who accept and maintain employment in pcHPSAs and non-urban designation areas as a means of advising rural clinic employers.
Methods
The study design was a non-experimental survey of licensed PTs. Responding PTs from three West North Central region Midwestern states were email solicited through their membership in the state chapters of a national professional organization. A second set of email invitations was subsequently distributed through licensing agencies in three additional states, and participants were encouraged to expand the scope of responses through email sharing with other PTs. The invitation used an electronic survey link to collect responses. An introductory script specified that advancement through the survey was an indicator of participant consent.
Instrument
The survey comprised several demographic and practice questions as well as the Determinants of Employment Acceptance Survey (DEAS) for PTs and PT assistants (Table 1).
Table 1: Determinants of Employment Acceptance Survey† construct statements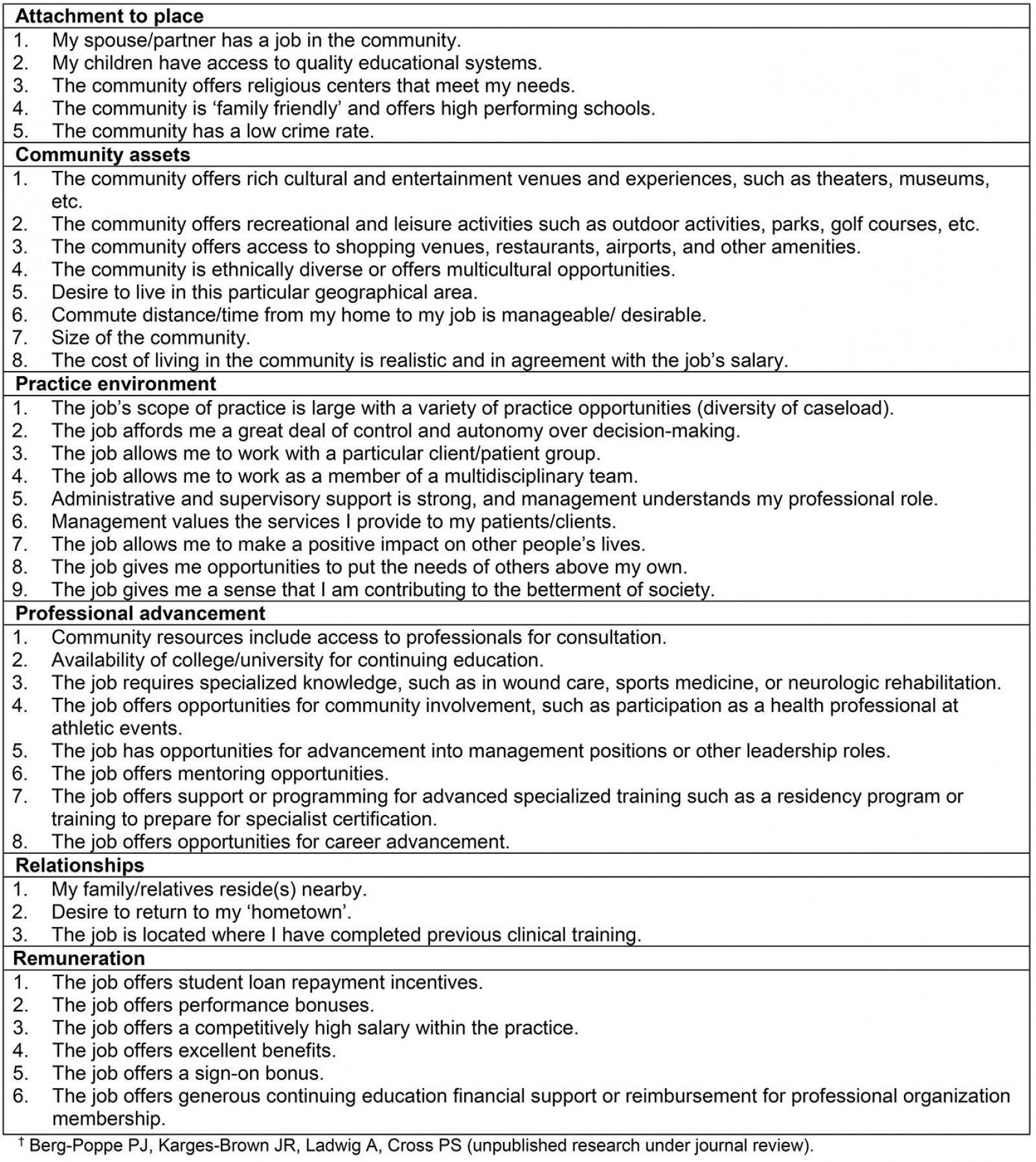
Determinants of Employment Acceptance Survey: The 39-item DEAS (Table 1) includes six component factors: attachment to place (five items), community assets (eight items), practice environment (nine items), professional advancement (eight items), relationships (three items), and remuneration (six items). The original item pool was generated through a critical review of the literature, informal focus group, and expert opinion. Face validity was improved by consultation with academic faculty and clinicians. All item statements utilized the same Likert scale with weighted values assigned to importance descriptors:
- 1: Not at all important – whether or not the job is linked to this factor would not make a difference in my decision to accept a position.
- 2: Not particularly important – if this factor were linked to the job it would be nice, but it holds limited influence over my decision to accept the position.
- 3: Important – if this factor were not linked to the job the position would be less than ideal, but it would not prohibit me from accepting the position.
- 4: Very important – if this factor were not linked to the job, I would think twice about accepting the job or remaining with the job.
- 5: Essential – this factor is so important that it is essential to any job I would accept.
Items were trimmed and clustered by fit using a principal components factor analysis. Cronbach’s alpha for the six components ranged from 0.623 to 0.786, suggesting acceptable consistency. A thorough description of this instrument’s validation is under journal review.
Data analysis
Descriptive statistics were used to profile the sample population. Reported primary practice area zip codes were used with the Am I Rural? web-based tool24 to categorize respondents as working within either a pcHPSA or a non-pcHPSA designation area and as practicing in either a non-urban (rural or urban cluster) or an urban geographical designation area. As recently as 2000, when the urban cluster concept was introduced, communities with populations fewer than 50 000 were considered non-urban/rural25. Census 2000 introduced a third category, urban clusters, defined based on the same criteria as urbanized areas but representing areas containing at least 2500 and less than 50 000 people. Rural migration has meant that health clinics serving communities of fewer than 2500 are often served through urban cluster communities that often act as a geographical buffer. For the purposes of this study, the pre-Census 2000 collapse of urban cluster and rural categories was utilized to inform the ‘non-urban’ classification25.
Because categorical variables were used to capture life experiences (eg practice setting, educational background) and practice within the areas of interest, a χ2 cross-tabs analysis was used to analyze the influence of life experience on practice in a pcHPSA. Independent t-tests were used to analyze between-group differences in DEAS component scores. Level of significance was established with α=0.05. Statistical analyses, including Cohen’s d calculations of effect sizes, were generated using SPSS v27 (IBM; https://www.ibm.com/products/spss-statistics).
Ethics approval
This study was approved by the University of South Dakota’s Institutional Review Board (2017.098).
Results
The original data set included 423 PT respondents. Fifty cases were excluded due to incomplete data sets, leaving 373 surveys for analysis. Response rates could not be accurately calculated, because dissemination methods could not capture the number of undeliverable emails and could not ascertain emails that remained unopened by intended recipients. Efforts to expand the sample through recipient sharing also limited the response rate calculation, since the total number of electronic invitations received and read could not be determined.
Demographics
Participants were primarily female (75.6%), had an average age of 41.7 years (standard deviation (SD)=11.5; range 23–72), and had practiced an average 16.1 years (SD=11.6). The most frequently reported highest degree earned was the Doctor of Physical Therapy degree (36.5%; Table 2). Thirty-two percent of respondents reported their PT educational program had a rural service mission; however, 41.3% were unsure if they graduated from a program with a rural mission. More than half (57.1%) of all respondents reported they completed at least one clinical affiliation in a non-urban25 community of 50 000 people or fewer.
Almost half of respondents reported full-time salaried positions, and the most commonly reported practice environment among respondents was health system or hospital-based outpatient facility or clinic (32.4%; Table 2). Primary areas of employment included 35.7% working in a pcHPSA and, when recategorized by urban designation, 66.6% working in an urban setting, 22.5% urban cluster, and 10.7% rural. A majority of those working in pcHPSAs worked in non-urban areas (60.5%), although this group of respondents constituted just 20.1% of the sample population (Table 3). More than half (56.5%; Table 2) of all respondents reported a primary practice region in the West North Central region of the Midwest. The average home-to-work commute time was 20.7 minutes (SD=14.7; range 0.0–85.0). The most distant site of service delivery from central work site was an average of 30.5 km (19.0 mi) away (SD=28.7; range 0.0–300.0).
Table 2: Demographic profile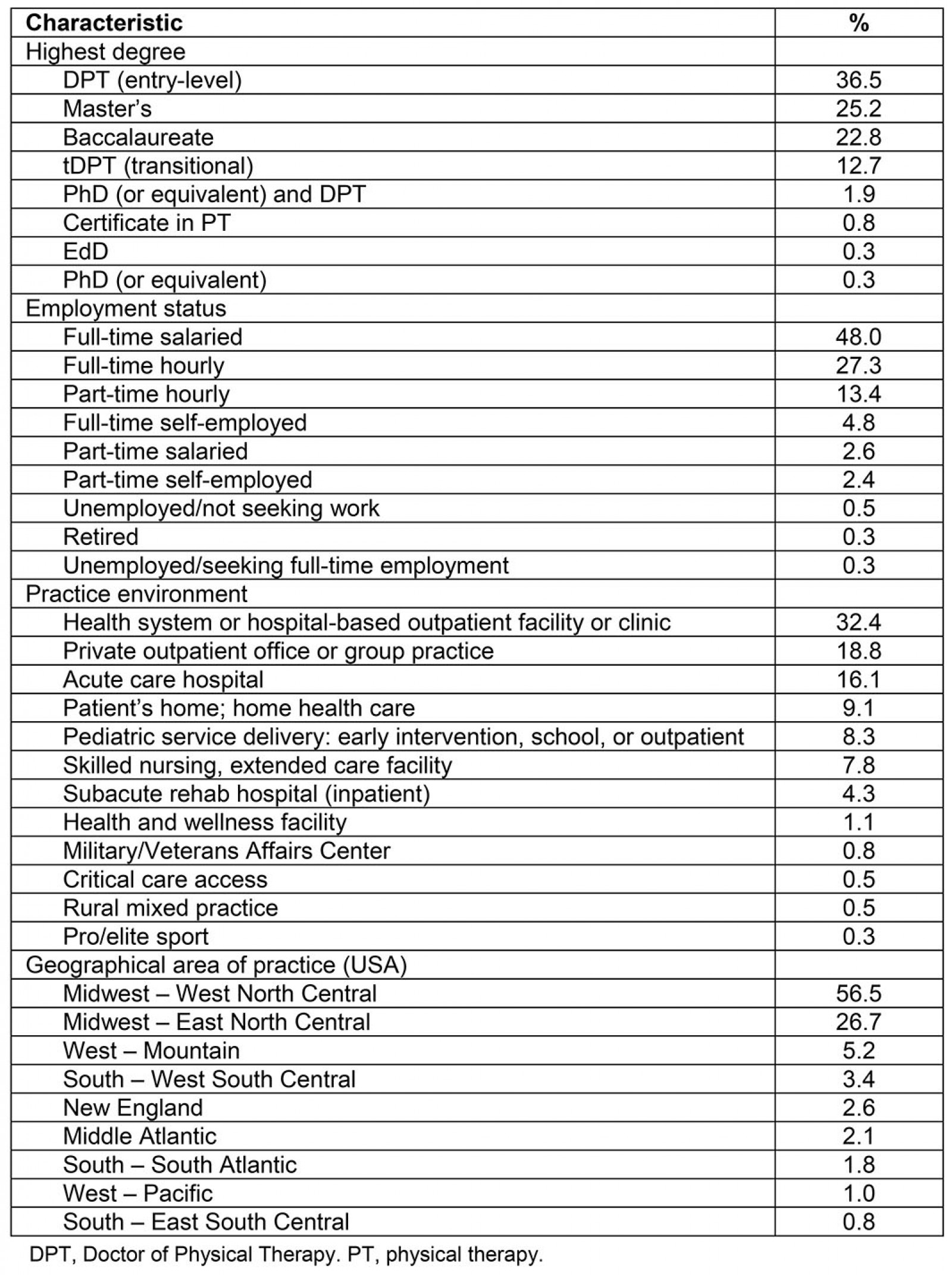
Table 3: Crossed distribution of shortage and urban designations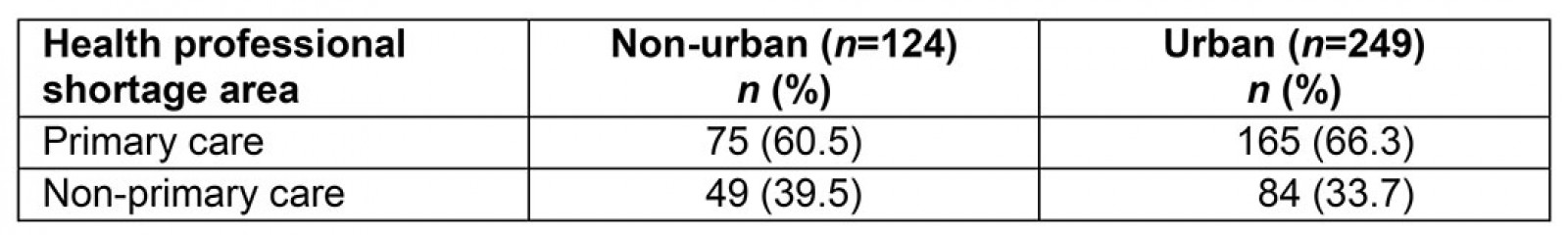
Life experiences on employment choice
Data were explored both by HPSA (non-pcHPSA v pcHPSA) and urban (non-urban v urban) designations to understand the influence of life experiences on choice of employment community. Chi-squared cross tabs showed that none of the following factors influenced a respondent’s employment choices within a pcHPSA or urban designation area:
- size of the community in which the respondent had spent the majority of his or her life
- whether the respondent graduated from a PT educational program with a rural mission
- whether the educational program was situated in a community of fewer than 50 000 people
- whether a PT educational program had rural placement requirements.
Justification for intent to leave
Most respondents (88.5%) reported they were either satisfied or extremely satisfied with their current job, with just 3.8% reporting they were either dissatisfied or extremely dissatisfied.
Respondents were asked, ‘Do you plan to leave your job within the next …’ with single-select options of 0–2 years, 3–5 years, 6–10 years, >10 years, and ‘I have no plans to leave my job’. Choices 0–2 years and 0–5 years were collapsed to create the dichotomous classifications ‘yes’ or ‘no’ for ‘intend to leave within next 5 years’ analyses. Approximately 31.1% of all respondents reported they intended to leave their current job within the next 5 years.
Primary care HPSA and urban designation within-group analyses were undertaken to understand justifications by designation. A χ2 analysis showed no significant difference in the frequency of ‘yes’ and ‘no’ responses when comparing primary non-pcHPSA and pcHPSA shortage designation area responses (χ2 [1, n=373]=1.73, p=0.19; Table 4). Similarly, when the sample was re-classified by urban designation groups, there were no significant differences in the number of reported ‘yes’ responses per sub-group (χ2 [2, n=374]=1.27, p=0.53; Table 4).
An additional multiple-selection survey item queried, ‘What is the motivation for planning to leave your job in the time frame indicated?’ The data file was split to analyze the presented justifications among respondents who reported intent to leave within the next 5 years (Table 5). Among this group, the most frequently reported reason for intent to leave was ‘better career prospects’ (31.9%), followed closely by ‘better income opportunity’ (31.0%). When split by separate analyses into either non-pcHPSAs or pcHPSAs, justifications differed, with ‘retirement’ occupying the most reported reason for pcHPSA respondents (31.9%) and the fifth-highest reason for non-pcHPSA respondents (14.5%; Table 5). There was no significant between-group difference (p=0.460, Cohen’s d=–0.080) in age among those working in pcHPSAs (median (M) =42.3, SD=11.7 years) and those in non-pcHPSAs (M=41.4, SD=11.4 years). No significant difference was detected (p=0.511, Cohen’s d=–0.071) in practice tenure between the two groups (pcHPSA M=16.6, SD=11.7 years; non-pcHPSA M=15.80, SD=11.6 years). Reported justifications among those working in non-pcHPSAs paralleled the overall sample, citing ‘better career prospects’ and ‘better income opportunity’ as reasons for resignation. For respondents of pcHPSAs, ‘retirement’ (31.9%) was followed closely by ‘better income opportunity’ (25.5%; Table 5).
The set of 116 respondents with intention to leave in the next 5 years was split by urban designation to explore these trends. When the data were reorganized by urban designation, ‘better career prospects’ and ‘better income opportunity’ emerged as the two most frequently reported justifications among both urban and non-urban respondents (Table 5).
Table 4: Change of employment against shortage and urban area designations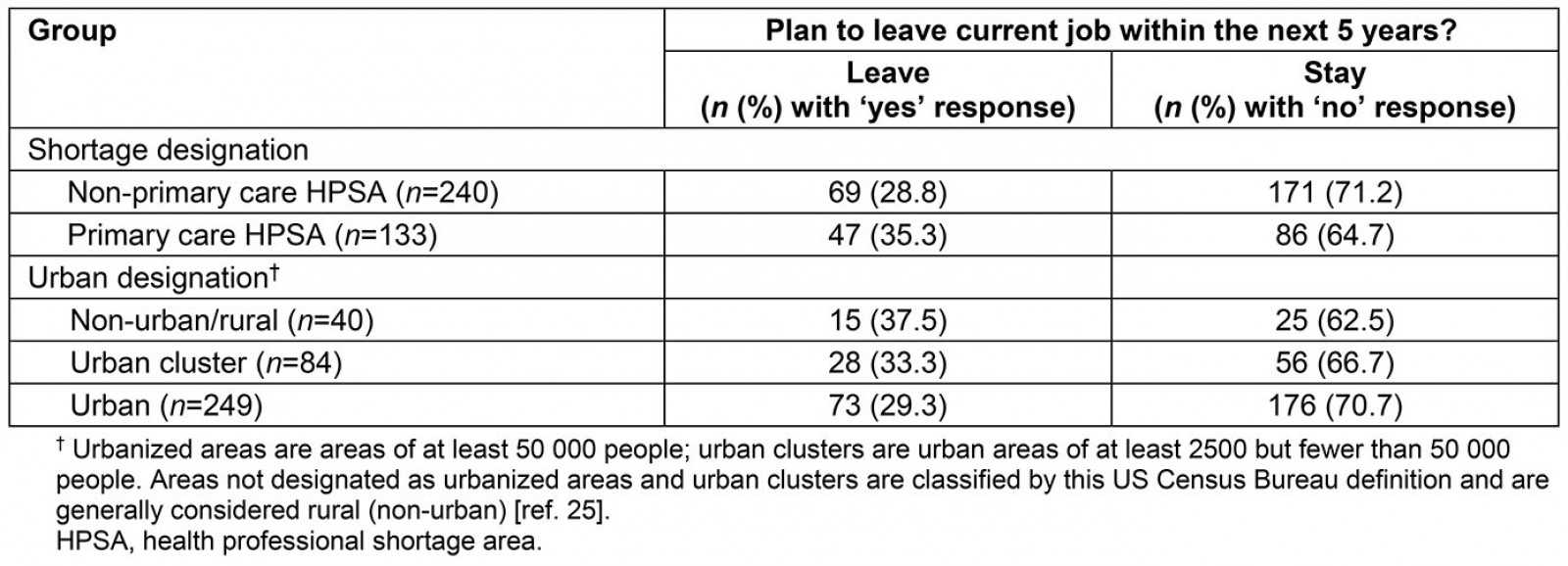
Table 5: Justification for leaving current position in next 5 years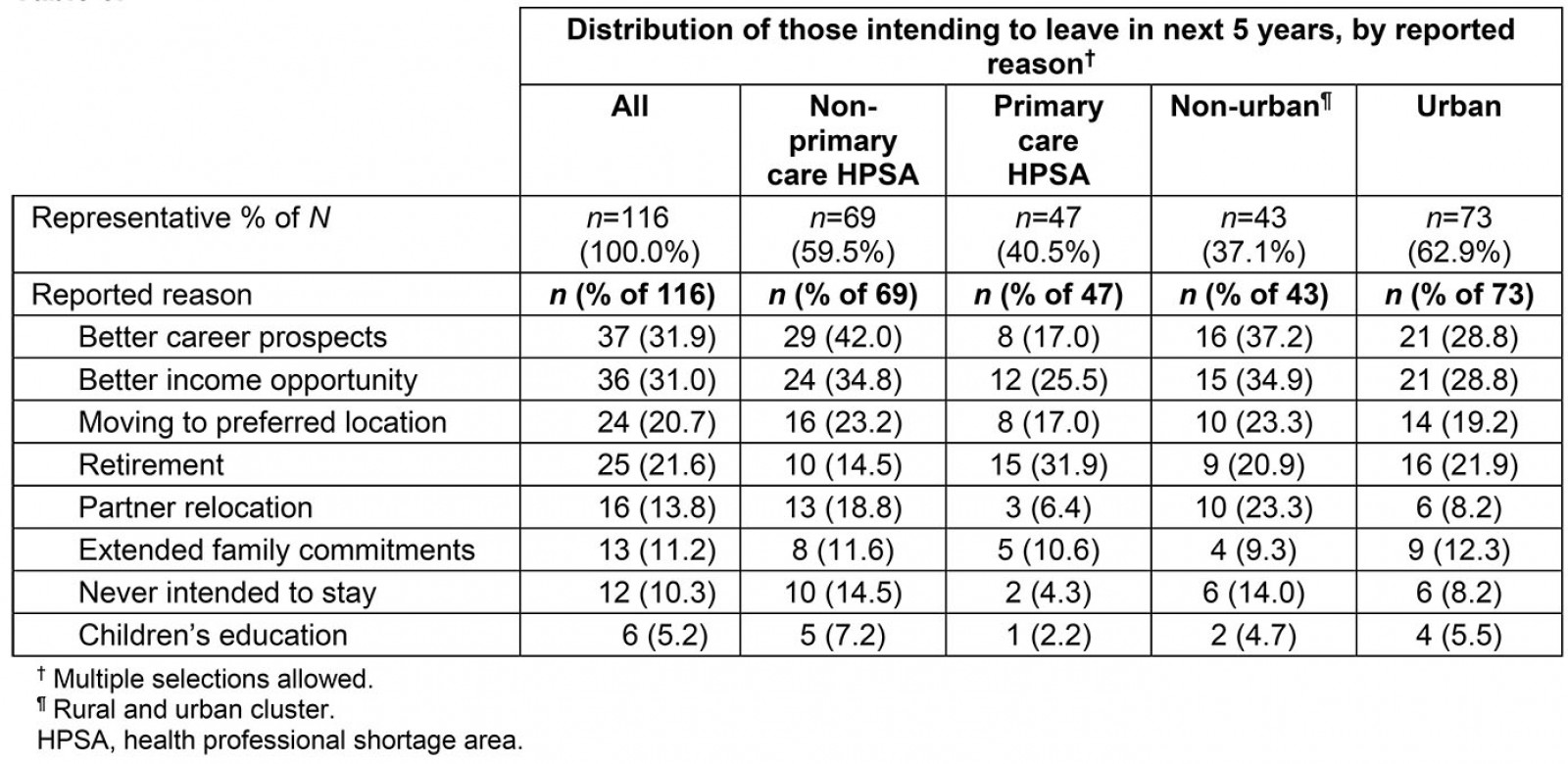
Determinants of Employment Acceptance
Determinants of Employment Acceptance components were analyzed to understand which factors discriminated respondents from pcHPSAs from non-HSPAs, as well as non-urban from urban respondents. The dataset was further reduced to examine subgroup differences between those intending to leave in the next 5 years against those who intend to stay.
Primary care HPSA versus non-primary care HPSA: Means for all six components of the DEAS were lower among respondents who work in pcHPSAs when compared to those in non-pcHPSAs (Table 6, Comparison A). Construct means for those working in a pcHPSA were significantly less for professional advancement (p=0.021, Cohen’s d=0.250), and relationships (p=0.046, Cohen’s d=0.216), alone (Table 6, Comparison A). Those who work in a pcHPSA placed lesser value on professional advancement and relationships when considering employment acceptance. While these differences were identified, the associated effect sizes were small.
The data were further split to examine the subset of pcHPSA and non-pcHPSA respondents according to whether they intended to leave or stay with their current employment situation within the next 5 years (Table 6, Subset Comparison B). Among those who worked in a pcHPSA, those who intended to stay reported significantly higher valuation of professional advancement than those intending to leave (p=0.009). This difference is approaching a medium effect size (Cohen’s d=–0.483). Among those working in non-pcHPSAs, attachment to place was more highly valued (p=0.019, Cohen’s d=–0.336) among those intending to stay, while remuneration was more highly valued (p=0.050, Cohen’s d=0.281) among those who intend to leave (Table 6, Subset Comparison B). These effects were small.
Table 6: Determinants of Employment Acceptance by shortage designation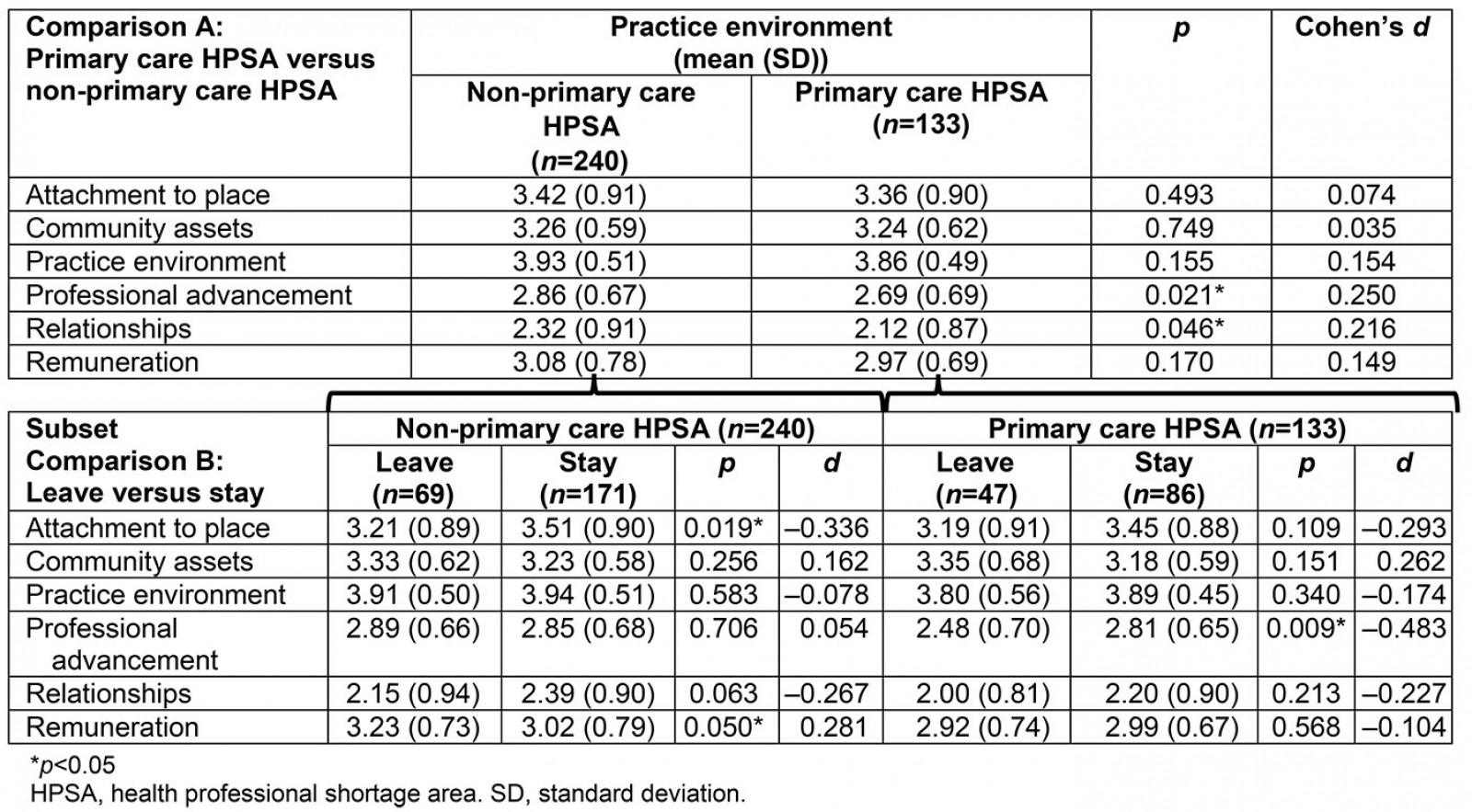
Non-urban versus urban: A second, repeated analysis reconfigured the sample by urban designation. Significant differences seen between those from pcHPSAs versus non-pcHPSAs no longer held true; there were no significant differences in DEAS constructs when comparing non-urban and urban designations. However, when the sample was reduced to subsets, those who worked in non-urban areas and planned to leave valued community assets significantly higher than those intending to stay (p=0.005), with a medium effect size (Cohen’s d=0.541; Table 7, Subset Comparison B). Among urban respondents, those intending to stay valued attachment to place significantly higher than those planning to leave (p=0.006), with a small observable effect (Cohen’s d=–0.387; Table 7, Subset Comparison B).
Table 7: Determinants of Employment Acceptance by urban designation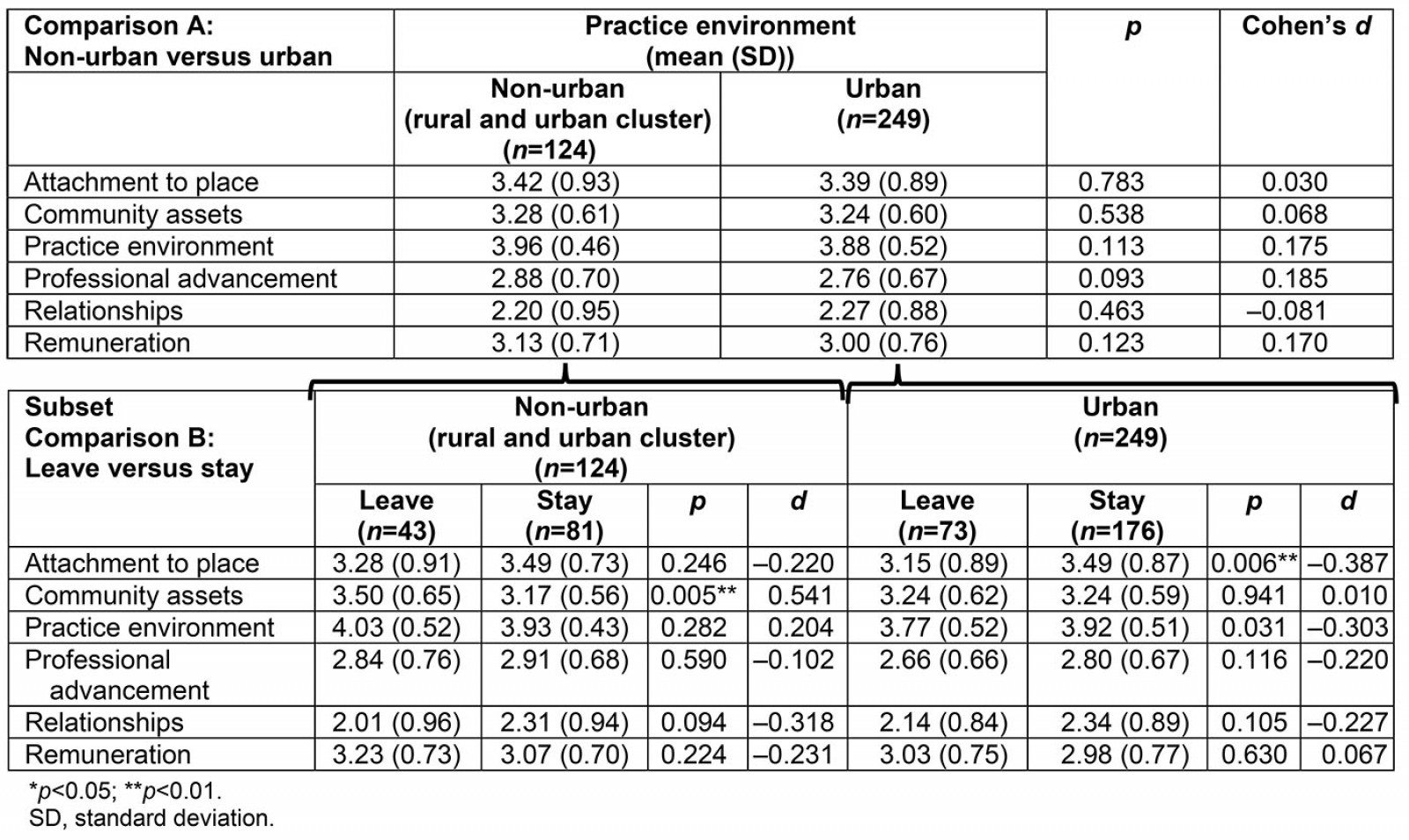
Discussion
Lack of adequate PT coverage is not an issue unique to the USA. Recruiting PTs into underserved and rural shortage areas is a global challenge. A recent WHO report emphasized that ‘a comprehensive strategy is required to strengthen rehabilitation and address global unmet needs’ (p. 1)26. Those concerned with health disparities impacted by professional shortages and, more specifically, those who recruit these professionals, should be particularly mindful of factors that contribute to employment acceptance among PTs. An understanding of these factors can bolster marketing that is tailored to the unique assets of a geographical region or social milieu and can incentivize interest among desirable hires.
In the USA, as providers with direct access privileges, PTs are uniquely positioned to ameliorate primary care shortages by serving as first-contact professionals within their scope of practice within pcHPSAs. The current study set out to understand the determinants shaping employment acceptance experience from the perspectives of PTs who practiced in pcHPSAs, to guide employers invested in recruiting and retaining PTs. Because pcHPSA designations encompass both non-urban and urban areas, the sample dataset was subsequently reconfigured to analyze responses using non-urban and urban classifications.
Primary care HPSA versus non-primary care HPSA
The current study examined valuation of employment acceptance factors by shortage areas. The results revealed PTs employed in non-pcHPSAs valued professional advancement more highly than those working in pcHPSAs. It is possible that the organizational structures within non-pcHPSA areas offer greater latitude for clinical and administrative advancement. Professional advancement questions also fielded responses about specialized practice that is not characteristic of the rural general clinician.
Relationships differentiated the whole sample by shortage designation, with those employed in non-pcHPSAs valuing relationships more highly. Relationship questions were specific to remaining in one’s ‘hometown’ and among friends and relatives. It is possible that these questions explain a hesitance for PTs who grow up in non-pcHPSAs to take employment in pcHPSAs, which may feel socially isolating to a PT without relationship connection. When evaluating determinants of employment acceptance among those planning to resign within 5 years, relationships no longer differentiated groups. Instead, remuneration emerged as more strongly discriminating, with PTs in non-pcHPSAs valuing these financial considerations more than those in pcHPSAs. Factors such as cost of living differences between pcHPSA and non-pcHPSA may, in part, explain these priorities.
Employers interested in attracting PTs to pcHPSAs should understand that the most highly valued aspects of employment for those working in these areas are practice environment, followed by attachment to place. Among those who share that they intend to leave, better income opportunity rises to the top, followed by retirement. Additionally, professional advancement discriminated pcHPSA PTs, with those who valued this determinant more highly being more willing to stay, perhaps to build a career with tenure. Employers are well positioned to control these factors (eg practice environment, workplace relationships, income, and opportunities for professional advancement) and should consider these values when strategizing ways both to recruit and retain PTs in pcHPSAs. Advocating for insurance reimbursement for direct access care delivered by PTs is one step in leveraging the expertise that PTs may contribute to pcHPSA needs.
An exploration of reasons for leaving revealed unanticipated differences between HPSA designation groups, with those working in pcHPSAs citing ‘retirement’ as the top reason for leaving, despite no statistically significant difference in age or practice tenure between groups. Further research should explore differences in length of practice for individuals in pcHPSAs versus non-pcHPSAs, as burnout may contribute to retention issues.
Non-urban versus urban
Among non-urban respondents, community assets discriminated those who leave from those who stay, with those who planned to leave within 5 years placing greater value on community assets. This non-urban group also described ‘better career prospects’ and ‘better income opportunity’ among the most frequently reported justifications for plans to leave. However, while DEAS professional advancement and remuneration were higher for non-urban respondents intending to leave compared to those intending to stay, these differences did not meet a level of statistical significance (p=0.093, p=0.123, accordingly). Interestingly, 23.3% of those in non-urban areas cited ‘partner relocation’ among their justifications for leaving, while just 8.2% of those in urban areas cited this same justification. This justification aligns well with the DEAS ‘attachment to place’ component, which was higher among non-urban respondents intending to stay. Pursuit of higher income was among the most frequently cited justification for leaving employment among both non-urban and urban providers.
The literature sheds light on these findings more broadly among samples of healthcare providers. Previous findings noted that loan repayment through programs, such as state health professional loan repayment programs, were influential in swaying 42% of healthcare providers who were predisposed to work in a rural environment (74%) to firmly commit to a rural community27. However, these same providers highly valued community location, scope of practice, and family fit, and, among those who ultimately left rural practice, just 22% cited higher income as justification for leaving28. The current study found 34.9% non-urban and 28.8% urban respondents with intention of leaving cited better income opportunity as a justification for leaving. Both non-urban and urban highly valued practice environment and attachment to place above all other factors. Consistent with the findings of Renner and colleagues28, non-urban response means were higher, though not significantly, than urban respondents (p=0.113; Table 7, Comparison A).
These analyses are predicated on a degree of respondent speculation, since questions were framed around intentions. The data cannot predict whether someone who reports intentions to leave will actualize this plan, nor can they discount a lateral move within the non-urban cluster designation. Nevertheless, a threat exists that reported justifications and rated determinants may explain a classification shift out of the non-urban and into an urban designation.
As was true of PTs in pcHPSAs, non-urban PTs reported high valuation of practice environment and attachment to place. Rural employers interested in recruiting PTs should consider that non-urban PTs intending to leave valued community assets more highly than those who planned to stay. Rural employers should consider community-building activities and investments that promote rich experiences, satellite options that can minimize commute times for those living outside of the non-urban area, and salaries commensurate with cost of living.
Limitations
Some conclusions from the current study are based upon respondent predictions about their actions in the future (eg importance of determinant in employment acceptance while still employed) or intentions (eg to stay or leave within 5 years). Surveying PTs who have recently left their employment or who are currently making an employment decision would provide more definitive results. However, the logistical efforts in identifying PTs meeting this inclusion criteria while still building a data set with sufficient power create barriers to this methodological approach.
Participants in the current study were disproportionately represented by individuals practicing within the Midwest region. Statistics representing the distribution of PTs in non-urban versus urban areas in the USA were not available to judge study representation. However, when compared to the US urban population (81%)27, the urban PT sample (67% urban) may be under-representative. Caution should be taken when generalizing these results to a broader population. These results are specific to PTs and are not generalizable to other disciplines or healthcare workers.
Conclusion
PT responses organized by pcHPSA designation revealed higher remuneration valuation among respondents from non-pcHPSAs intending to leave employment within 5 years, when compared to respondents from pcHPSAs with the same intentions. PTs in pcHPSAs who planned to continue their current employment valued professional advancement more highly than those who planned to resign within the next 5 years. When the data were reconfigured to look at PT responses by urban classification, community assets discriminated non-urban respondents by retention decision, with those planning to leave current employment in the next 5 years valuing community assets more highly. In summary, the problematic shortage of PTs, especially in rural and pcHPSAs, should be met with an evidence-based, strategic approach, including what is understood about unique values and employment determinants of those already embedded in these settings. This research suggests that approaches that prioritize practice, workplace relationships, income, and opportunities for professional advancement show recruitment and retention promise.
Acknowledgements
The authors acknowledge Kristy Hodne, Jeremy Van Klompenburg, and Michelle Wasland for their survey development contributions, and Taylor Kuehn for her assistance with designation categorizations.
References
You might also be interested in:
2015 - Measuring organisational-level Aboriginal cultural climate to tailor cultural safety strategies




