Introduction
The SARS-CoV-2 (COVID-19) pandemic brought about many changes in society. COVID-19 was given pandemic status from 11 March 20201. On 17 March 2020, the Scottish Government placed an emergency footing for non-elective care to be postponed. Following discussions in Parliament, non-urgent elective care was suspended to free up hospital capacity in response to the pandemic2. Health Protection Scotland introduced guidelines to follow with regard to personal protective equipment (PPE) and guidance as to which surgical procedures were permitted. These unprecedented changes impacted the way in which hospitals operated, with surgical departments cancelling elective work to leave only emergency care on offer. The Royal Colleges of Surgeons in England, Wales and Scotland (the professional organisation in the UK and some Commonwealth countries responsible for training, development and research in specific specialties) then also introduced guidance for individual specialties for which procedures could be performed, and the level of PPE required2,3.
A cancer response group was formed; however, this protected only those who were already living with a cancer diagnosis4. This allowed for those who were already receiving treatment to be prioritised to continue with treatment. Cessation of face-to-face outpatient clinics and also endoscopic procedures came into play in March 2020. These restrictions came about abruptly, which led to a backlog of abandoned outpatient clinic investigations (specifically endoscopic procedures, during which most colorectal cancers are diagnosed). These ‘blanket’ rules were introduced for the whole of the UK and did not account for the prevalence of COVID-19 in individual areas. Subsequently, the Scottish Government introduced a tier-based system that classified regions according to incidence of COVID-19 and instigated regional restrictions for social activity and visitation rights5. Such a system was not applied to surgical procedures, which might have allowed more work to be carried out in areas with lower incidence of COVID-19.
This study looked at the impact of COVID-19 restrictions on small communities, specifically the Orkney Islands, Scotland.
Background
The COVID-19 pandemic created numerous hurdles to accessing surgical services, including blanket national policies in place at the time that created additional challenges. These challenges affected diagnosis and treatment of surgical conditions including cancers.
It is known that the time from diagnosis to treatment of cancer is critical, with delays significantly increasing morbidity and mortality6. In Scotland, all patients referred to secondary care for cancer investigations have to be seen within 2 weeks of the referral being sent from a general practitioner7. The National Health Service (NHS) also has an aim that patients who are referred need to be treated within 13 weeks of referral.
Another barrier to patients accessing surgical services during the pandemic was fear of contracting COVID-198.
NHS Orkney has a small district general hospital covering a population of 22 000 across 20 inhabited islands. The Orkney islands are situated off the coast of mainland Scotland. There are two operating theatres, 22 acute inpatient beds for surgical and medical, four maternity beds and 16 rehabilitation beds. There are two High Dependency Unit (HDU) beds. During the pandemic, four Macmillan Cancer Support palliative beds were requisitioned for potential COVID-19 patients. Patients requiring higher levels of care are stabilised on the Orkney island until weather and other service demands allow transfer to tertiary centres on mainland Scotland. The day surgery unit was converted into a ventilation unit so that COVID-19 patients could be ventilated prior to transfer to a tertiary centre. This led to a reduction in availability for day surgery patients.
Methods
The number of patients diagnosed with cancer between June 2020 and October 2020 was compared with the period of June 2019 to October 2019. Stage (using Tumour Node Metastasis system) at diagnosis and the treatment options offered at diagnosis were examined, as well as the timeline between diagnosis and treatment, looking specifically at the delay caused by COVID-19.
Recurrent surgical admissions between April 2020 and October 2020, in particular those attributed directly to COVID-19 surgical restrictions, were also considered, as well as the number of COVID 19 cases in NHS Orkney during this period. A retrospective study was done to look at the admissions as outlined above using the local database. The data were obtained by interrogating case notes and looking at the hospital database for surgical hospital admissions during the time periods specified. Data were anonymised and all patient-identifiable information removed once diagnoses were established and confirmed as surgical.
Ethics approval
Although specific patient-identifiable data were not used, ethics approval was discussed with the hospital Caldicott Guardian. Caldicott approval was obtained to allow use of patient data. The latter was obtained because patient data are more easily identifiable in small communities. Individual consent was received from patients to allow for discussion in educational meetings and also writing of this article.
Results
During the period between June and October 2020, a total of 43 cancers were diagnosed. Of these, 15 patients were referred for best supportive care, two patients died before treatment was offered and three were referred for palliative chemo-radiotherapy. In the same time period in 2019, 42 patients were diagnosed with cancer. Of these, five patients were referred for best supportive care, one patient died before treatment was initiated and three were referred for palliative treatment (Table 1).
In 2020 (between June and October), fewer patients were referred for active treatment compared to the number in 2019 within the same time frame. In 2020, the number of patients referred for best supportive care was three times the number in 2019 and five times the number for the same time period in 2018. The delays caused by the COVID-19 pandemic are a suggested factor for this.
In 2019, most patients were within the 2-week wait target period from referral to diagnosis; only three were not, due to patients rescheduling appointments. In the month following the restrictions the average wait for urgent cases was 3.5 weeks. During April and May of 2020, no invasive investigations were performed, thus all cancers were diagnosed by imaging (CT and ultrasound scans). These were not included in the study as they were not diagnosed via surgical means.
Using colorectal cancer as an example, the average staging at diagnosis during the time period above was T3 disease. During this time some patients declined investigation as they were apprehensive that they would contract COVID by attending the hospital. This was evident because patients expressed their concerns during telephone consultations when invited into the hospital. The ‘did not attend’ rate increased by 25% between March and October. The data were acquired by looking at the outpatient clinic records of attendance.
Aside from cancer diagnosis, non-urgent work was significantly disrupted due to the pandemic in 2020. The average waiting time for non-urgent clinic consultation increased from 6 weeks to 18 weeks during this period. The number of patients awaiting endoscopic investigations increased threefold – from 20 on the waiting list pre-pandemic to 62. There was also an increase in the number of emergency admissions due to complications of disease. Following the lack of early/elective surgical intervention during the months April–October 2020 was an increase in the complications seen in biliary disease, hernias, diverticular disease and also delayed diagnoses of cancer.
The average waiting time for a laparoscopic cholecystectomy increased from 8 weeks to 20 weeks. Four patients on the waiting list for cholecystectomy attended with recurrent infection requiring intravenous antibiotic treatment. One patient awaiting laparoscopic surgery attended with a gallbladder empyema and required urgent cholecystostomy – dense adhesions prevented removal. Three patients attended with severe pancreatitis and two patients required transfer to a tertiary centre for intensive care support.
There was an increase in rare disease complications due to delay. One patient presented with gallstone ileus, which is known to be present in 0.3–0.4%9 instances of cholelithiasis and constitutes only 4%10 of patients who present with mechanical intestinal obstruction.
The waiting list during the pandemic to be seen in outpatients for a possible intervention such as hernia repair was 18 weeks. Hernia complications during the time period comprised four strangulated hernias, two spigelian hernias and one incarcerated hernia. Of these, one required HDU support following bowel resection due to gangrenous bowel. Of these patients, five were awaiting outpatient clinic appointments for hernias, one patient had no previous diagnosis of a hernia and one had declined surgical intervention, opting for conservative management prior to the pandemic.
Four patients attended with a delayed presentation of diverticular perforation – two underwent a Hartmann’s procedure and one required HDU admission for 2 weeks. Two patients were treated with antibiotics and had a sealed collection not suitable for drainage and one patient required laparoscopic washout of collection, and drain insertion.
A woman aged 34 years was diagnosed late with intussusception following an atypical presentation. The authors think diagnostic investigations were delayed due to COVID-19 as at the time of presentation the gastrointestinal symptoms could have been attributed to COVID-19 infection.
A delay was observed in the presentation of patients with acute appendicitis, with 50% of appendixes removed during this time being gangrenous and one patient presenting with a superficial flank abscess. Two patients who had been on the waiting list for sigmoid colectomy were readmitted with sigmoid volvulus.
In the same time period, NHS Orkney had 39 confirmed positive COVID-19 patients, with nine requiring admission to ward-level care and one death.
In the same period in 2019, there were no emergency procedures for complications of biliary disease. All patents who presented with acute cholecystitis were offered surgery within 8 weeks of admission or sooner if they presented with gallstone pancreatitis. One patient was admitted with gallstone pancreatitis; however they had previously declined definitive surgical management. On this admission the patient was reluctant to have further surgical management in light of the COVID pandemic. No transfers were required with pancreatitis, although two patients were transferred for endoscopic retrograde cholangiopancreatography. Two patients were admitted with volvulus; these patients underwent surgery after the third admission. Hernia repairs were performed within 6 weeks of being reviewed in the outpatient clinic. There was one incarcerated hernia and one strangulated hernia, and both of these patients had not been on the waiting list for surgery.
Statistical analysis could not be done due to the small numbers; however, it should be noted that small increments in a small district hospital dramatically affect the workload and cause a greater impact. In larger hospitals, an increase of two or indeed three patients would likely be ‘absorbed’ and would not be as clinically significant.
Table 1: Comparative treatment offered to patients with a cancer diagnosis between 2019 and 2020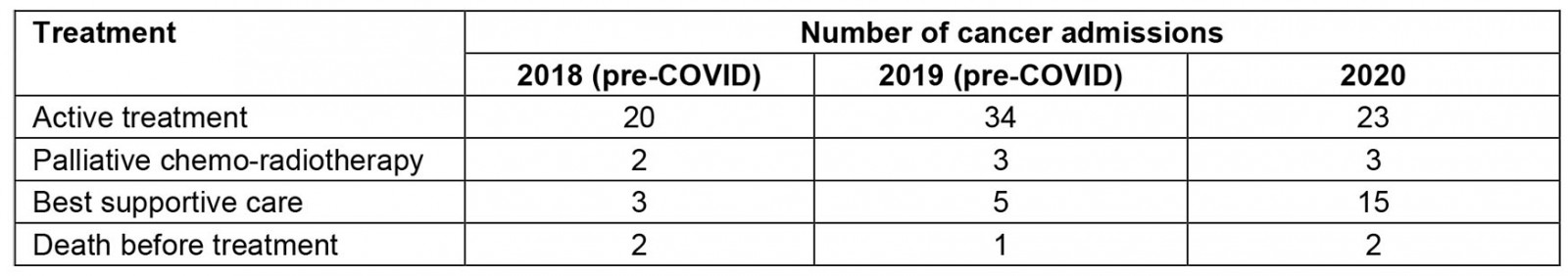
Discussion
The data show that, although the prevalence of cancers diagnosed was static, unfortunately patients presented at a much later stage, with significant impact on prognosis and quality of life. This corresponds with the delay in clinic review. Further, a significant proportion of these cancers were diagnosed through imaging alone, due to the COVID-19 regulations on procedures. During this time, although the number of cancer diagnoses equated to the same number as in 2019, the outcomes were very different. The patients in 2020 carried a poorer prognosis with disease diagnosed at a later stage. Data collected around late diagnosis are in keeping with a Macmillian Cancer Support report stating that an estimated 50 000 people were missing cancer diagnoses in 2020, when compared to diagnoses made in 20194.
The authors attribute the increase in missed appointments to patient fear and anxiety, intensified by the media and new COVID-19 information packs sent during this time8. Patients appeared to equate attending hospital with contracting COVID-19 despite low local rates of infection4.
The authors saw an increased rate of repeat presentations in patients awaiting definitive surgical management, within the timescale that elective surgery usually would have been performed. In addition, there were more complex and rarer complications of common presentations, with associated morbidity.
The results of the present study show that the blanket surgical restrictions for the NHS have negatively affected the populations in rural communities where the prevalence of COVID-19 was very low in 2020.
Conclusion
Although the effects of COVID-19 have been felt nationwide, the authors propose that the impact is more exaggerated in communities such as those in Orkney, due to the small population. It is likely that the indirect impact on surgical morbidity and mortality in this population in 2020 due to national restrictions was disproportionate given the relatively low prevalence of COVID-19 in the Orkney community. It is well known that rural communities face unique challenges, and most policies do not suit such environments11. The COVID-19 pandemic also illustrated that these rules may not be applicable in such communities. Further, due to limited island resources, a significant number of patients required transfer to tertiary centres for management of complications. This issue unique to the Orkney rural community illustrates the need for rules tailored for each environment12. Repeated admissions and use of HDU beds also have a financial impact.
The COVID-19 pandemic has placed an unprecedented strain on the NHS; however in the authors’ opinion this allows for learning opportunities. In the future, the Scottish Government and other governments with rural communities with rural health boards should consider a localised approach to restrictions in the NHS. Ideally, for health boards in areas with low infection prevalence, elective work could continue to avoid unnecessary delays, delayed diagnosis and treatment of time-critical ailments and reduce avoidable admissions into hospital. This would reduce the devastating indirect impact of COVID-19 on smaller communities where restrictions have been disproportionately high compared to COVID-19 prevalence in 2020.
References
You might also be interested in:
2015 - Halter traction for cervical spine injuries - initial treatment in the district hospital
2009 - Management of minor medical problems and trauma: the role of general practice
