Introduction
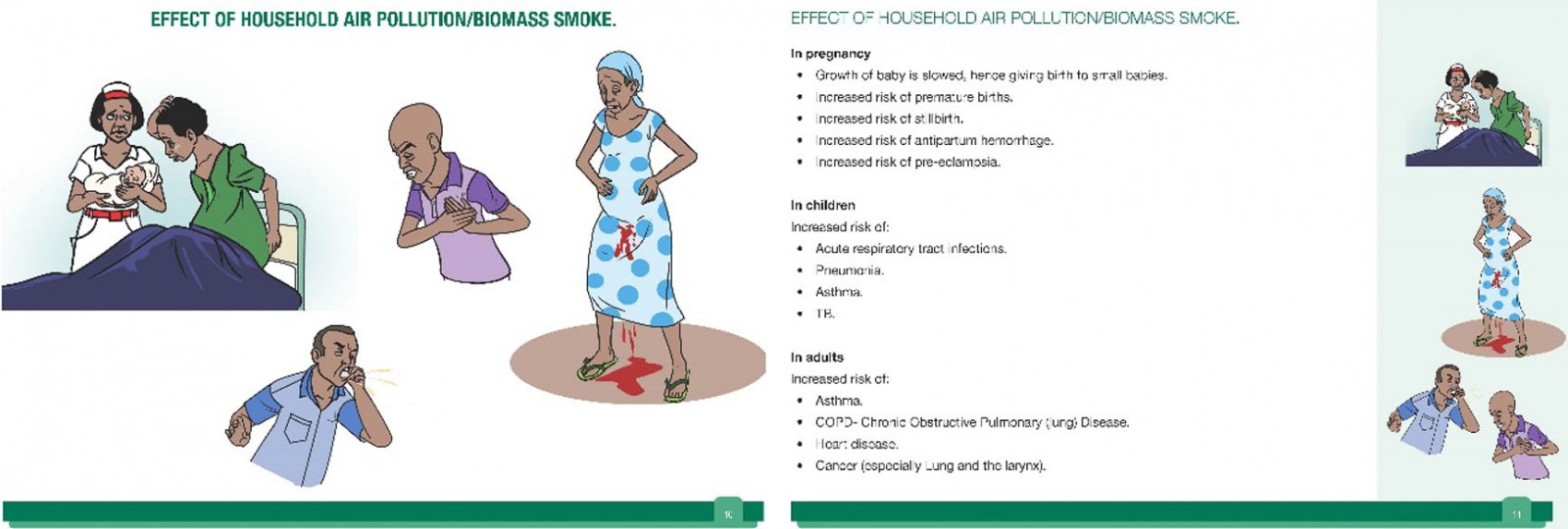
Globally, household air pollution is responsible for 3.8 million deaths per year, more than 700 000 of which are in Africa1,2. Three billion people, mostly in low- and middle-income countries (LMICs) like Uganda, use biomass fuel (any organic matter, such as wood and dung) for cooking, using cookstoves that create household air pollution and lead to adverse health outcomes. Household air pollution is linked to three of the top five causes of death in Uganda (neonatal death, respiratory infection and tuberculosis3,4), as well as negative pregnancy outcomes (eg low birth weight)5 and other non-communicable diseases like chronic obstructive pulmonary disease, heart disease, lung cancer, stroke, and a twofold increase in risk of childhood pneumonia1. The negative health impacts of air pollution have implications for babies in utero and onwards throughout life6.
Eighty-four percent of the Ugandan population live rurally7 and, on average, women work a disproportionately higher number of hours per day compared to men (15:8), as women carry out most of the family responsibilities, including cooking, in addition to agricultural work8. Ninety percent of Ugandans rely on wood for cooking fires, and women and children can spend up to 9 hours a day in small, smoky, poorly ventilated kitchens burning biomass fuels as well as being exposed to other sources of air pollution, such as burning rubbish. Women and children are therefore particularly vulnerable to the negative health effects of air pollution9-11.
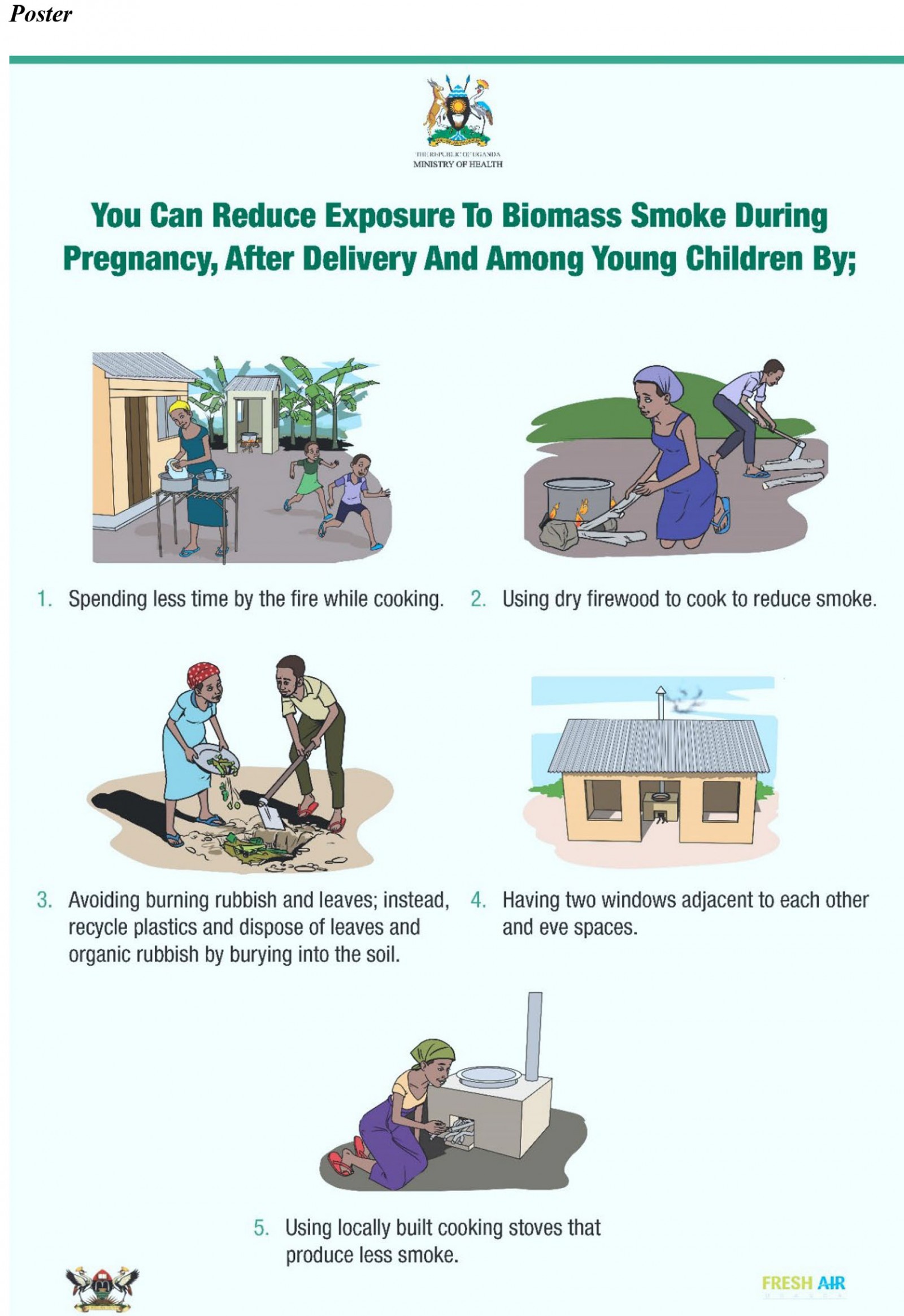
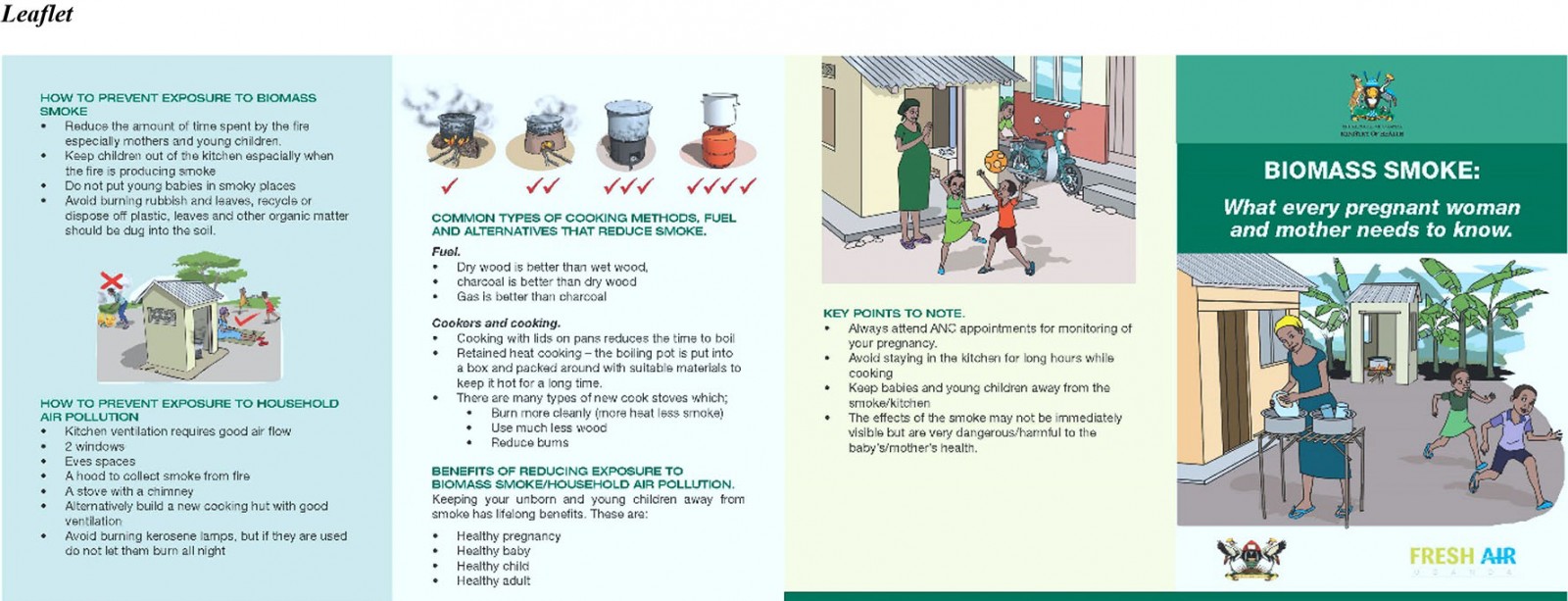
The Midwife Project, a novel implementation study, began in 2016 in response to these health risks12. It was felt that midwives were in an ideal position to reach women and children, with the aim of targeting health from in utero onwards to reduce lifelong risks, in an attempt to alter health behaviours from childhood onwards. Researchers from the UK and Uganda collaborated with midwives from the Jinja region of southern rural Uganda to produce educational materials in the form of a flipchart, poster and leaflet (Appendix I) for midwives and village health teams (VHTs, volunteers in the community who assist with health education and care outside of the health centre environment) to deliver to antenatal and postnatal women with the aim of reducing exposure to biomass smoke. These materials were approved by the Ministry of Health in Uganda.
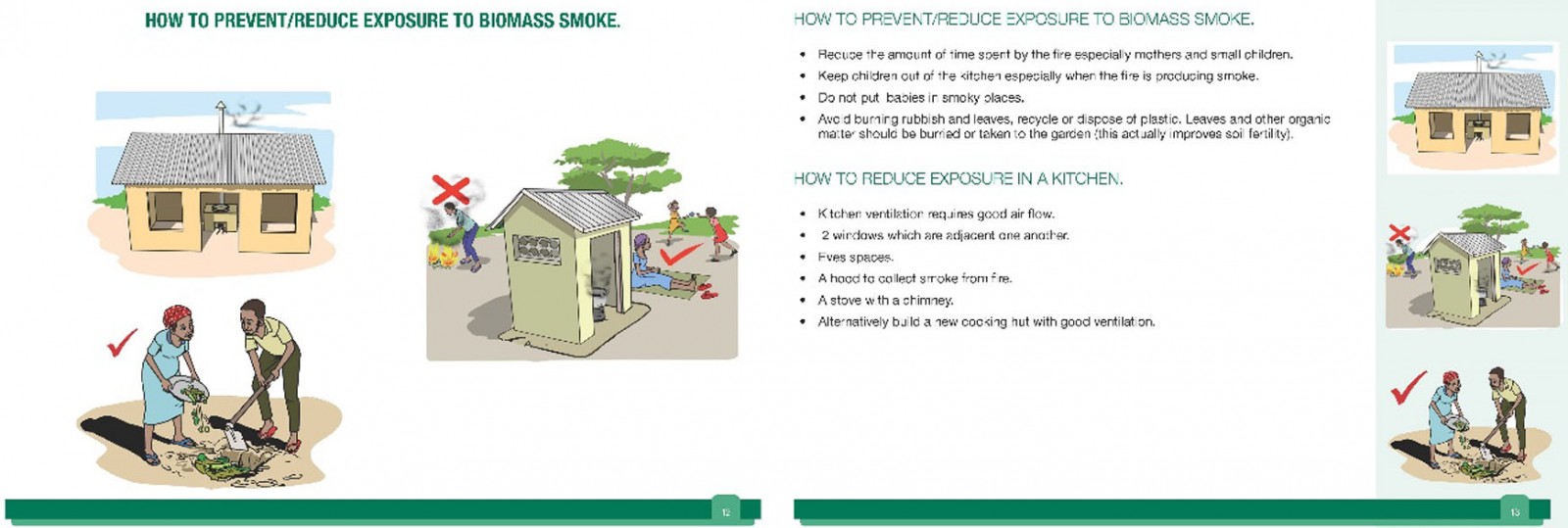
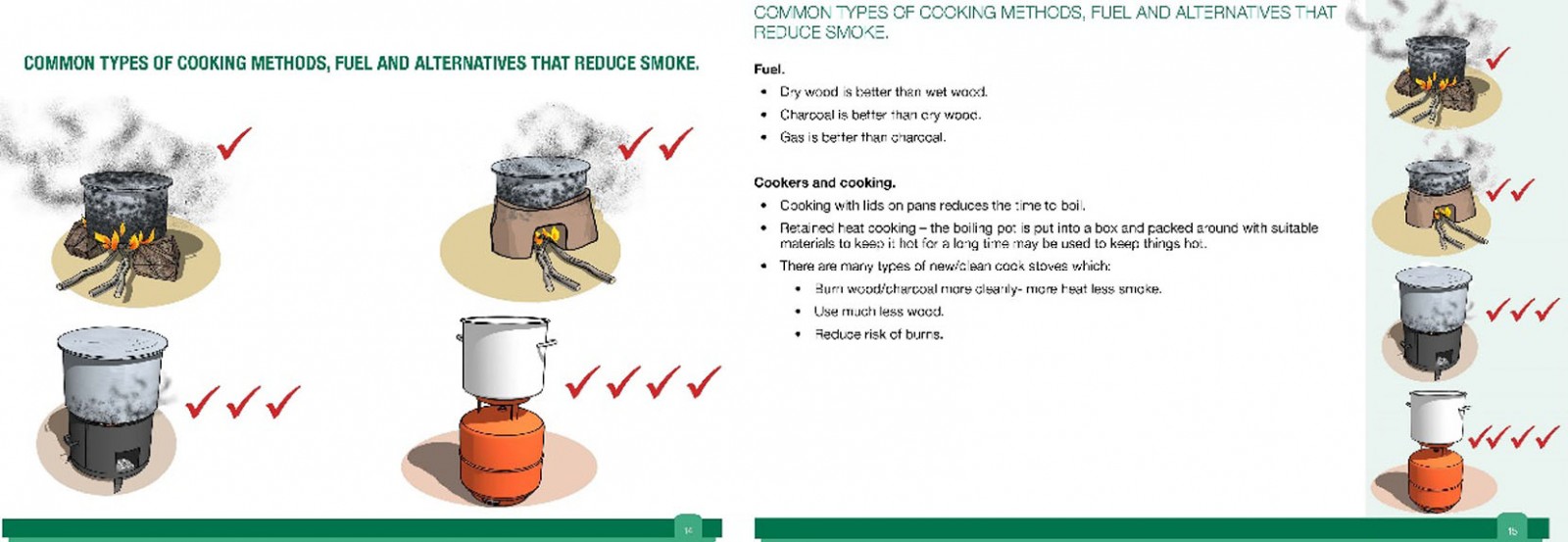
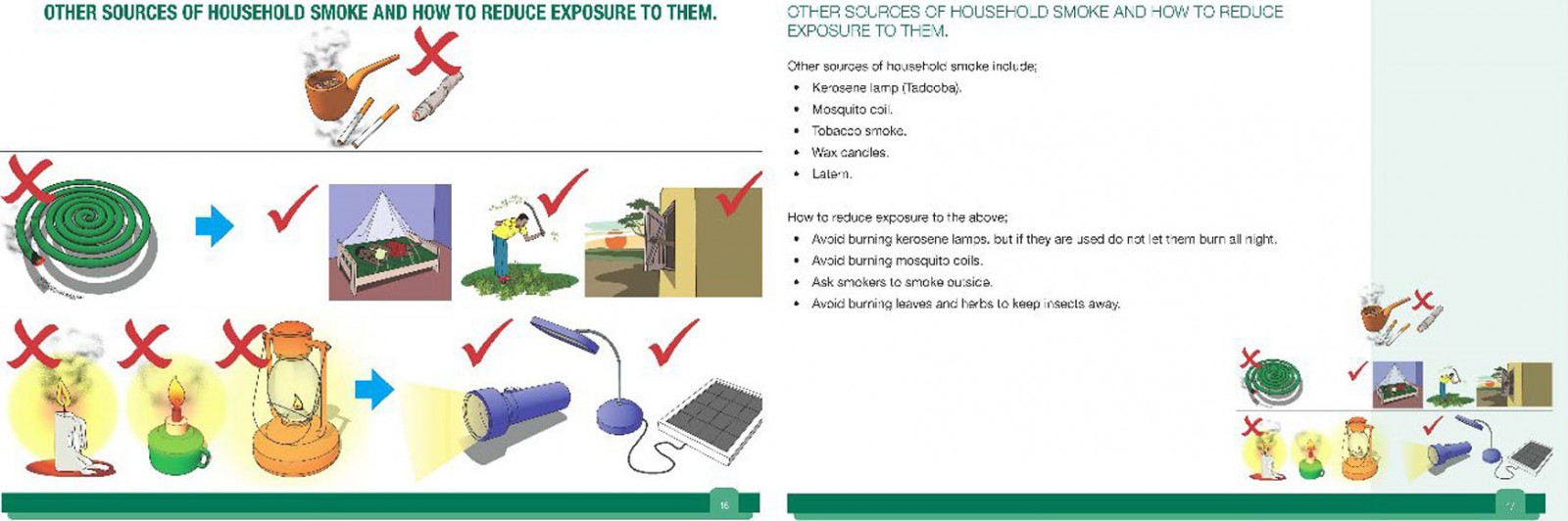
Midwives were recruited from four randomly selected health centre IIIs (rural facilities that provide outpatient and maternity care) in Jinja: Busede, Lukolo, Mpambwa and Wakitaka, and VHTs from the four corresponding villages were educated by midwives to reinforce topics in the community. Delivery was intended to be as often as healthcare workers (midwives and VHTs) felt able to, and to as many mothers as possible, between April and June 2018. Topics included sources of biomass smoke, health risks, cookstove improvement and placement, improving kitchen ventilation, improving fuels, and avoiding other sources of smoke (eg tobacco smoking, burning rubbish).
The Midwife Project originally aimed to examine feasibility and acceptability; and whether knowledge, attitudes and behaviours were changed. This was assessed with mixed methods: quantitatively with a before-and-after knowledge questionnaire for midwives, VHTs and mothers, and qualitatively, with 21 mothers interviewed. The qualitative assessment focused on education session content, and barriers and facilitators to attendance and engagement. Mothers found the intervention to be acceptable, although the main barrier was lack of money, which prevented them from being able to afford transport to attend the health centre and to buy materials for making changes. The education program was assessed as feasible, and knowledge was increased across all topics for healthcare workers and mothers alike12.
The overall objective of the Midwife Project was to design a health-improving education program suitable for wider rollout across Uganda. A 2015 systematic review of improved cookstove interventions concluded that longer term follow-up periods are necessary to assess sustainability13, but impact and viability past the end date of the original Midwife Project had not been examined, including if and how educational content had been shared between communities, outside of the health centre setting. Therefore, this follow-up study aimed to address the following research questions:
- What is the ongoing impact of this education program on behaviour change from the perspective of women and healthcare workers involved in this program?
- How has the program affected health from their perspective?
- Is program content being shared among the community, how is it being shared and what is the impact of this?
- Are any changes to program content required in consideration of widespread rollout?
In the original study, only mothers had been interviewed. For this follow-up study, it was essential to assess the views of healthcare workers as well to understand the impact on healthcare delivery in this context.
Methods
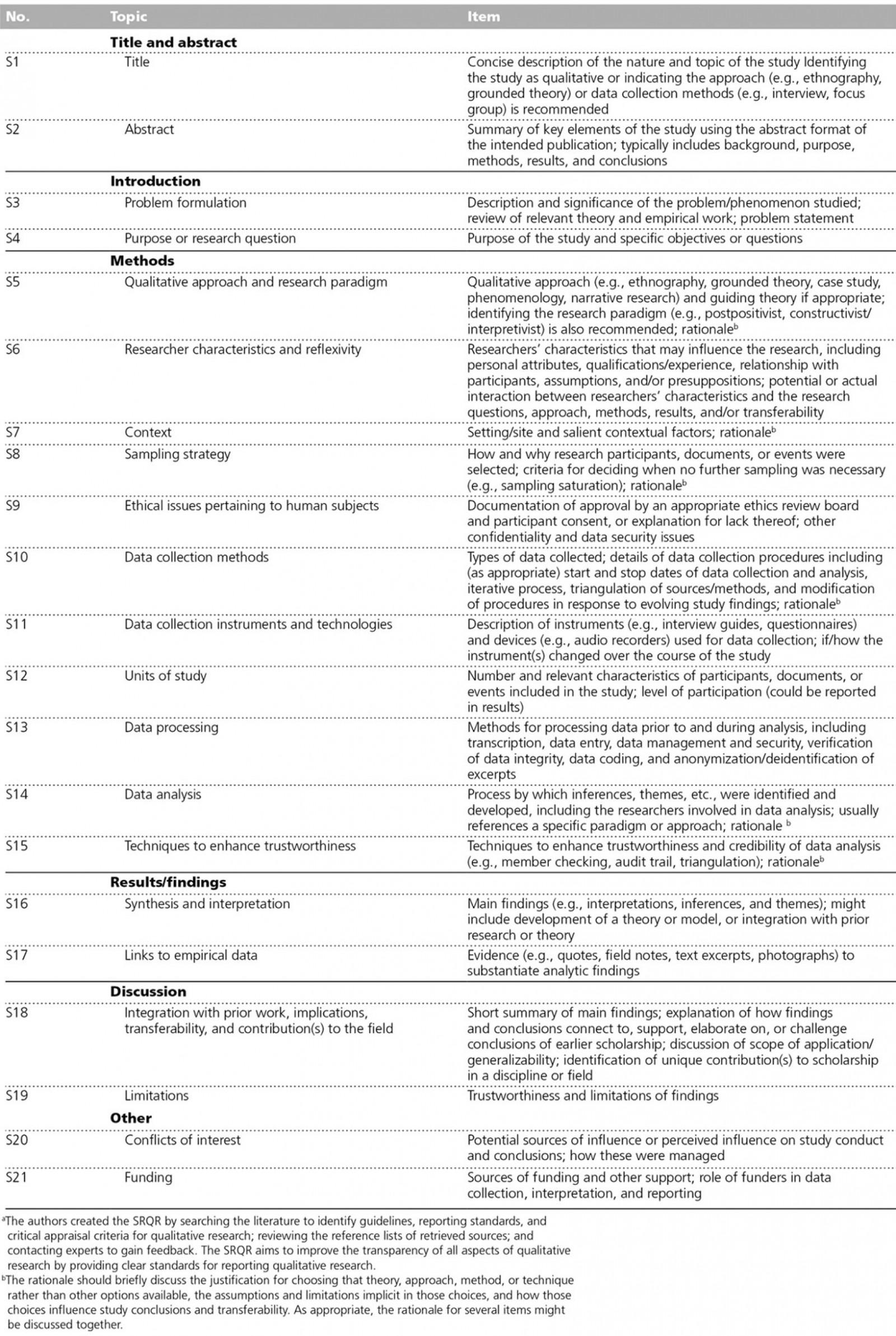
The Standards for Reporting Qualitative Research guidelines14 were used to guide reporting (Appendix II).
Sample
To enable pragmatic recruitment, purposive sampling was carried out by the research team at the Makerere University Lung Institute in Kampala and the District Health Office in Jinja. Eligible participants were consenting antenatal or postnatal women, midwives and VHTs who had previously attended or delivered an education session on biomass smoke. As the UK team could not easily return to collect more data, it was agreed beforehand between researchers that three mothers, two or three midwives and one VHT per health centre would be a sufficient number to balance practical considerations (eg time limitation) with the need to assess a range of experience and perspectives.
Data collection
Although it was originally intended to carry out interviews only, focus groups were conducted with midwives to minimise the impact on their time, as they had high patient caseloads at the time of data collection. Due to these time and access constraints, it was not possible to recruit off-duty midwives. All other participants were interviewed individually.
All interviews and focus groups took place over 2 days in February 2019 at the health centres in Lukolo, Wakitaka, Busede and Mpambwa in Jinja by two researchers and with the assistance of six translators as per availability. Translation was not necessary for midwives as they all spoke English. For translated interviews, questions were asked in English, then translated into Lusoga, the local dialect. The answer was given in Lusoga and then translated back to English. Attempts were made during interviews with mothers to encourage rapport with more familiar body language15.
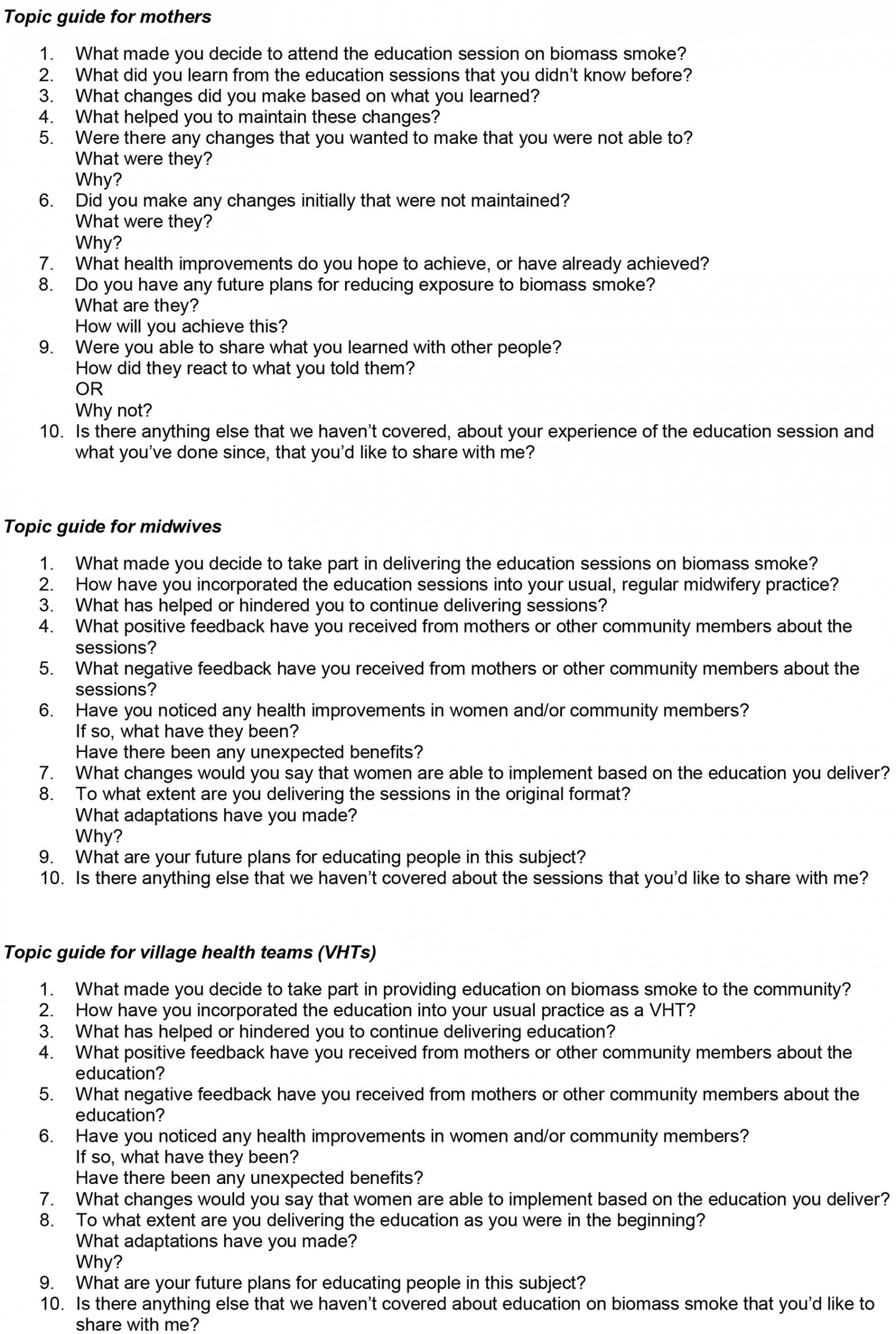
Interviews and focus groups were semi-structured and directed by topic guides tailored for each group (Appendix III). They were recorded with a password-protected audio-recorder, saved onto a password-protected laptop at the end of each day and then deleted from the audio-recorder. Reflective and observational notes were made by both researchers at the end of each day.
Twelve mothers who had attended the education program were interviewed, three per health centre. The time between first session attendance and interview ranged between 3 and 16 months. Four focus groups were conducted with 10 midwives in total, two to four per health centre (all female), and interviews with four VHTs (two male, two female), one per health centre. Interviews and focus groups took similar times to conduct, with a range between 17 and 36 minutes and an average of 27 minutes.
A second opportunistic visit to all four health centres was made in October 2019, while researchers were visiting for another research project. Informal discussions were held with combined groups of 12–14 midwives and VHTs, during which similar topics were covered to further examine similarities and differences in views, and changes to practice. Notes from these meetings were incorporated into the analysis.
Analysis
A qualitative thematic analysis approach was adopted following Braun and Clarke’s suggested six stages of thematic analysis: reading and familiarisation, coding across entire dataset, searching for themes, reviewing themes, defining and naming themes, and writing/finalising analysis16. Constant comparison was utilised throughout analysis by comparing new concepts with existing ones17.
Verbatim transcription and familiarisation of interviews and focus groups was carried out by the lead author, and coded thematically using NVivo Pro v12. There were two coding groups, one for mothers and another for healthcare workers, to separate out the different perspectives. Transcripts were initially coded in NVivo, then codes were refined into more coherent themes and subthemes. Where questions appeared to deviate from the topic guide in a leading way, a judgement was made about whether the response seemed unbiased, but responses to these questions were largely omitted. From each transcript, a narrative ‘story’ for each mother was also summarised separately, which provided context and a coherent picture for each woman, to aid understanding of individual motivations, thus further supplementing concept development.
A second researcher independently generated themes from a sample of transcripts, and this aided in corroboration of the thematic framework. The visit notes made during both trips in February and October 2019 were cross-referenced to identify any thematic corroboration or contrast. Illustrative quotes for this manuscript were chosen and anonymised for reporting by the lead author.
Ethics approval
Primary ethics approval was obtained in 2016 from the Mulago Hospital Research and Ethics Committee, Kampala as part of the FRESH AIR giant protocol (MREC 971, trial ID: NTR5759). A renewal of this approval was obtained for this study in February 2019. All participants provided written informed consent before participation.
Results
Although the education program was originally intended to be delivered between April and June 2018, midwives and VHTs reported in both February and October 2019 that they were continuing to deliver it frequently. However, only one mother mentioned VHT input during the February interviews and this was because they had directed her to an education session but not provided education themselves. Although there was a very wide range of topics learned, some aspects were not mentioned at all by mothers or healthcare workers: chronic obstructive pulmonary disease, using a kitchen hood, more efficient cooking methods (eg using a lid to reduce cooking time and thus reduce the amount of smoke produced), tobacco-smoking, burning leaves as an insect repellent, not burying plastic in the ground, and adding eave space for ventilation. Thematic16 and narrative analysis generated five broad themes as reported below. Illustrative quotes appear in the third person for mothers and VHTs, as interviews were translated in this way.
Ability to change, and changes made
Most women reported being able to make changes, the most common of which were to the cooking area itself (reconstructing the ‘traditional’ cooking place of a cooking pot balanced on three large stones to a more stable and efficient construction), changes to kitchen ventilation (increasing window space and installing chimneys), and staying away from smoke for both themselves and their children:
Now what she has learnt, or ever since she had knowledge about the smoke from the midwives, she now has improved on her cooking place, she has now learnt she should not sit with her children in the kitchen while cooking, as well as she should also not sit in there while cooking … that she has to get out, get fresh air and only check on what she’s cooking … She has constructed her cooking facilities with an improved stove. Instead of the ordinary three stones. (Mother 1, Mpambwa)
Some women also reported no longer burning rubbish, and changes to lighting from candles or kerosene to solar-powered. Some expressed wanting to make further changes if possible, although there were financial barriers that had prevented them from doing so yet, as reported below.
Ability to change dictated by money
Most mothers reported crop-growing as their main livelihood, with some acquiring additional money by other means in order to pay for suggested kitchen improvements. This included selling snacks or firewood, obtaining crop money from their husband, growing additional crops to sell and borrowing from the bank. However, some mothers had specific business ideas (eg selling clothes) but no money to move this forward.
Money as a barrier to change was also expressed by most healthcare workers, particularly with regard to the unaffordability of charcoal and gas as substitutes for firewood, something also mentioned by mothers. However, some mothers reported that by improving their cookstove, money was actually saved by buying less firewood and reducing medical costs to treat negative health impacts caused by smoke exposure:
She says that she now rarely goes to seek medical treatment as it used to be because there is great improvement … not as much as she used to do. She says that it has cut on the costs and it has made her see, even when it comes to maybe buying firewood. Because this modern stove requires little firewood compared to the other one whereby one has to keep lots of firewood. (Mother 3, Mpambwa)
Importance of practical education
Some mothers reported attending several education sessions – up to four – which was an unexpected finding and something that was not an intended outcome. This mostly appeared to be in an attempt to gain practical information about how to make changes, for example how to build a different cookstove, an element that is missing from the education material:
But she has heard it twice. They were first given information, then they came and they were told how to improve on their cooking places. (Mother 1, Mpambwa)
The mothers who did report being given practical information had been able to make changes themselves or even educate others practically, in a resourceful, cost-effective way:
She has told her friends, her neighbours. But some of them have requested her to go and construct for them. Because she has the knowledge and has constructed her place. She teaches them how to prepare, for example, the mud where they get bricks from. And then, when they are prepared, she goes and constructs for them. And tells them how to look after it. (Mother 3, Wakitaka)
She says that she didn’t put in anything like money but it is only the knowledge that she got together with her friends because they were taught how to do it. And together with her friends [she] set up a group, they went and used local materials to construct. They did it themselves because she didn’t bring in anybody to make it for her, she did it herself. Because she had no money, so she used the local materials and she constructed it there herself. They had groups of five. So they would construct one home and then when it was sorted they go to another home and another home after that. (Mother 1, Mpambwa)
Although there were consistent reports that some people were setting up groups and using cheap, local materials for construction, healthcare workers also acknowledged that others did not have the practical understanding to be able to do this:
In addition to telling people what to do, we need to take action. We need to teach them exactly what the stoves look like. Because some of them don’t know the techniques. (VHT 3)
Furthermore, healthcare workers recognised that there was misunderstanding about the importance of having two windows for ventilation18 (as per program content) rather than one, and this is reflected in the interviews with mothers:
But she says that, maybe what she did, she put in there only one window but it is wide … she has no specific reason. She just wanted one big window. Maybe she needs to be educated more about the need for two windows. (Mother 1, Wakitaka)
Perceived health improvements
Most women interviewed either had no knowledge of the dangers of biomass smoke exposure prior to attending an education session, or had heard from their community about the health risks associated with it, but didn’t believe it. Some stated that they believed the health risks after attending an education session with the midwives, and others reported that they themselves or others had only taken it seriously after experiencing the negative health consequences they had heard about:
There is one she used to tell and she refuses and refuses. But when she [mother] fainted, that very person has said now ‘I will stop’. (Mother 3, Lukolo)
One midwife reported that she had noticed differences in pregnancy outcomes for the same women, before and after education, and other midwives stated that once they had the knowledge, they realised the link between smoke and specific health problems in patients:
It was interesting, we are getting knowledge of which we are not aware. Because we are getting abortions [miscarriages], when you do investigation, you don’t see the cause of that. So now we are getting some abortion [miscarriage], this is biomass smoke. We’ve got that information. That knowledge. (Midwife 1, Mpambwa)
For healthcare workers, perceived health improvements for both mothers and themselves included reduced coughing, tuberculosis, pneumonia, pregnancy- and baby-related illness, asthma, rash and breathing difficulties. Mothers reported perceived health improvements in breathing, respiratory infections, bleeding during pregnancy, fainting, coughing and flu. More surprising findings included healthcare workers’ perceived reduction in burns for children, and in malaria, by both mothers and healthcare workers.
Passing on knowledge
Eleven of the 12 mothers reported educating others about biomass smoke (with the 12th intending to, now that she had taken the content seriously), and although it was reported that most people had reacted positively to this and had made changes, some had again experienced a financial barrier. Some mothers seemed unsure about passing the knowledge on more widely:
She has passed on the information to her immediate relatives. And she says that if she gets anything new and if she learns more, she is going to start telling the community. She says that she could, but maybe when we come back just as you’ve now come, you could give them more information before she is able to go out into the community. (Mother 2, Busede)
Several healthcare workers stated that they had encouraged mothers to share knowledge from this project with their community and that they had seen evidence of this happening. Both midwives and VHTs stated that obtaining money for transport was the biggest barrier to them sharing the education more widely, with the local community areas being geographically very large. However, this may differ between health centres, with one VHT conversely stating they felt in a good position to communicate with ‘masses’ of people. Healthcare workers expressed a desire to spread the message to other healthcare workers, communities, schools and churches.
Discussion
Main findings
Themes: The altered behaviours of healthcare workers and mothers suggest that this program was successful in delivering its key messages of the health risks associated with household air pollution and how to improve the home environment or avoid smoke to reduce air pollution exposure. Healthcare workers had continued to deliver this education long past the project end date, which was not a set expectation, suggesting acceptability and feasibility for sustained implementation. All mothers described their ability and desire to make changes to avoid biomass smoke in order to prioritise their health and the health of their families, even if lack of money had prevented them from changing everything they would have liked to. This included construction changes to cooking areas and housing ventilation, no longer burning rubbish, and a change to solar power for lighting.
There were some inspiringly resourceful stories from mothers about the ways in which they had overcome financial barriers, by making additional funds and/or, as a community, using cheap, local materials to construct new cooking areas themselves. Significantly, this shows that changes can be made in this context without the need to spend much money, and some experiences reflect actual financial benefits from using less firewood and spending less on medical bills. Many women also reported staying away from smoke, a completely free option. However, not all mothers had been given practical information, and it would seem that those making changes had only been able to do so by having explicit building advice, including how to do it cheaply or for free, suggesting inconsistency in healthcare worker knowledge.
There was some suggestion of health improvements, and it is interesting to note that some mothers reported only taking biomass smoke education seriously after experiencing or witnessing health effects. However, quantitative research would be needed to explore the validity of these subjective views. The repeated mention of malaria reduction was surprising as it was not an expected health improvement in relation to reduction in biomass smoke exposure. There are several possible explanations for this:
- There could have been a misconception regarding what constitutes malaria and perhaps the opportunity to clarify this was missed.
- The use of mosquito coils, which produce smoke, is one of the education topics. Several mothers stated that they had changed from using a coil to mosquito net and it could be that this provides better protection.
- Malaria incidence is reducing in this population, regardless19.
- It is possible that a reduction in biomass smoke exposure improves health generally and, in turn, malaria resistance.
- Malaria is one of the leading causes of death in Uganda20 and is therefore well-recognised; it could be that mothers mentioned it due to social desirability bias – reporting what they assumed they should (discussed further below).
There were also unexpected reports from midwives of fewer burns in children, which was attributed by them to improved cooking areas. Traditionally, the three-stone cookstove is located in a small, dark kitchen and can be very unstable and dangerous. With changes in construction and location, it is possible that children were being burned less.
Analysis of how education was shared demonstrated that not all mothers felt empowered to pass information on to others; midwives and VHTs could encourage communities to share education with as many people as possible and thus reduce unnecessary health centre attendance. There is, however, a risk of messages becoming distorted, and it is therefore important that the education being given is clear and consistent, and that VHTs reinforce the correct messages in the community. Despite healthcare workers being keen to share information more widely in places like schools and churches, there was already possible miscommunication evident, such as the misunderstanding of the need for two windows rather than one18. Further, there seemed to be misunderstanding of the VHT role in sharing education for this project, with midwives stating that they would like to go into the villages to educate people and one woman reporting that a midwife had visited her at home to ‘supervise’ changes. While this demonstrates enthusiasm and could be useful, this should be the remit of the VHTs. It is interesting that mothers did not really mention VHTs as having an educational role; this may not have been made clear, or could highlight a gap in VHT training.
Implications: Although money was perceived by some as a barrier to change, the authors suggest that the simple option of staying away from smoke, along with potential financial benefits, could be emphasised more to alter this perception. The inclusion of practical information in all education sessions could reduce the need for multiple session attendance, which was not an original intention of the program, thus reducing the time and cost burden for both mothers and midwives. Together, this would ensure all participants are given the same message and equal opportunity to make changes, and would be invaluable for future implementation of this program and possibly other similar public health interventions in low-resource settings.
A further adaptation to program content could be a review of education topics. There was a consistent focus on some education topics, while others were not mentioned at all; further qualitative interviews with healthcare staff and mothers could help to establish why this has happened. It could be that there are too many topics to focus on, understanding is limited in certain areas, the least useful topics as perceived by midwives are left out, or that mothers are not receptive to some ideas. Adaptation could therefore be warranted to make the education as focused and useful as possible. To optimise reach and impact, it is also important that women are empowered to share what they have learned and that the educational role of VHTs is clear to all.
The Midwife Project is a novel education program; as stated by the researchers involved, it is the first of its kind to utilise midwives in delivering health education on biomass smoke12. There is a knowledge and literature gap for examining implementation of this type of public health education program in Uganda, and indeed across Africa and in other LMICs. This follow-up study therefore informs understanding of how co-produced health education can be implemented and replicated in similar settings and for other health topics. A recent scoping review of health screening interventions in sub-Saharan Africa concluded that more effective interventions included those utilising community health educators and those targeting financial barriers21. The Midwife Project has included VHTs to educate the community, and this follow-up study has demonstrated how financial barriers can be overcome in this context.
Other studies aiming to reduce biomass smoke seem to focus only on the outcomes of providing improved cookstoves. However, two recent studies suggest that more needs to be done than simply introducing ‘cleaner’ cookstoves, by taking behaviour change into consideration and improving implementation strategy, aspects that have been neglected in previous interventions, and that can help to improve sustained change22,23. A 2018 systematic review and meta-analysis demonstrated varying effectiveness for health improvement following cookstove improvement, but did not examine the behaviour change and implementation implications behind this; inconsistent effectiveness of alternative cookstoves could be due to neglect of these important factors24. The Midwife Project therefore benefits both from taking behaviour change into account, by allowing women the autonomy of making adaptable and resourceful changes for themselves rather than just providing a different cookstove, and by employing an iterative implementation strategy involving midwives, VHTs and local communities at every stage.
Michie et al’s Capability Opportunity Motivation-Behaviour framework for understanding behaviour (Fig1)25 suggests that behaviour is influenced by capability, motivation and opportunity. It could be argued that the mothers making the most impactful changes were motivated by the education session(s) they attended, had capability by having the knowledge and skills to make changes, and opportunity by making additional money and/or having access to local materials.
The Midwife Project did provide evidence of increased knowledge in the original study, as did another awareness-raising education project for healthcare workers in rural Uganda in 201426. However, a recent review of education programs for midwives in LMICs showed lack of evidence that knowledge acquisition alone correlated with behaviour change or improved outcomes for women and children27. By taking behaviour change and implementation strategy into account, this follow-up study has demonstrated a different outcome in that behaviours have changed for those with capability, motivation and opportunity, and therefore there is additional potential for improved health outcomes. Utilising midwives to deliver other health-related messages in this way could be an impactful method for other public health interventions in Uganda and beyond.
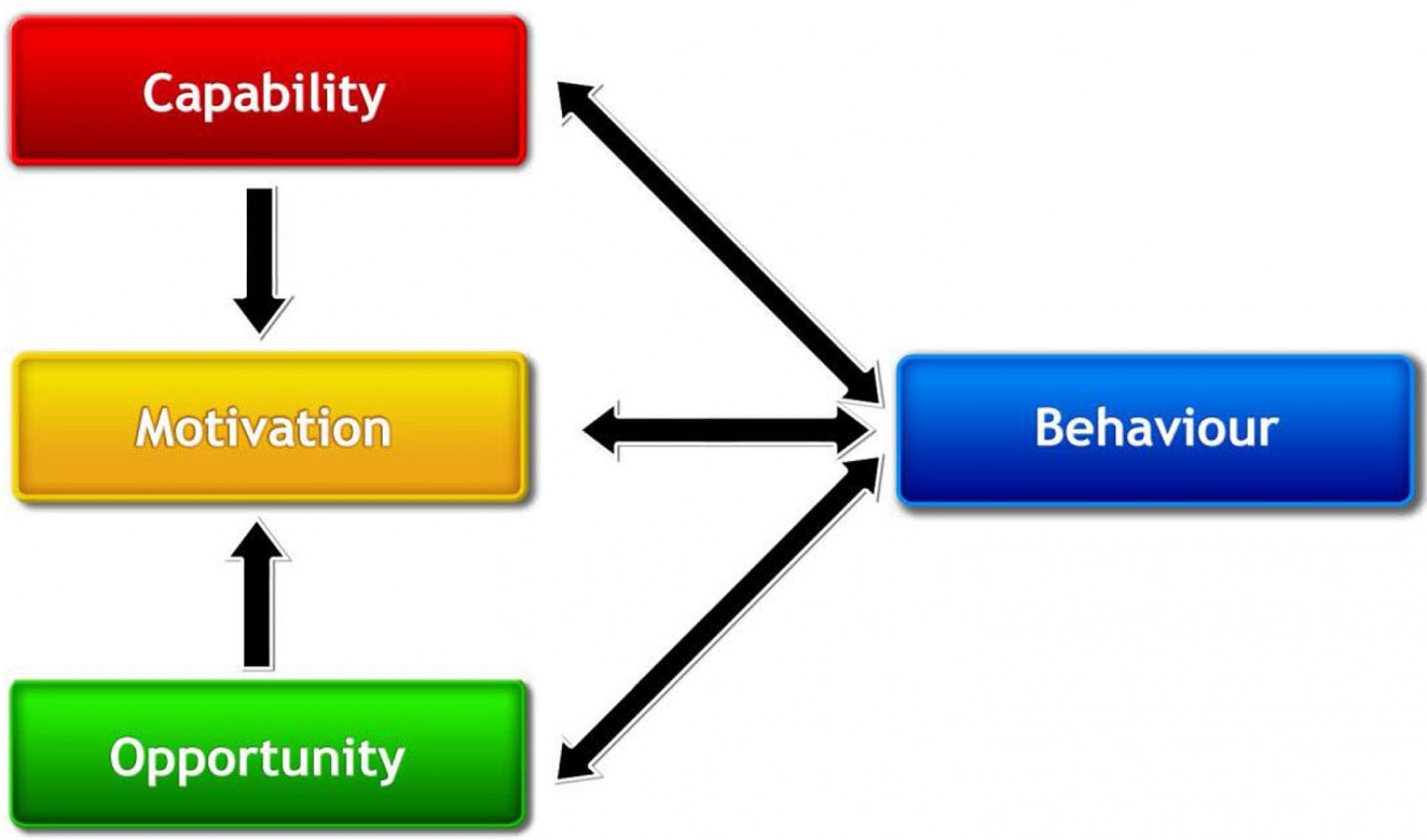 Figure 1: The Capability Opportunity Motivation-Behaviour system – a framework for understanding behaviour25.
Figure 1: The Capability Opportunity Motivation-Behaviour system – a framework for understanding behaviour25.
Strengths and limitations of this study
Participants were interviewed from four health centres spanning a large area of Jinja. The sample therefore represented a diversity of experiences in this region, a strength of this follow-up study that potentially optimises transferability for widespread rollout.
It is possible that there was some sampling bias in that mothers may have been chosen because of their enthusiasm to take part, and therefore they were more likely to express positivity. It was not feasible for the UK team to organise recruitment and so this is a potential limitation that the researchers were aware of from the start; attempts were therefore made to minimise sampling bias by liaising with the Ugandan research and healthcare teams responsible for recruitment.
There is also the possibility of social desirability bias in that mothers and healthcare workers alike may have stated what they felt the researchers wanted to hear in order to gain approval, especially due to differences in socioeconomic backgrounds; there was some evidence of recitation of education topics rather than answering the questions. One translator was the district health officer for women’s services in the region, whose presence may have increased this bias further by being a figure of authority. However, the topics recited were the same for both mothers and healthcare workers, at least demonstrating a consistency in the topics being taught and received. Attempts were made during interviews to balance encouragement with not praising responses too much, in order to minimise this bias.
Recommendations for future research and practice
Based on the findings of this research, the following recommendations are made for amendments to the program:
- Include affordable, practical building information in education sessions, including an emphasis of the importance of having two windows.
- Provide greater emphasis during education on overcoming financial barriers; for example, staying away from smoke is free, and it is cheaper overall to improve the kitchen than pay for ongoing firewood and medical costs.
- Emphasise the benefits of (consistent) dissemination of learning to others.
- Make the role of VHTs clearer to midwives, mothers and VHTs themselves.
Additionally, further research is recommended in the following areas:
- Further qualitative work is needed to review why some topics are being neglected and whether some items need clarification or removal.
- Although the health benefits of improved cooking conditions have been evidenced elsewhere28, the experience of health benefits in this study is subjective and cannot be relied upon alone; this would need to be triangulated with objective pre- and post-education quantitative data collection related to health impacts and outcomes, including malaria and burns. The District Health Office in Jinja has been contacted to assist in obtaining this data, although this is currently on hold due to COVID-19.
Conclusion
In an area for which there is very limited literature, this follow-up study has improved knowledge and understanding of the longer term impact of a midwife-led health education intervention and has shown that behaviour change and implementation strategy are important factors in enabling change in this context. Based on this study’s findings, adaptation to educational messages for this program would optimise impact for women in rural Uganda and could be used for widespread rollout. The Midwife Project strategy could have impact both for reducing biomass smoke exposure and therefore improving health, but also be used for other health-related interventions in low-resource settings. Further research is needed to enable refinement of education topics and to examine health benefits.
Acknowledgements
Funding for this study was supported by the Global Challenges Research Fund.
Authors would like to thank the research team at the Makerere Lung Institute and the District Health Office in Jinja for their invaluable help with recruitment and the organisation of visits to Uganda in February and October 2019; and the mothers, midwives and VHTs in Busede, Lukolo, Mpambwa and Wakitaka for their time and continued help in understanding implementation of The Midwife Project.
This is independent research supported by the National Institute of Health Research Applied Research Collaboration South West Peninsula. The views expressed in this publication are those of the authors and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.