full article:
Introduction
Poor health outcomes among lesbian, gay, bisexual, transgender, intersex, queer, and people with a diversity of sexual and gender identities (LGBTIQ+)1-4 highlight the necessity to ensure equitable access to high-quality care5. Research indicates these communities may experience myriad challenges when engaging with health systems, such as multilevel discrimination, receipt of inappropriate care, and insufficient expertise on the part of providers5,6. For LGBTIQ+ populations residing outside of major cities, the rural healthcare landscape has fewer services (specialist or general), health workforce shortages, and travel-related access burdens that can shape health and health care7-9. The precise nature and implications of this intersection of rurality and LGBTIQ+ identity are not yet well understood. Although rural LGBTIQ+ people form part of study samples, findings specific to this cohort are often not distinguished or explored, which may reflect a lower representation within the sample, as well as the possibility that rural LGBTIQ+ community members do not feel comfortable disclosing identity, including as part of research studies10,11, which in turn, impedes accumulating understanding.
To date, a systematic review of the peer-reviewed literature published between January 1998 and February 2016, limited to US samples, undertaken by Rosenkrantz et al (2017)10, offers the most comprehensive reporting on this body of work. They identified the presence of mental health issues, sexual risk-taking, and substance-use concerns among rural lesbian, gay, bisexual, and transgender (LGBT) communities for whom stigma, discrimination, insufficient provider cultural competency, and challenges associated with disclosure of identity were experienced in health service interactions. Further, features of the sociocultural context shaped these experiences including the education and approach of providers, a number of access barriers (eg costs), and a lack of social support, combined with social stigma. Rosenkrantz et al found ambiguous and inconsistent results in the comparison of the health and health care between urban and rural LGBT populations (compounded by methodological limitations in this body of literature) and concluded that the differences observed concerning rural populations warranted further investigation of the experiences of this population.
Findings from Rosenkrantz et al (2017)10, in addition to recent research7,12,13, underscore the need to support an emerging understanding of the health and healthcare experiences of rural LGBTIQ+ communities and, with it, grow capacity to inform policy and guide practice. This review contributes to these efforts by building and extending this foundation10, along several dimensions. First, the current review provides updated knowledge by synthesising the relevant evidence generated within the past 5 years. Second, the geographical scope of the study is expanded to Canada, Australia, New Zealand, and the UK, as well as the USA, to capture data from countries with comparable health systems that provide services to rural populations. Third, to aid comprehensiveness and incorporate those insights not represented in traditional academic outlets, grey literature is included.
Review aims
The present review seeks to progress understanding about rural LGBTIQ+ communities with regard to wellbeing, healthcare access and experience, and barriers and facilitators to health care.
Methods
Search strategy
Search strategies for the peer-reviewed literature were adopted from Rosenkrantz et al10, and revised to reflect updated terminology and the expanded focus. The strategy contained three blocks of relevant terms and keywords for identity-related terms, rural-related terms, and health and healthcare-related terms shown in Table 1. PubMed, Academic Search Premier, CINAHL, and PsychInfo databases were searched in August 2020 to capture literature published from January 2015 to August 2020. This timeframe was decided upon to capture relatively recent literature, including literature published since the Rosenkrantz et al review. Results of the searches were imported into EndnoteX9 and duplicates removed.
Grey literature was searched via Google Advanced Search for the same period. Given multiple groups of individual search terms, a customised Google Search Application Programming Interface (API) client was developed to combine terms in the aforementioned keyword blocks14. The automated algorithm generated a set of unique search queries for each possible combination of individual terms from each group, combined through the Boolean ‘AND’ operator. The algorithm was configured to ignore results from YouTube and Wikipedia, and to return a maximum of 50 results per query15. The returned results were aggregated and duplicates removed. In this work, three groups consisting of 5, 3, and 10 terms respectively were provided, resulting in 150 individual queries. A total of 6774 raw results were returned, of which 2785 were considered unique. Raw Google API results were parsed into a comma-separated text file, with each entry containing a numeric index, the query string from which it was returned, the results page number, page title, URL, and a summary ‘snippet.’ Reference lists of all included articles were screened.
Table 1: Search terms for database searches of peer-reviewed literature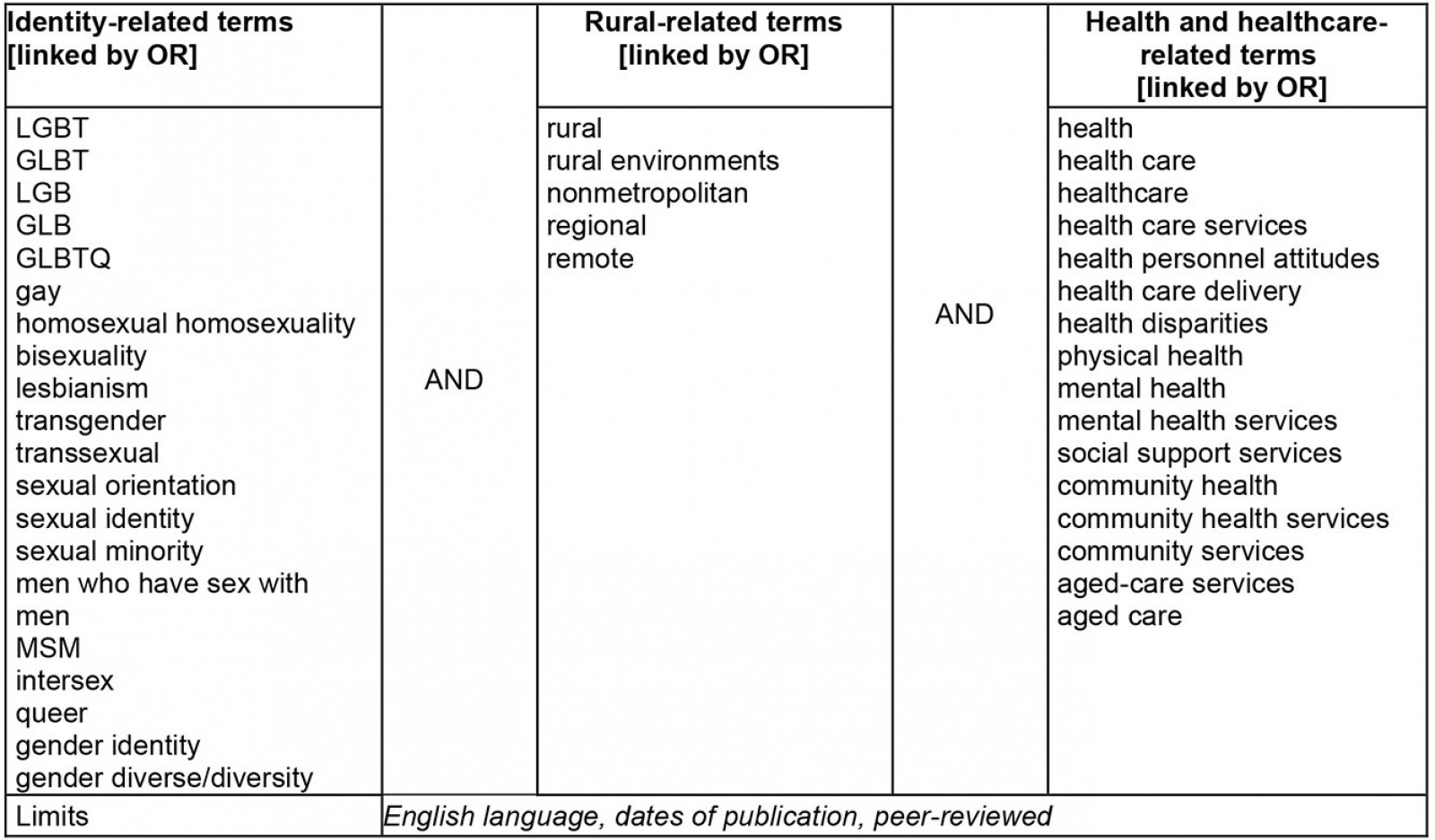
Inclusion criteria
Records were included if they were published in English; qualitative, quantitative or mixed-method; reported findings from the US, Canada, Australia, New Zealand, or UK; published between 2015 and 2020; and reported on the health of and/or healthcare services for LGBTIQ+ adults in rural areas. The reporting of primary findings was required for peer-reviewed records. Study selection was documented and is summarised in a flow chart compliant with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)16 (Fig1).
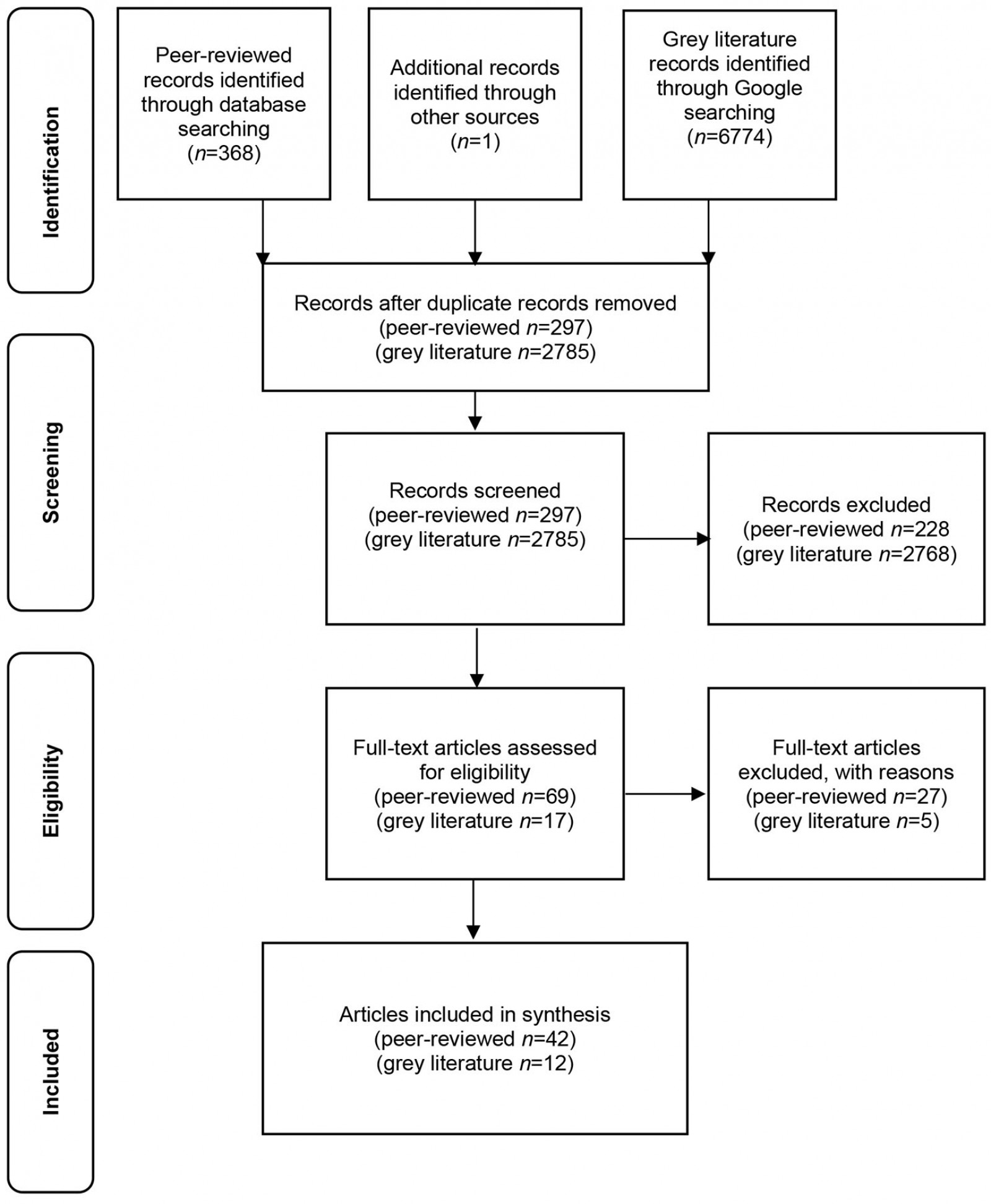 Figure 1: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart for search strategy of peer-reviewed and grey literature
Figure 1: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart for search strategy of peer-reviewed and grey literature
Study selection
For the peer-reviewed articles, one author reviewed the titles, abstracts, and full texts of articles that appeared to meet the inclusion criteria; another author followed the same procedure for the grey literature. At each step, a second author reviewed a sample of 10% of the articles to ensure consistent application of the inclusion criteria. Throughout the process, consultation was undertaken between the authors to resolve any uncertainty, and progress was reported on and discussed with all authors.
Quality assessment
The quality of peer-reviewed studies was assessed using the Mixed Methods Appraisal Tool (MMAT)17. This tool was specifically designed to assess a range of quality dimensions in qualitative, quantitative, and mixed-methods research. The Authority, Accuracy, Coverage, Objectivity, Date, Significance (AACODS) checklist18 was used to appraise the grey literature. An independent assessment of all included literature occurred and, in each case, a second assessor examined a 10% sample for rigour.
Data extraction and synthesis strategy
A purpose-designed Microsoft Excel template was used to guide data extraction, which included citation, year, title, country of study, population, study aims, study design, recruitment strategy, sample size, data collection method, analysis method, barriers, facilitators, findings, and other similar details. These data were then grouped thematically corresponding to the key areas of focus. Microsoft Excel software was used to manage and assist with the analysis. The reporting framework employed in Rosenkrantz et al10 offered an initial template for grouping the data, which was subsequently revised to better capture the data collected in this review.
Ethics approval
Ethics approval was not required as the systematic review include publicly available resources and data from published studies.
Results
Searches conducted on literature published between January 2015 and July 2020 returned 296 unique peer-reviewed records and 2785 grey literature documents, with one additional peer-reviewed record included following reference list review. The full texts of 69 peer-reviewed papers and 2785 grey literature documents were assessed for eligibility. A total of 27 peer-reviewed papers and 2773 grey literature documents were excluded on the basis that metropolitan and non-metropolitan data were not distinguishable, LGBTIQ+ participants’ data were not distinguishable, or there was insufficient focus on health/health care. Subsequently, 42 eligible peer-reviewed papers and 12 grey literature documents were included (Fig1).
Characteristics of included studies
Complete details of the included peer-reviewed studies and the grey literature are shown in Tables 2 and 3, respectively. In summary, studies from the peer-reviewed literature were conducted in the USA (n=27)13,19-44, Australia (n=8)7,12,45-50, Canada (n=4)8,9,51,52, the UK (n=2)53,54, and a single study conducted in both the USA and Canada (Table 2)55. Grey literature was produced in Australia (n=6)56-61, the USA (n=5)62-66, and Canada (n=1)67 (Table 3). Peer-reviewed studies used a range of quantitative (n=20)19-24,26-28,30,32,33,35-39,41,48,55, qualitative (n=17)7-9,12,13,25,29,34,40,43,45,46,49-52,54, and mixed-methods (n=5)31,42,44,47,53 designs. Grey literature comprised reports (n=4)56,64,66,67, articles (n=5)60-63,65, submissions (n=2)57,58, and an information sheet document59.
In the peer-reviewed literature, 36 studies reported findings from LGBTIQ+ communities, most commonly men who have sex with men (n=7)13,28-30,33,39,53; lesbians (n=7)20-22,25,34,35,50; lesbian, gay, bisexual and transgender (n=4)36,37,41,45; and transgender (n=4)7,9,24,40. In the grey literature, communities most commonly identified were lesbian, gay, bisexual, transgender, and intersex (n=3)56,57,59; transgender (n=2)61,63; and lesbian, gay, bisexual and transgender (n=2)60,64. Some of the literature concerned specific subgroups, namely elders (n=5)25,46,50,54,57, veterans (n=2)24,32, and young people (n=4)12,45,48,67. Healthcare provider perspectives were reported on in nine peer-reviewed studies7-9,31,38,42-45 and in five of the grey literature documents57,61,63-65. Additionally, in one study, general practices were examined via document analysis49. The majority of the peer-reviewed studies and grey literature addressed some aspect of engagement with health services. Across these bodies of literature multiple or non-specific health services were most frequently referenced.
Table 2: Characteristics of included peer-reviewed studies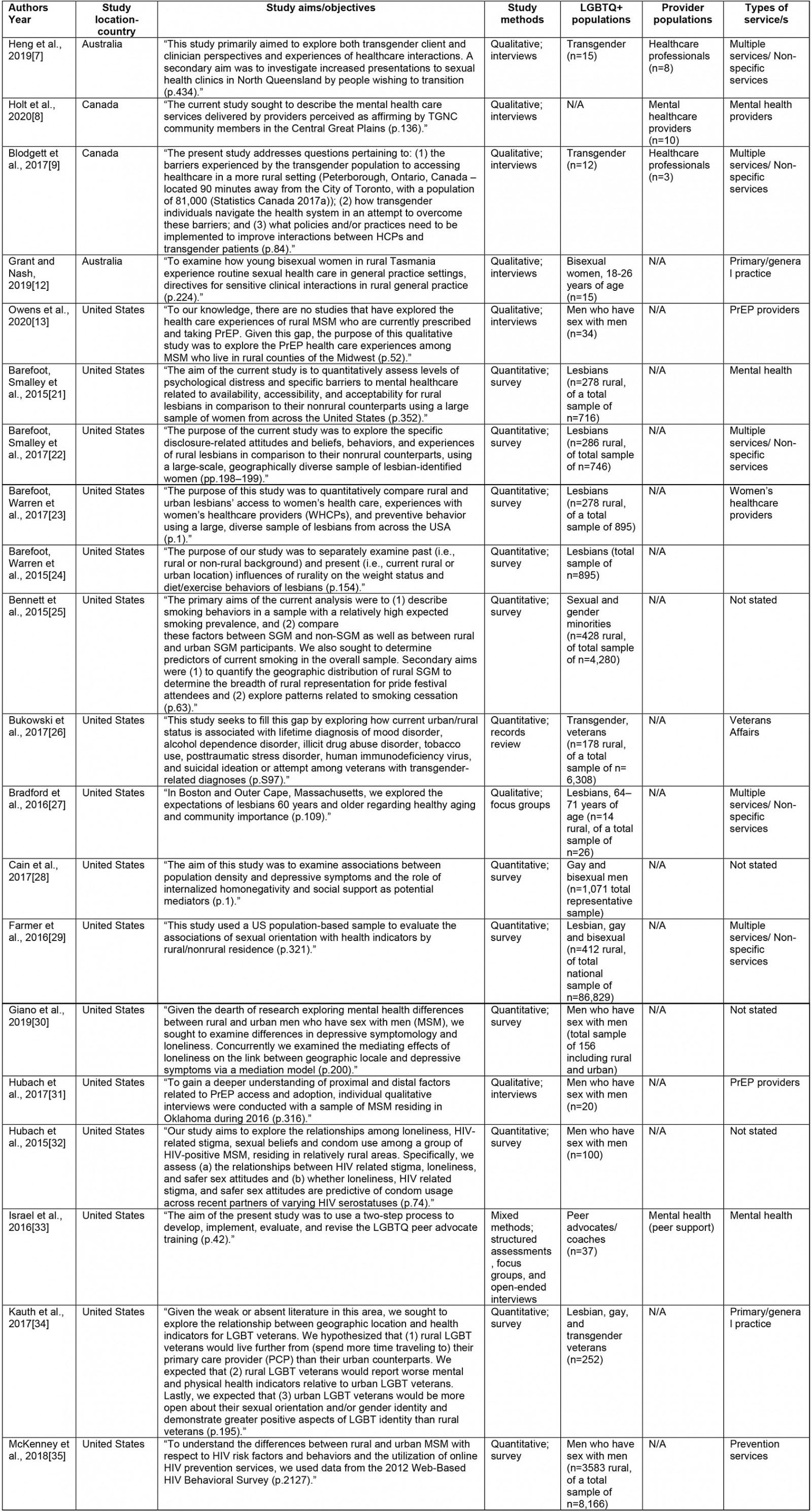
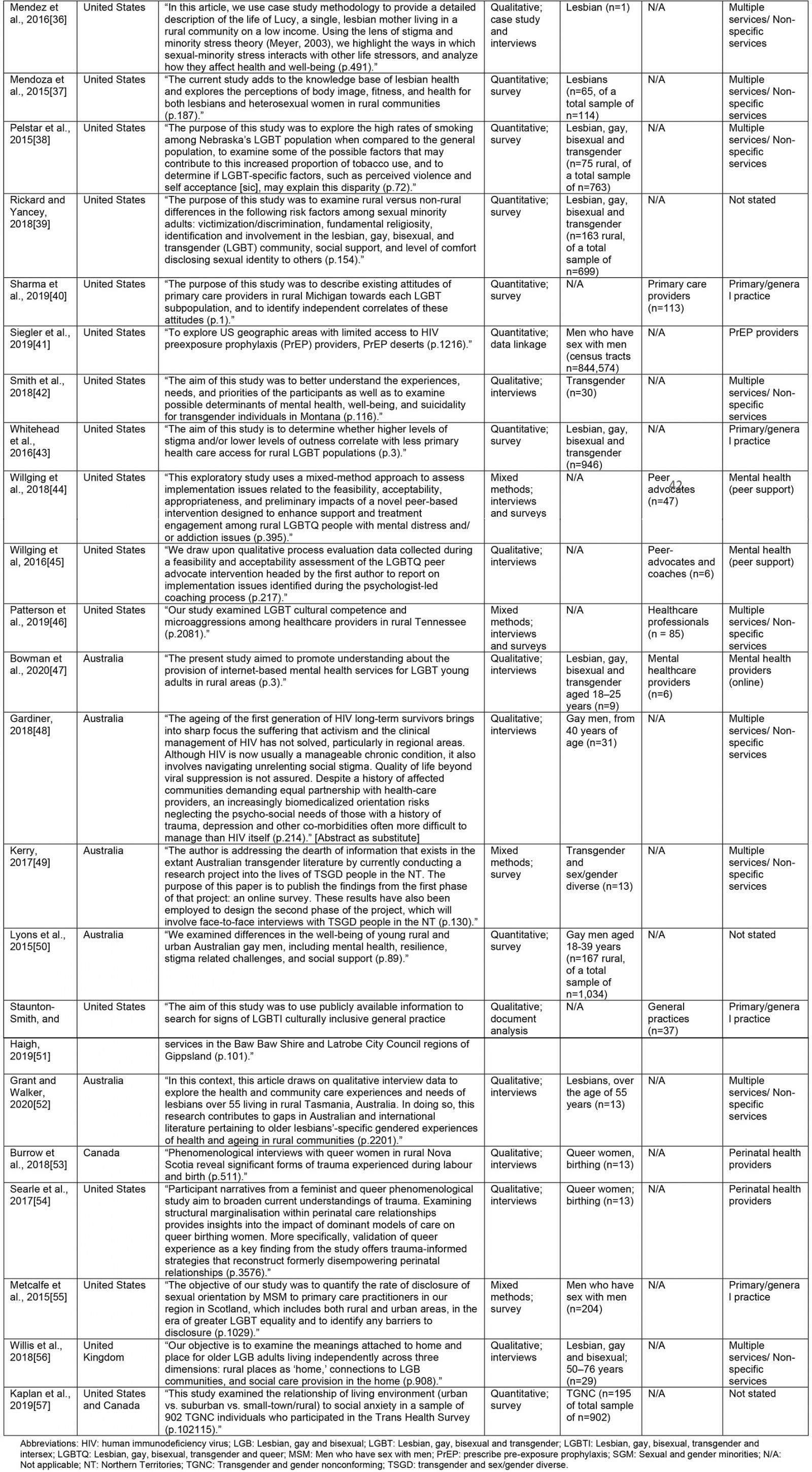
Table 3: Characteristics of included grey literature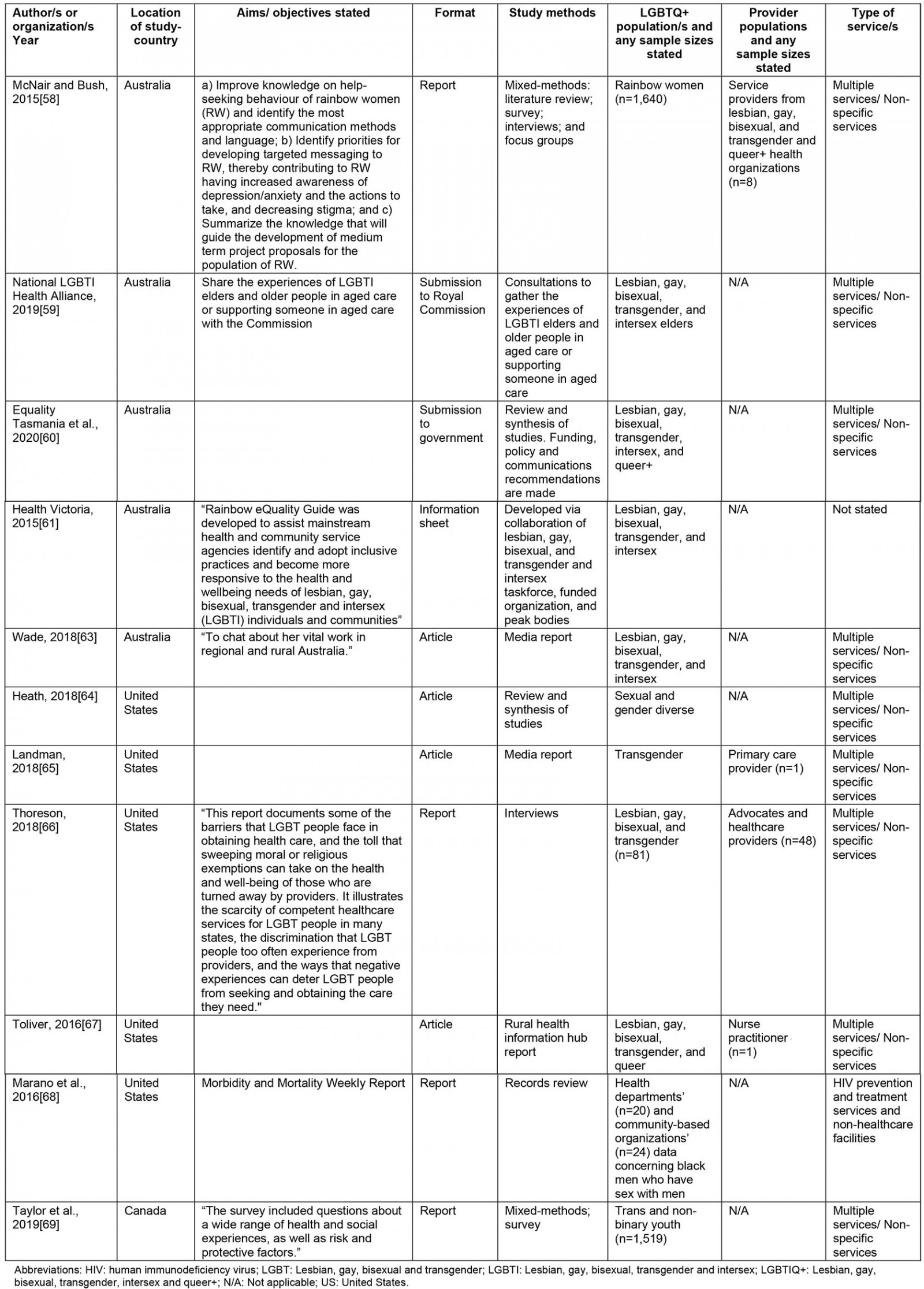
Quality of included literature
The majority of peer-reviewed studies satisfied 80% or more of the quality components corresponding with the study design (Table 4). On average, the grey literature satisfied 5.5 of the six AACODS criteria, with a range of 4/6 to 6/6 (Table 5).
Table 4: Mixed Methods Appraisal Tool quality appraisal of peer-reviewed literature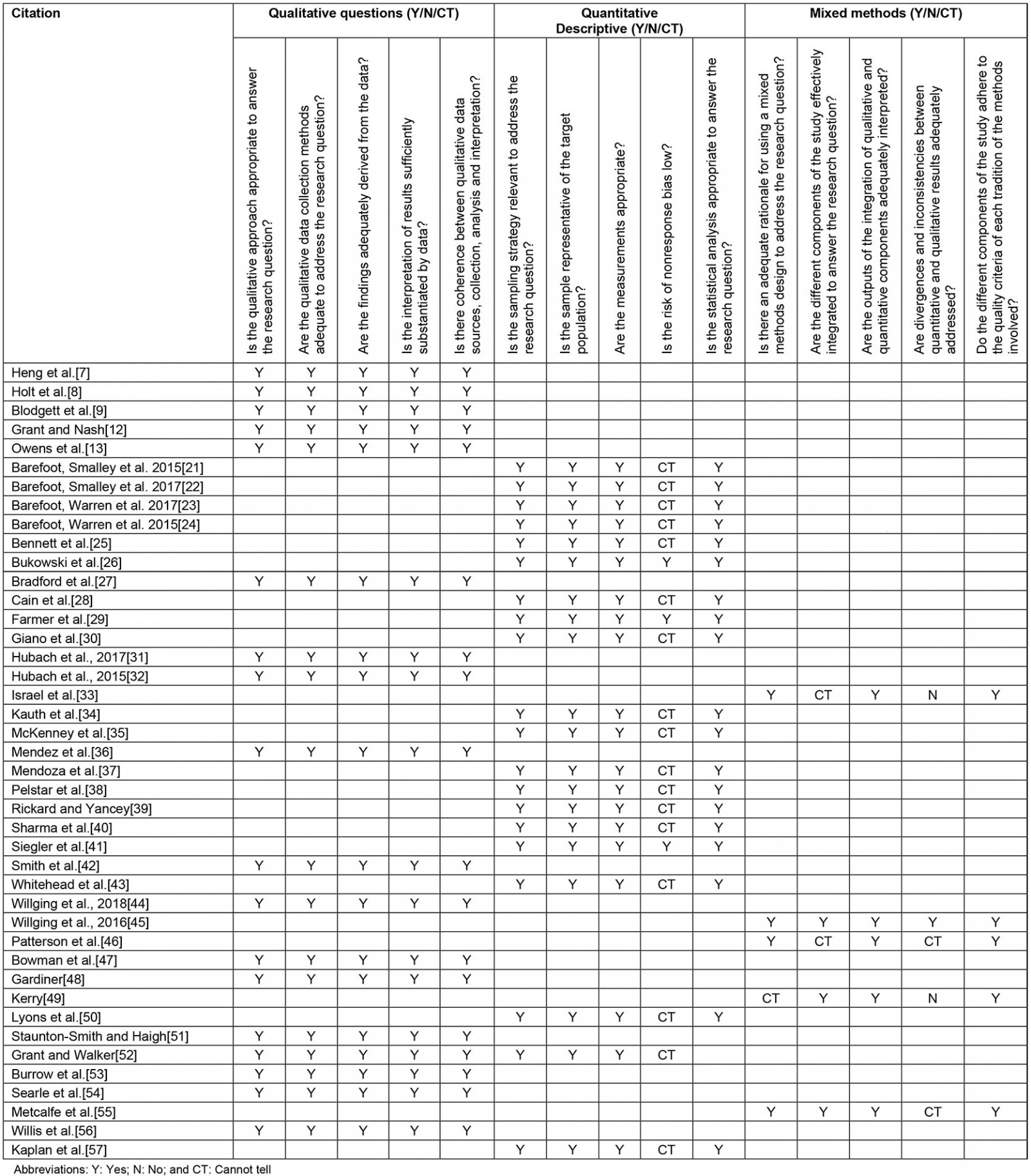
Table 5: Authority, Accuracy, Coverage, Objectivity, Date, Significance quality appraisal of grey literature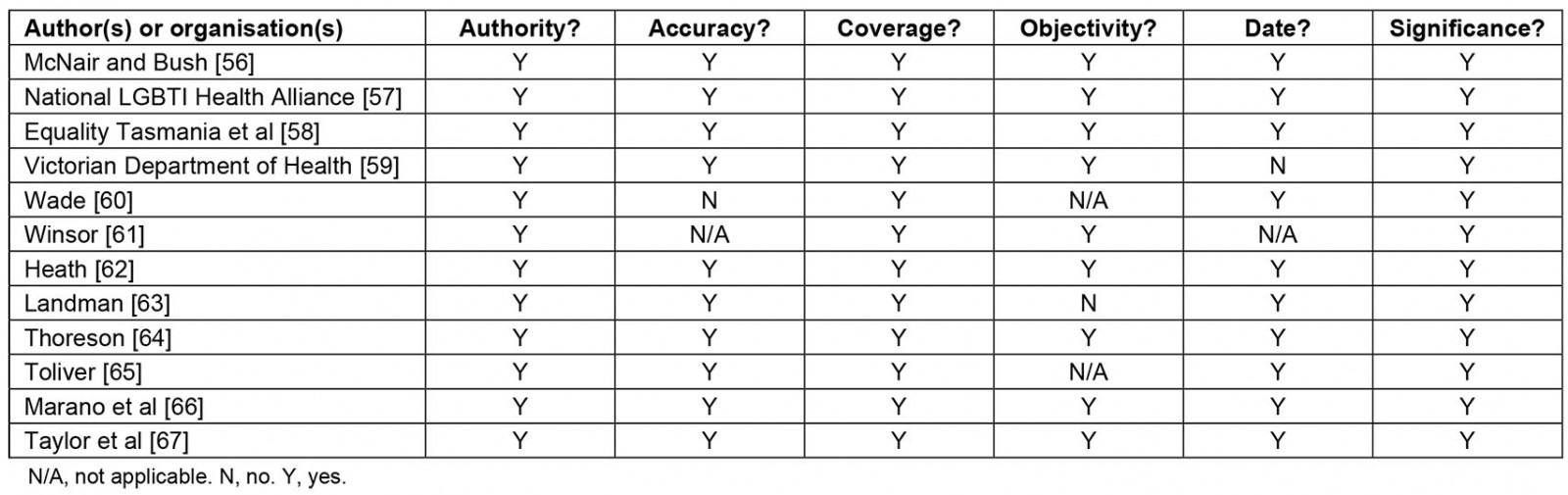
Synthesis
Data synthesis resulted in four superordinate themes: wellbeing, healthcare access and experiences, barriers, and facilitators. The first theme examines various domains of health status, while the second theme presents the experiences of rural LGBTIQ+ communities in engaging with health care, including reporting findings of what has constituted quality care. The final two themes identify those barriers and facilitators that are interconnected with health status and experiences of engaging with care. Table 6 depicts themes and nascent subthemes identified in included studies.
Table 6: Themes and subthemes identified in included studies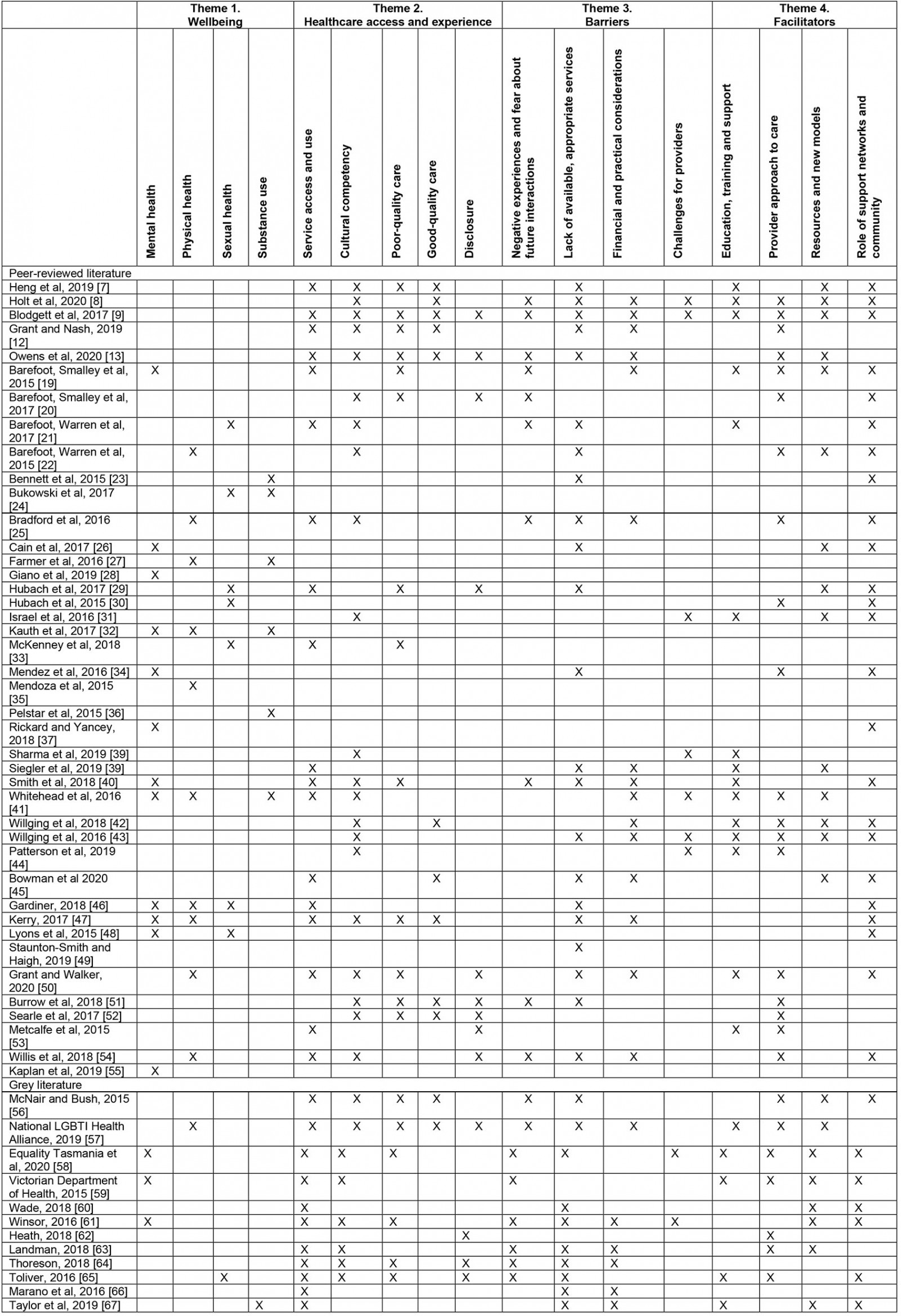
Theme 1. Wellbeing: This theme concerns mental, physical and sexual wellbeing, as well as reporting on substance use.
Mental health Depressive symptoms were reported as an issue among rural LGBTIQ+ communities26,28,32,41,46,47, as were anxiety32,47,55, and elevated psychological distress (measures often included indicators of depression and anxiety)19,48,58. Multiple studies noted the interconnections between mental health and participants’ reduced comfort in disclosing sexual identity37,48, as well as deficits in community support, isolation and loneliness26,34,37,40,46,48,58,59,61.
Physical health Studies reported a mixture of good47 and poor27 overall health, with differences noted among subgroups (eg cisgender men reported better health relative to other groups)41. Co-morbid and chronic conditions were identified as impacting health status41,46,47, with approximately a third of participants diagnosed with chronic conditions in one study41. Weight concerns were also identified as an issue22,27,32,35. Where ageing was examined, participants expressed fears about decline in physical health, mobility, and were concerned that being forced by disability or illness to enter assisted living where their isolation might be further exacerbated25,50,54,57. Gardiner’s (2018)46 research provided insight into the intersections of ageing, rurality, and living with HIV, where rural gay men felt that the complexities of their lived experiences had given them wisdom that could be applied to the process of ageing46.
Sexual health Rural LGBTIQ+ community members reported receiving insufficient sexual health education and prevention counselling21,29,33,65. Mixed results were found where studies compared prevalence of rural men living with HIV to their metropolitan counterparts24,30,33,48. For MSM in rural areas, HIV-related stigma was correlated with loneliness and impacted sexual health practices30. Older gay men living with HIV in rural areas also managed co-morbidities and treatment side-effects46. It is important to contextualise this information within the broader experiences of provider interaction, as will be discussed in the following sections.
Substance use A high prevalence of current and former tobacco use among rural LGBTIQ+ communities was indicated in several studies23,24,36,41,67, with some studies indicating differences among subgroups within these communities27,32. Whitehead et al (2016) found a high prevalence of binge drinking among rural LGBTIQ+ communities41. In other studies, rural status was not found to significantly impact alcohol or illicit drug issues24,32. Similarly Bukowski et al (2017) found that neither rurality nor urbanity impacted prevalence of illicit drug use among transgender veterans24.
Theme 2. Healthcare access and experience: This theme captures service access and use, cultural competency, variable quality of care as well as reporting on disclosure.
Service access and use Local availability of appropriate services was a key issue for rural LGBTIQ+ participants7,9,12,13,19,25,29,39-41,45-47,50,53,54,57-61,63-67. A lack of specialist gender services could mean long waiting lists and travel, which may be difficult to negotiate, particularly for young people without family support9,40,41,47,67. Suboptimal preventative healthcare practices were identified, including uptake in vaccination and screening for a range of general, sexual, and reproductive health concerns21,33,41. Even where care was available, the full range of services were not easily accessible for rural LGBTIQ+ populations; this would, for example, include where there was fear of discriminatory treatment from providers56, and where local providers would not prescribe pre-exposure prophylaxis (PrEP, a course of medication shown to reduce the risk of contracting HIV)13,21.
Cultural competency Participants highlighted the importance of cultural competency (knowledge and awareness necessary to provide appropriate care) on the part of providers7-9,12,13,20,21,25,38,40,41,44,47,50-52,54,56-58,61,63-65. Identifying knowledgeable providers may not always be easy, as demonstrated in Staunton-Smith et al (2019), where only 6 in a sample of 37 of primary health practices visibly displayed signs of a culturally inclusive LGBTIQ+ environment49. Insufficient provider knowledge relative to the concerns of rural LGBTIQ+ community members was reported7-9,12,19,38,40,44,57,59, including this being ‘out of their scope (p. 86)’9. This was mirrored in findings concerning healthcare providers’ knowledge and preparedness31,38,41-44,64.
Poor-quality care The majority of the included studies cited interactions between rural LGBTIQ+ community members and providers, which were characterised by explicit and implicit discrimination, stigma, and degradation7,9,19,20,29,42,52,56-58,64. This included instances where participants were exposed to detrimental attitudes and judgements9,12,47,50,61,64, breaches of confidentiality51,52, provider failure to support choices made51, refusal of services9,13,33,64, and invasive questions9,65. In many of these cases, community members were subjected to heterosexism and cisgenderism, which, among other means, was enacted in language (eg misgendering)58,64.
Good-quality care Participants valued inclusive, confidential, competent, and affirmative approaches that did not reproduce dominant and stigmatising paradigms via provider behaviour and language9,12,13,42,45,47,51,52,56,57. The benefits of a whole-of-person approach to care were expressed7-9, for example ‘trans healthcare is more than just hormones and surgeries (p. 438)’7. Additionally, it was appreciated when providers engaged in advocacy and facilitated connections with support systems8,9.
Disclosure Participants reported that they had not been asked about sexuality and gender by providers, as well as having few opportunities for disclosure20,53. Participants described navigating this process carefully, given the possible impact upon the relationship9,13,29,50-52,64,65. Previous reactions to disclosure were reported to shape this decision9,29,57, and a mixture of affirming and negative reactions were reported in studies20,53,62. A complex picture of disclosure emerged where, for some participants, it was a way to screen unsuitable providers, carers, or the care agencies they represent54, while others felt disclosure was not relevant to their care53.
Theme 3. Barriers: Reported within this theme are barriers concerning negative experiences and fear about future interactions, a paucity of available, appropriate services, financial and practical issues, as well as the challenges for providers.
Negative experiences and fear about future interactions Apprehension and fear about negative interactions with health services were cited as a barrier13,19-21,25,40,51,54,56-59,61,63-65. Future engagement with services is informed by previous negative experiences and, as a result, trust in health services requires rebuilding8,9,57.
Lack of available, appropriate services A lack of local, appropriate services emerged as a substantial barrier with implications for the wellbeing of rural LGBTIQ+ communities7-9,12,13,21-23,25,26,29,34,39,40,43,45-47,49-51,54,56-58,60,61,63-67. A lack of local, affirming, or, at a minimum, non-stigmatising providers of PrEP emerged as a critical issue in this review13,29,39, where, for example, lower urbanicity was strongly associated with increased odds of PrEP desert status for MSM39.
Financial and practical considerations The financial and practical considerations associated with travel are impediments to accessing care by LGBTIQ+ people, where appropriate services are not locally available (eg cost and logistics of travel)9,12,13,25,39,41,50,57,61,63,66,67. In addition, insufficient financial coverage and/or limited financial resources formed a barrier to accessing appropriate care8,9,13,19,40,54,63,64. This included, for example, whether insurance covers telehealth (care delivery of care via telephone, video-conference, and other internet-based platforms) specialist consultations63. Further, limited internet coverage in rural areas posed a barrier to accessing internet-based mental health services42,43,45,47,63.
Challenges for providers Deficits in relevant education, training, and support mean that providers are underequipped to provide quality care31,38,41-44. As an example, only 54.87% of primary healthcare providers in a US sample reported receiving education specific to LGBTIQ+ health during their professional degree program38, with a similar proportion of professionals indicating that they felt competent to provide LGBTIQ+ patient care in another sample44. Fewer appropriate local services could place a burden on providers9, where they may be professionally isolated61, have long waiting lists8, few appropriate options for referral9, and risk burnout9, which increases demand on already stretched services to support LGBTIQ+ communities, particularly during high-need periods such as created by the COVID-19 pandemic58.
Theme 4. Facilitators: Within this theme, education, training and support, the provider approach to care, resources, and new models and the role of support networks and community are identified and described as facilitators to health and health care.
Education, training, and support Education, training, and support helps providers deliver quality care to rural LGBTIQ+ communities7,9,19,21,31,38-44,50,53,57-59,65,67. Providers in several studies welcomed opportunities to learn more about LGBTIQ+ needs7,8,31,38,42,43 and were self-educated8,9. The importance of ongoing learning, support, training, and connections with other helpful providers in the community was reported19,31,42,43.
Provider approach to care Cultural competency and providers’ willingness to learn underpins quality care9,12,13,22,25,42,43,50,53,54,56,65. An explicit commitment to inclusive and affirmative care, which can take the form of visual signage, as well as being enacted in the language and behaviour of providers, is also valuable9,12,19,20,30,34,41,44,51-53,57,58,62,63,65. These may be especially important where community members are fearful or apprehensive about services, and could aid disclosure12,62. In addition to avoiding the reproduction of problematic heterosexist and cisgenderist assumptions and practices, participants reported the importance of holistic care, which promoted autonomy and aided community members to connect with support systems where desired8,9,13,19,20,22,42,52,59,65.
Resources and new models Models to enhance care were suggested: embedding a specialist within primary care practices8,9, creating pathways to streamline and regulate the assessment process for access to transition-related therapies7,60, and using peer advocates as paraprofessionals31,42,43. Telehealth could play a useful role by furthering the reach of services, supporting anonymity where desired, and combating isolation7,13,19,22,26,29,31,39,41,45,56-59,61,63,67. However, caution was urged about ensuring that these services complement, rather than replace, face-to-face services45,56.
Role of support networks and community Support from those closest to rural LGBTIQ+ people, as well as from social networks and the broader community, were considered important for wellbeing7-9,21,22,25,26,29,30,34,37,40,43,45-48,50,54,56,58-60,65 as poor community support can impact mental health and help-seeking29,34,48. The development of support systems including those with family, friends, and social networks was advocated for7,9,47,54, and providers can play a role in facilitating these connections8,9,19-23,31,34,42,43,58,59,67.
Discussion
We systematically reviewed recent evidence from peer-reviewed and grey literature to advance understanding of the wellbeing and healthcare experiences of rural LGBTIQ+ communities. Cumulatively, data from the USA, Australia, the UK, and Canada are reported, encompassing a range of primary care and specialist services, with representation of the experiences and views of LGBTIQ+ rural communities, as well as service providers. Overall, the included literature was deemed to be of good quality.
The first aim of the review was to examine the health of rural LGBTIQ+ communities. Consistent with previous findings10, rural LGBTIQ+ people face many of the health challenges experienced in the wider LGBTIQ+ community1-4. These challenges included the impact of co-morbid and chronic conditions41,46,47, challenges associated with substance use23,24,36,41, and managing HIV-related stigma and living with HIV in rural contexts30,46. Poor mental wellbeing, including experiences of depression, anxiety, and elevated psychological distress, and its interconnections with comfort in disclosing sexual identity, isolation, and loneliness, as well as deficits in community support, were noted26,34,37,40,48,58,59,61. A chief concern is that in rural communities there may be a lesser visible presence of LGBTIQ+ networks, as well as more identity concealment48, which, in turn, can limit access to support, including that from LGBTIQ+ peers47,48.
In examining healthcare experiences as the second aim of the review, suboptimal preventative healthcare access and practices were identified across general, sexual, and reproductive health domains13,21,29,33,41, which presents a pressing concern for the wider LGBTIQ+ community68,69. A lack of locally available, appropriate services, including specialist services, was observed and, even where present, rural LGBTIQ+ populations did not necessarily receive the full range of care needed13,21. Studies describing the experiences of LGBTIQ+ elders illustrated the interaction between rural contexts and wellbeing; elders encounter fewer LGBTIQ+-friendly provider choices and become socially isolated with decline in physical mobility and, potentially, independence25,46,50,54,57. While there has been rapid growth in LGBTIQ+ aging research, significant deficits remain70, and the development of policy and procedures to guide care as well as aged-care provider training are sorely needed71,72.
Congruent with best practice guidelines73,74, good-quality care was represented in the review as culturally competent, inclusive, confidential, and affirmative, where a whole-of-person approach was taken. In contrast, poor-quality care included discrimination (eg refusal of services), stigma, and demeaning interactions, often enacted in language (eg misgendering) or practice (eg breaches of confidentiality). These findings suggest that experiences with poor-quality care remain significant, ongoing issues for rural LGBTIQ+ communities. Consistent with Rosenkrantz et al10, identity disclosure could negatively impact healthcare interactions, and, in these current findings, LGBTIQ+ peoples’ assessments of identity relevance and the ways disclosure may enable screening of inappropriate providers capture the complexity and range of determinations inherent in clinical interactions. Greater attention to rural populations in the dedicated study of disclosure practices is vital75,76 to supporting the communities negotiating these interactions.
Many of the well-established barriers to wellbeing and health care are also reported for rural communities. Synthesis showed the way in which a lack of local service availability in rural areas is compounded by logistical and practical challenges. In light of this, access improvement initiatives ought to account for these considerations, including any necessary travel and limited internet coverage. Findings that captured service provider perspectives underscore deficits in provider education and training, and alert us to the need to address the pressures of high demand and the risk of professional isolation faced in rural areas8,9,58,61.
The provision of education, training, and support that is ongoing and connected with professional networks may be a means to mitigate some aspects of this barrier, including for paraprofessionals, such as those involved with peer support programs. Engaging in the types of high-quality care as previously described is regarded as a facilitator to care. A visible, explicit commitment to these practices would help affirmative services be more easily recognised by communities. The need to engage with new models of care, such as those that embed expertise and streamline processes, was evident7-9,31,42,43. An important insight concerned the potential of telehealth, especially internet-based approaches, to ease some of the burdens associated with a lack of local services. If enacted to complement in-person care, the careful integration of such services, including rural LGBTIQ+ community input and needs at the heart of its development, is recommended45,56. It was not surprising, given existing understanding77-79, that the development of support systems including family, friends, and social networks was viewed as key to wellbeing, and while this may challenging in rural contexts, providers can play a critical role in facilitating these connections8,9,19-23,31,34,43,44,58,59,67.
Limitations
While the abbreviation LGBTIQ+ is commonly used in the literature, the term does not fully capture the full diversity and range of identities and practices of the communities discussed in this review, who have nuanced and individualised experiences of health and health care. Further, this framing holds assumptions that may be unhelpful or problematic for certain groups including people who are intersex80. With the exception of one article49, findings concerning the experiences of rural intersex community members were from the grey literature, which indicates the need for in-depth consideration of the experiences of this population, employing a more relevant and sophisticated strategy. As such, the findings should be interpreted to indicate the range of possible shared issues and experiences encountered collectively.
The search was restricted to Canada, Australia, New Zealand, and UK and included only English language records. It is, therefore, possible that relevant studies may have been overlooked. The inclusion/exclusion criteria dictated that studies be excluded where it was not possible to distinguish between results concerning LGBTIQ+ communities and non-LGBTIQ+ communities; therefore, several studies that appeared in the previous review were excluded from the synthesis of the current review. Finally, the evidence encompasses a variety of health service contexts and, therefore, the general concerns about de-contextualisation in systematic reviews are relevant here, and findings should be interpreted accordingly.
Conclusion
This review reinforces that many aspects of the health and healthcare experiences of LGBTIQ+ are not unique to the USA and has served to provide further evidence and extend upon what is understood about these experiences. These findings indicate directions for future research efforts, including advancing evidence to guide policy and practice for aged care services in rural areas; investment in strategies to support rural providers; and the design, trialling, and evaluation of tailored models of care that account for rural barriers and harness existing capacities.
Acknowledgements
This research has been funded by the Department of Communities Tasmania’s LGBTIQ+ Grants Program 2020.



