Introduction
Rural generalist anaesthetists (RGAs) in Australia currently train for 4 years to gain general practice fellowship, with 1 year of this training time allocated to completing advanced skills training in anaesthesia. This year of anaesthetic training is overseen and examined by the Joint Consultative Committee of Anaesthesia (JCCA)1. The JCCA was formed in 1994 as a tripartite committee of elected representatives from the Royal Australian College of General Practitioners (RACGP), Australian College of Rural and Remote Medicine (ACRRM) and the Australian and New Zealand College of Anaesthetists (ANZCA)2. From February 2023, the JCCA will be superseded by the Diploma of Rural Generalist Anaesthesia (DRGA). Similar to the JCCA, the DRGA is a collaboration between the RACGP, ACCRM and ANZCA and is governed by a tri-college committee. (The DRGA curriculum is available at anzca.edu.au.)
RGAs are central to the delivery of elective and emergency anaesthesia and the acute care of critically unwell patients in much of rural and remote Australia. Without a well-trained RGA workforce of sufficient numbers, Australia would struggle to provide anaesthetic services outside of urban locations or make viable other crucial healthcare services that are reliant on anaesthetic support such as obstetrics, surgery, emergency medicine and critical care. RGAs also provide essential support to other rural doctors when managing critically unwell patients. As generalists, RGAs also bring added value to rural health services, working across a broad scope of rural medicine including general practice, palliative care, emergency medicine, aged care, Aboriginal health, paediatrics, general internal medicine and more.
The current policy of ANZCA is to support the delivery of anaesthesia by RGAs in areas ‘where there are no specialist anaesthesia services’3. Inherently, the wording of ANZCAs publicly articulated position on RGA service delivery raises questions about RGA practice. Most significantly, is anaesthesia delivered by RGAs less safe than that delivered by specialist anaesthetists? Due to the central role of RGAs in rural and remote health services, evidence detailing RGA training, volume of practice, scope of practice and service outcomes, would prove exceptionally useful. This data could be used for health service and workforce planning, and to drive clinical change or provide reassurance when aspects of RGA procedural practice are in question.
The process of reconciling what constitutes adequate training, safety, and the assessment of RGA practice is complex. Currently, data detailing the delivery and outcomes of anaesthetic services by RGAs are inconsistent and incomplete. Information is collected via numerous credentialling bodies, continuous professional development (CPD) programs run by several medical colleges, as well as by the many state, federal and private organisations that fund RGA services. Consequently, there is no single RGA data repository, making it difficult to reach reliable conclusions regarding the simplest of enquiries. For example, it is not officially known how many RGAs currently provide services in Australia. The closed Facebook page Rural Anaesthesia Down Under has collected the most comprehensive RGA demographics. A recently published estimate is that there are 568 RGAs4; however, the data are continually updated and now suggests there are 679 actively practising RGAs in Australia (Dr Greg Coates, pers. comm., December 2021).
Contemporary anaesthetics in health services in Australia and other developed countries are considered safe procedures5. Safety is an abstraction that does not exist as a discrete entity and is difficult to measure retrospectively, let alone to predict. It has been described in terms of patient indicators including the absence or minimisation of death, disease, disability, discomfort and dissatisfaction6. However, safety can also be described in terms of the structures and processes of risk avoidance and risk mitigation7. RGAs can be considered a structural (human resource) intervention to meet the challenge of the absence of specialist anaesthetists in rural health services. The authors are interested to consider how safety is measured, what discourse is occurring in terms of safety management and where the nidus of control lies in the rural health context. This article details a systematic review of the literature specifically asking the question, ‘What is the current evidence of the safety of anaesthesia delivered by RGAs?’
Methods
Literature relating to the safety of anaesthetics performed by RGAs published after 1950 as accessed using electronic literature databases (MEDLINE, Emcare, Scopus, Web of Science, CINAHL and Cochrane), which were searched using the following terms (PRISMA search protocol registration number CRD42018102883):
- Rural/non metropolitan – TI ( (rural* OR remote* OR region* OR "non-urban") ) AND AB ( (rural* OR remote* OR region* OR "non-urban") ) OR (MH "Hospitals, Rural") OR (MH "Medically Underserved Area") OR (MH "Rural Health Services") OR (MH "Rural Health") OR (MH "Rural Population")
- General Practitioners – TI ( (general practition* or GPs or physician* or nurse practition* or an?esthetist* or an?esthesiologist*) ) OR AB ( (general practition* or GPs or physician* or nurse practition* or an?esthetist* or an?esthesiologist*) ) OR (MH "Anesthesiology") OR (MH "Anesthesiologists") OR (MH "Nurse Anesthetists")
- Anaesthesia – (MH "Anesthesia, Conduction") OR (MH "Anesthesia, Dental") OR (MH "Anesthesia, General") OR (MH "Anesthesia, Intravenous") OR (MH "Anesthesia, Obstetrical") OR (MH "Anesthesia Induction") OR (MH "Anesthesia Recovery") OR (MH "Conscious Sedation") OR (MH "Neuromuscular Blockade") OR (MH "Premedication") OR (MH "Sedation") OR (MH "Premedication") OR (MH "Sedation") OR (MH "Anesthesia, Inhalation") OR (MH "Nerve Block") OR (MH "Anesthesia, Spinal") OR (MH "Anesthesia, Local") OR (MH "Anesthesia, Epidural")
- Safety – (MH "Patient Safety") OR (MH "Equipment Safety") OR (MH "Safety") OR (MH "Equipment Safety") OR (MH "Mortality") OR (MH "Child Mortality") OR (MH "Infant Mortality") OR (MH "Maternal Mortality") OR (MH "Fatal Outcome") OR (MH "Hospital Mortality") OR (MH "Adverse Drug Event") OR TI ( (safety* OR "adverse event*" OR mortalit* OR morbidit*) ) AND AB ( (safety* OR "adverse event*" OR mortalit* OR morbidit*) ) OR (MH "Risk Management") OR (MH "Quality of Health Care") OR ( ("risk manag*" OR quality*) )
Inclusion criteria for articles included that they were written in English and involved human subjects. Search results were imported into the citation management system Endnote vX9.3.3 and duplicates were removed. Title and then abstract of each article were screened and articles excluded if they were not relevant to the four search enquiries as above. Titles were reviewed of the references from these initial articles and relevant articles included in the literature review process.
All included references underwent critical appraisal using The Joanna Briggs Institute suite of critical appraisal tools (https://joannabriggs.org/critical_appraisal_tools). Each article was appraised independently by authors PG and LW. Articles were judged independently on a Likert scale of ‘very low rigour’ to ‘very high rigour’. The results were then compared and where discrepancies occurred a judgement of rigour was made by consensus.
A thematic analysis of the articles was conducted by PG. As the lead researcher undertaking this literature review, PG is a practising RGA who is also involved in the selection, training, education and support of both trainee RGAs and practising RGAs. As an informed insider, PG’s professional experience shaped the analysis. Several articles were read aloud by the team to develop an initial qualitative analysis grid8. This coding grid was used to analyse each journal article in turn, with new content areas brought to the group for exploration and sense-making. Further codes were developed through consensus. Themes were derived from findings that emerged across a number of studies. Themes were further refined by PG following further group critical discourse. When complication rates were included in an article and urban comparisons were not provided, the author sought contemporaneous Australian urban comparisons.
Results
The initial database searches found 22 765 articles (final search November 2021), and the number was reduced to 12 458 after duplicates were removed (Fig1). Following 12 403 articles being excluded by title, 55 abstracts were reviewed and 13 articles were included: 12 in the initial process and then an additional one article found from the references of the original articles.
Ten articles were from Australia9-18, with two from Canada19,20 and one international study21. Most articles were published after 2001, used clinical audit or surveys and were of moderate to high rigour (Table 1).
None of the reviewed studies provided a definition of ‘safety’; rather, it was inferred that safety was understood by the reader. ‘Quality’ and ‘safety’ were often used synonymously in the articles reviewed. Five themes were identified from the reviewed articles:
- appropriate training and leadership9-13,15,17,21
- rates of complications11-14,19,20
- volume or scope of practice12,13,16
- availability of equipment10,15
- case selection10,13.
For each of the five themes, the articles are discussed in near chronological order. This reflects the evolution of rural generalist anaesthetic practice.
Table 1: Characteristics of publications included in the literature review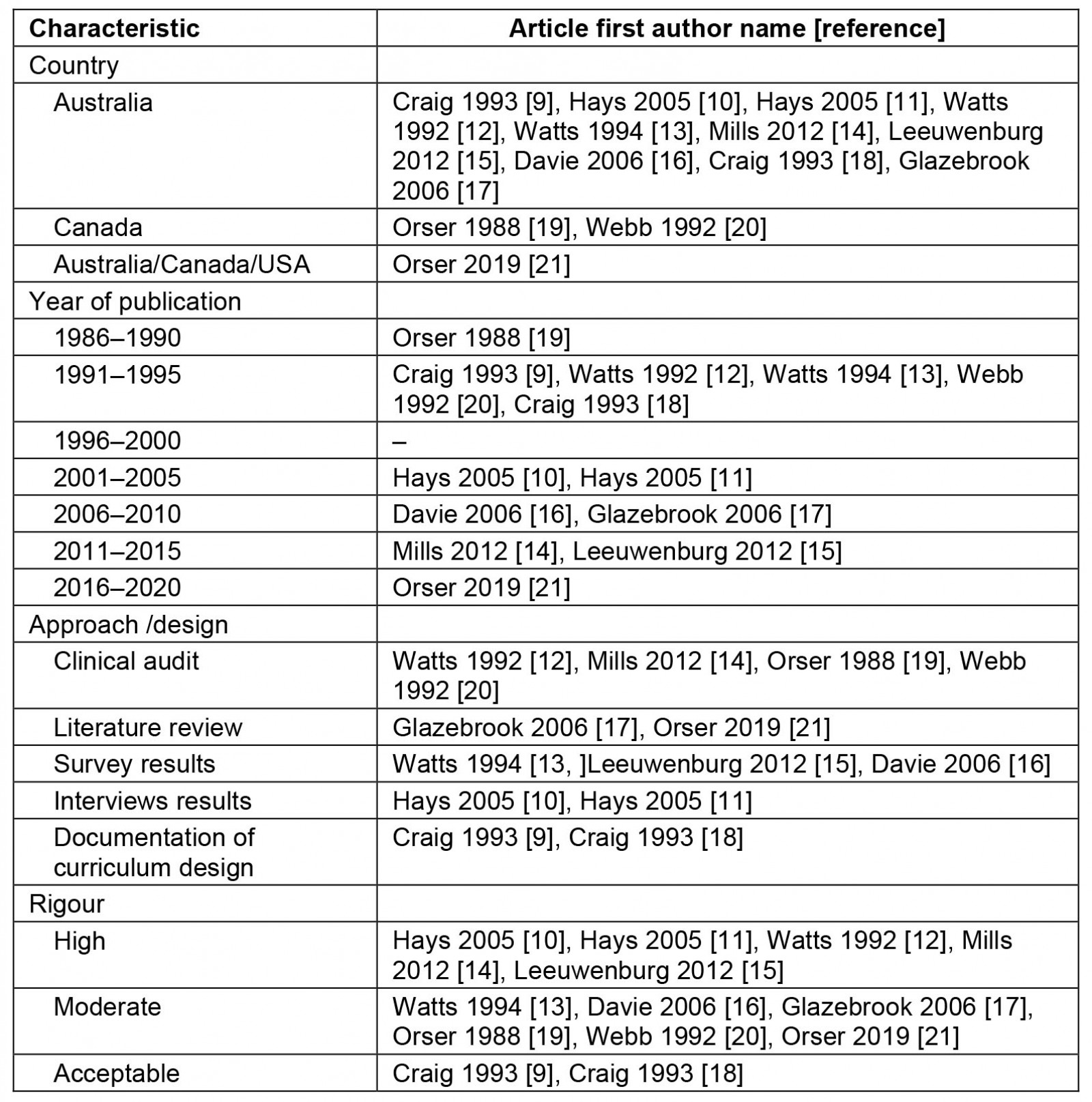
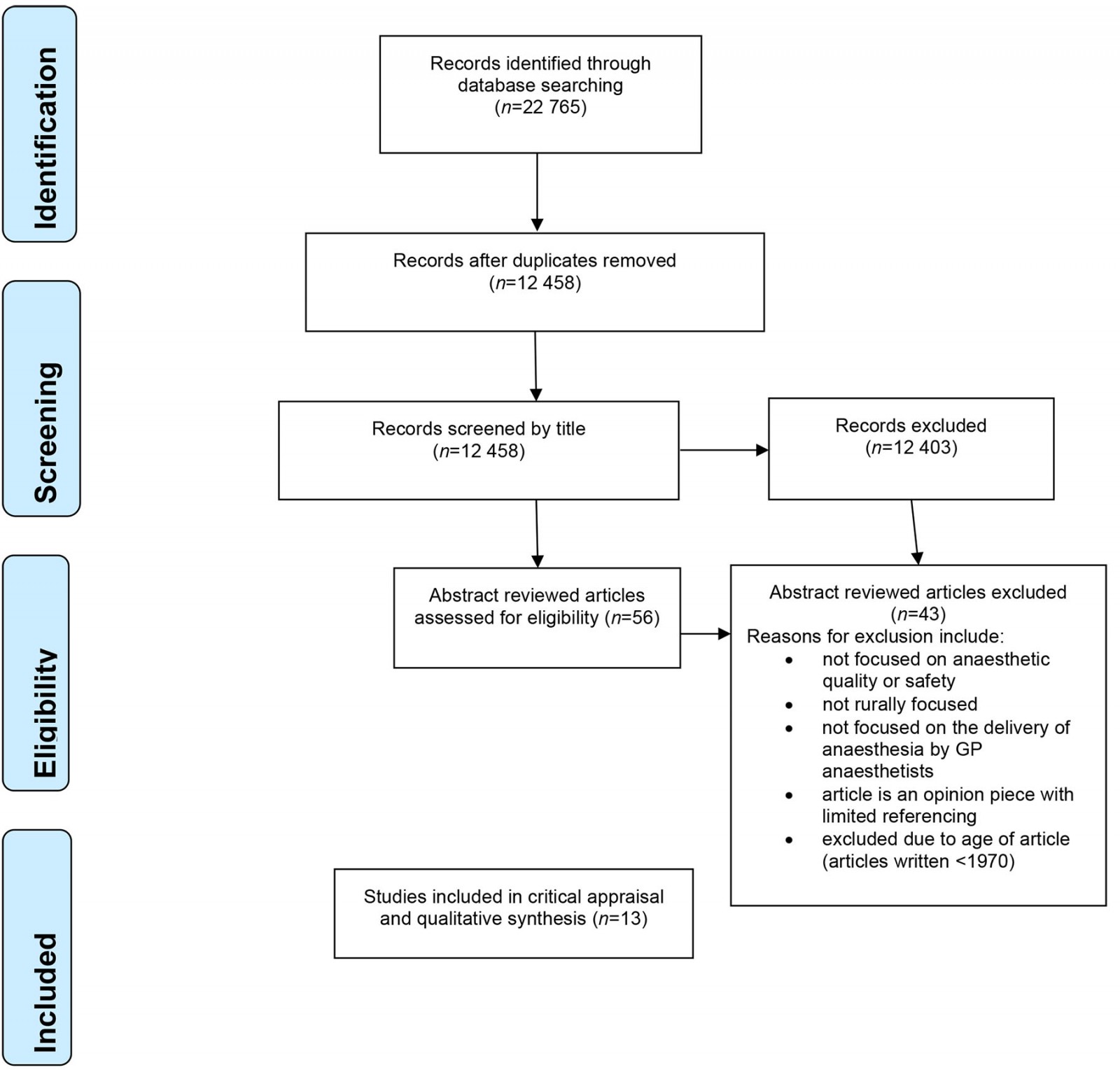 Figure 1: PRISMA flow chart.
Figure 1: PRISMA flow chart.
1. Appropriate training and leadership
Eight articles considered the link between training or CPD and safe anaesthetic practice. In relation to initial training, a 1994 study found a mean training time of 7.5 months, with most respondents receiving training at a level ‘too junior’ for subsequent independent practice13. This sentiment was supported by a rural doctor survey in 1992 in which respondents felt they had ‘inadequate preparation for rural practice’, particularly in procedural areas18. No studies identified optimal training time for GPs wanting to deliver rural anaesthesia. In Australia the 1994 Rural Medicine Curriculum design project created a framework for a 12-month GP anaesthetist (GPA) training program. Although two of the formal learning objectives had a specific focus on safety including demonstrating skills for safe practice and adaptability to change in anaesthetic practice, the link between training and safe procedural practice was not subject to appropriate evaluation9,17.
Five articles considered continuing professional development of GPAs10,11,15,17,21. Trained and experienced medical and other health professional staff were recognised as required to ensure that there was little ‘difference in the quality of that care provided when compared with care expected in urban hospitals’10. A parallel reference by the same authors concluded that ‘how technical competence is maintained’ is an important determinant of quality in rural health care11. Both recency and content of training were recognised as important, with one study describing that 71% of GPA respondents (n=209) had accessed anaesthetic upskilling within the previous 12-month timeframe while only 44% of respondents had accessed a specific difficult airway course within a previous 3-year timeframe15. Barriers identified included distance to training and lack of locum cover. These were consistent with barriers identified in a 2006 literature review that specifically looked at obstacles to the maintenance of advanced procedural skills for rural and remote practitioners in Australia17. In relation to training, one reference recommended ‘locally delivered courses aimed at not just GPAs, but also associated health staff, particularly nursing staff in rural operating theatres and emergency departments’15.
One reference approached the provision of safe anaesthetic care from a leadership perspective and from the assumed position that specialist anaesthetists were ‘ultimately responsible to facilitate access to high quality care’21. This 2019 reference was written by a multinational team and provides a summary of the literature, the current situation and recommendations for the future of rural and remote anaesthesia in affluent countries, specifically Australia, Canada and the USA. It highlighted that ‘rural and remote settings do not provide the volume or complexity of cases required to attract and retain a highly specialized physician workforce’. Consequently, the authors urge a collaboration between all care providers to ‘provide timely access to safe anaesthesia’ and offer solutions under four broad headings21:
- flexible work arrangements – including specialist outreach programs to support the continued practice of non-specialists
- formal networks of care to encourage collaboration between specialists and non-specialists. Quality, including outcomes, would then belong collectively to the region
- clinical coaching by specialist anaesthetists of ‘other care providers’ in rural locations
- telemedicine to facilitate greater specialist involvement in the delivery of rural and remote anaesthesia and pre-operative evaluation of surgical patients.
The authors conclude that these solutions will ‘strengthen and stabilise’ anaesthesia care teams in rural and remote regions. However, there is no discussion on potential challenges or drawbacks with the recommendations.
2. Rates of complications
Six of the thirteen references in this review discussed complication rates (Table 2). Comparisons between studies prove complex due to layering of confounding factors. Confounding factors include, for example, the location of the study (rural or remote, emergency department or theatre), the anaesthetic technique examined, equipment used and the clinical experience of the study participants.
A 1994 survey of South Australian GPAs13 reported a failed intubation rate of 50/10 000, which was described as higher than the comparison rate reported in this study of 5–35/10 00013. Although this finding seems to suggest significantly greater complication rates, it is not clear whether the definition and reporting processes for the study differed from the collection methods of the comparison data.
Complication rates of 116 epidurals performed over a 10-year period (1974–1983) by non-specialist rural anaesthetists were reviewed by Orser 198819. This retrospective audit found a major complication rate of 16.3% versus 4.2–10.5% reported from two other contemporaneous references (1973 and 1983) that studied labour epidural anaesthesia at university and community hospitals19. In this instance, a major complication was defined as any of the following: dural tap, punctured vessel, toxic reaction, hypotension, paralysis, transient paraesthesia or subarachnoid injection19. In stark comparison to the 1988 Orser review, Watts’ 1992 study12 was a prospective audit of 324 epidurals performed over a 5-year period (1986–1991) by a single practitioner in rural South Australia. The author reported no major complications although the definition of what constitutes a major complication is unclear. The total complication rate was 18.7% of the obstetric epidurals reviewed. This study collected information on all obstetric epidural complications and listed them as failure, blood in catheter, dural tap and difficulty feeding the catheter. The incidence of complications for non-obstetric epidurals was 17%, and complications were listed as failure, dural tap, headache, hypotension (systolic blood pressure <90mmHg), pain on injection and dizziness. Watts reported that the incidence of dural tap, blood in the catheter and failed epidurals compared favourably to other studies. The incidence of maternal hypotension of 24.6% was compared to a study by Crawford et al 1986, which used the same parameters to define maternal hypotension and reported an incidence of 14.6%22. Interestingly, maternal hypotension doesn’t appear to be considered either a major or minor complication in the study design. Webb and Kantor 1992 reported a complication rate of 23% when retrospectively auditing 225 epidurals performed over a 5-year period in a rural Canadian hospital20. Hypotension occurred in 12% of patients, while the dural puncture incidence was 1.8%. The above audits were undertaken more than 27 years ago. They were done at a time when there was no formal training in anaesthesia for family physician anaesthetists in Canada or for rural GPs in Australia.
A 2012 retrospective audit by Mills and Newbury of 889 consecutive episodes of anaesthesia delivered over a 5-year period (2006–2010) in the hospital of a small, remote town in South Australia documented no perioperative deaths, and the researchers found 16 intraoperative and 7 postoperative problems documented in the anaesthetic records14. A difficult intubation rate of 1% compares favourably to 1993 Australian Incident Monitoring System data, which cited an incidence of 4%. Similarly, the rate of hypotension and hypertension of 0.34% compares well to that of a 2008 study that reviewed adverse physiological events during 3790 anaesthetics and found an incidence of 1.77%. This may reflect careful case selection by the anaesthetists as 95% of patients were American Society of Anesthesiologists (ASA) physical status I or II, and 51% were aged between 5 and 50 years. Despite the limitations of a retrospective audit with small sample size, these findings indicate that a GP can provide safe anaesthesia in a small, remote hospital14.
Hays et al undertook a series of interviews with patients, their families and rural healthcare workers that considered the quality of procedural rural general practice11. The authors proposed three determinants of quality in procedural rural medical care:
- structural – staff, equipment, space, consumables
- process – equity of access, convenience, cultural appropriateness, technical expertise
- outcome – patient satisfaction, cost, patient functionality, complication rates.
Complication rates were considered a key component of the outcome determinant.
Table 2: Summary of complication rates with contemporaneous comparators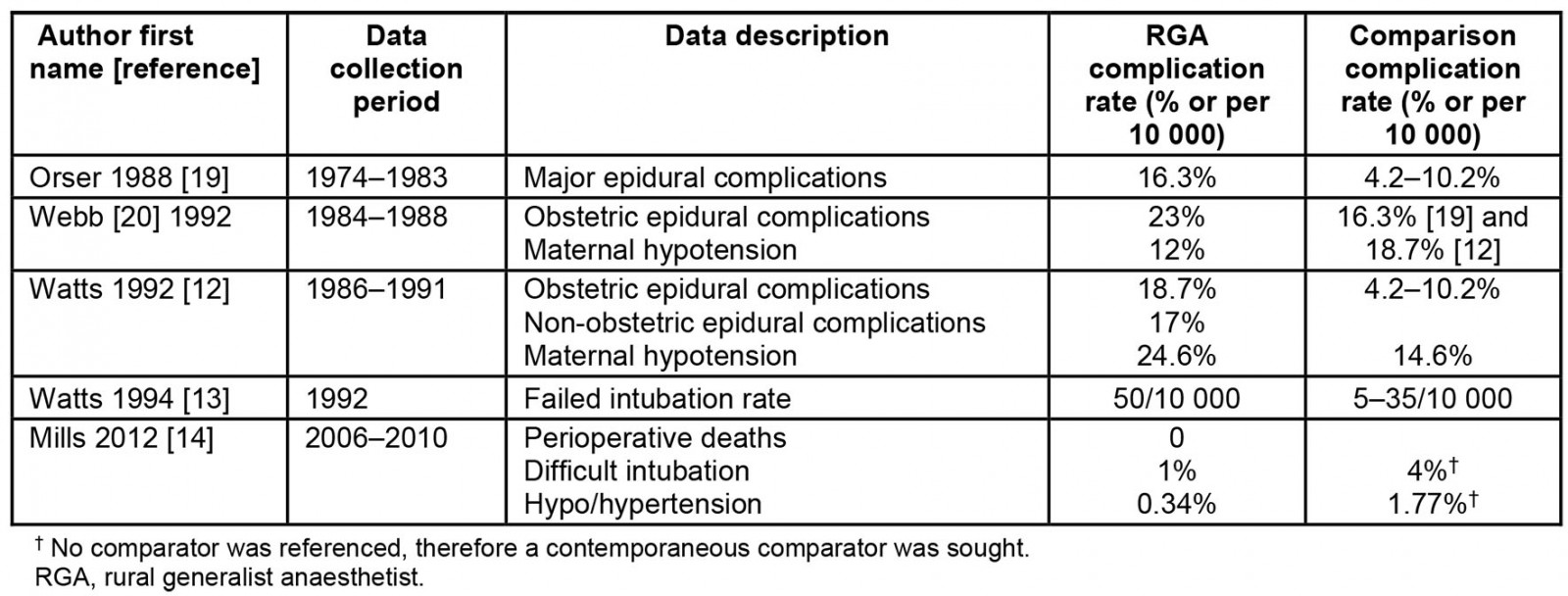
3. Volume and scope of practice
A 2006 survey performed by Davie focused on the work practices of Australian GPAs who undertake the JCCA Maintenance of Professional Standards Program. This research documented self-reported scope of practice and volume of practice16. The article did not express any opinion regarding appropriate caseload or scope of practice. Davie found that 18.9% of respondents were administering >500 anaesthetics per year, 51.8% undertook 151–500, 11.6% 101–150, 17.7% of respondents were administering 100 or fewer anaesthetics per year, with 3.6% reporting less than 25. Sixty four percent administered epidurals, which was comparable to a 1996 survey of Western Australian GPAs16. The mean minimum age of paediatric anaesthesia was 4.1 years. This age was higher than the 1996 survey of Western Australian GPAs. Only 4% reported that they had no minimum age for elective paediatric surgical patients as compared to Watts and Bassham (1994), who reported 46% of GPAs were providing anaesthesia to patients in the 0–12-month age range13. These findings suggest a significant change in either rural surgical practice or GPA practice over 10 years from 1994 to 2006, with greatly reduced early childhood anaesthesia performed by Australian GPAs.
Watts’ 1992 study prospectively reviewed the administration of 324 epidurals over a 5-year period12. The author concluded ‘this study shows that a GP anaesthetist with twelve months’ training, performing one to two epidurals per week can provide a safe and effective epidural service’.
A visual analogue scoring system was used by Watts and Bassham (1994) to determine how comfortable GPAs were in the provision of anaesthesia13. The study found that GPAs with higher anaesthetic caseloads felt more comfortable providing anaesthetic services. The authors concluded that ‘those GPs who practice infrequent anaesthesia or feel very uncomfortable doing so would be advised to stop’. Furthermore, the authors made the judgement ‘It is inappropriate that 46% of GP anaesthetists provide anaesthesia for the 0 to 12 months paediatric age group and such services must be rationalized’. This statement appears to be based on the assumed high-risk nature of anaesthesia in this age group without discussion of case selection.
Mills and Newbury’s 2012 audit reviewed 889 consecutive anaesthetic events delivered predominantly (98%) by four resident RGAs at a rural South Australian hospital over a 5-year period14. This audit reported that 89% of anaesthetic events (n=790) occurred in patients with an ASA physical status of I or II. Determining the ASA rating of patients is important for both RGA case selection and scope of practice. Emergency surgery occurred in 6% (n=50) of patients with an ASA physical status of I or II. The remaining 5% (n=49) were patients with an ASA physical status of III. No ASA III patients had emergency surgery in the 5-year period of the study. In relation to paediatric anaesthesia, 8% (n=67) were aged <5 years, 9% were aged 5–15 years and 83% were aged >15 years. Within the limits of a retrospective audit, the anaesthetic complication rates were favourable compared to other contemporaneous studies (see section ‘Rates of complications’).
4. Availability of equipment
Hays et al (2005) specifically referenced ‘necessary equipment that is maintained’ as a key component of the structural determinant of quality of rural procedural practice11. Other than a reference to anaesthetic machines, the authors did not expand further on what was meant by ‘necessary equipment’.
A 1994 survey of 76 (of an estimated 92) South Australian GPAs explored approaches to potentially difficult anaesthesia13. The survey included access to different types of monitoring equipment and found 100% had access to pulse oximetry and continuous ECG monitoring, 85% had access to capnography, 73% to automatic non-invasive blood pressure and 37% had access to a nerve stimulator. Of significance is that all these monitoring systems are now mandatory in hospitals across Australia.
One of the most contemporaneous pieces of research that looked at access to equipment was undertaken by Leeuwenburg 201215. The author surveyed 293 rural GPAs across Australia and specifically looked at the availability of equipment in rural hospitals for the management of difficult airways. This study was primarily concerned with GPA access to difficult airway equipment considered mandatory by ANZCA in Technical Document T01 (since superseded by PS5523). The author found that 53% of survey respondents did not have access to a difficult airway trolley, despite well published algorithms that detailed the equipment needed for this potentially life-saving equipment.
5. Case selection
Watts and Bassham 1995 stated that ‘Rural GP anaesthesia is an area of anaesthetic practice which requires particular skill in case selection’13. They reported that ‘most’ GPAs surveyed would avoid anaesthetising ASA III–V patients, patients with severe asthma, unstable angina, morbid obesity, renal failure and known anaesthetic risk factors. In looking at the quality of rural procedural practice, Hays et al recognised that case selection was an important caveat to their conclusion that ‘rural medical procedural care can be of an acceptable quality’10. Mills and Newbury’s 2012 audit attributed the low rates of anaesthetic complications found in their study to case selection and a number of organisational factors14.
Discussion
The training of rural GPs to undertake procedural work has always focused on increasing access to safe procedural medical care for rural and remote patients, especially in high-risk areas such as surgery, anaesthesia and obstetrics3,9,11,17,24-26. The available literature that examines the safety of anaesthesia delivered by RGAs can be grouped into five themes.
In a 1992 survey of rural doctors, a common theme that emerged was a feeling of ‘inadequate preparation for rural practice’27. This report held enough weight at the time to be a key impetus for the Rural Medicine Curriculum Design project9, which ultimately led to the formation of JCCA in 1994. Today, the JCCA is responsible for supervising and examining rural GPs and rural GP trainees who are undertaking 12 months of training in anaesthesia as an advanced skill1.The JCCA curriculum has been revised multiple times since its development and is currently in its sixth edition28. Safety is a strong theme of the curriculum and is directly and indirectly referenced in its 35 learning outcomes. Curricula revisions have occurred in response to changes in educational practice, for example the development of learning outcomes. The curriculum has also changed in response to advances in anaesthetic technology, for example improved monitoring equipment and ready access to equipment such as computerised anaesthetic machines, ultrasound and video laryngoscopes.
Since 1994, to the detriment of the profession there has been a distinct lack of peer-reviewed research addressing the question of whether rural doctors now feel ‘adequately prepared’ for rural practice. Attempting to answer this question is complicated by two additional issues. First is contextual differences in each rural or remote centre including staffing, systems, physical resources, available equipment, patient demographics and community resources29-31. Second is a lack of clarification about how clinical training for rural practice should be assessed, measured or monitored to determine if it is adequate.
Anaesthetic safety is difficult to quantify as trainees gain skills and become progressively more independent7,32. For RGAs this is especially complex as they transition from urban centres or regional practice to more rural and remote practice. The lack of empirical research makes it difficult to draw a direct line between initial training and improved patient safety in the rural context33,34. This has allowed risk-averse, urban-centric social, political and administrative forces to shape RGA training32.
In line with contemporary educational practice, there is a clear need for the future of RGA training to focus on development of a competency-based training program35,36. The use of more tools such as entrustable professional activities37 and a suite of workplace based assessments could be excellent starting points36,38. Failure of non-technical skills are frequently implicated in patient harm39,40. Lynch (2020) describes non-technical skills as (i) social skills including communication, teamwork, leadership; (ii) cognitive skills including decision making and situational awareness; and (iii) personal resource skills including managing stress and coping with fatigue40. Future RGA training curricula could have a specific focus on the development of non-technical skills. Any of these potential changes to RGA training need careful evaluation to ensure that rural patient safety is improved.
In Australia, RGAs are subject to a triennial compulsory CPD program. The CPD requirements for RGAs were implemented by the JCCA as a result of recommendations made by the Victorian Coroner in 2016 in the wake of the tragic death of 42-year-old Delta Poke41. Mrs Poke presented to an urban Victorian day surgery in 2011 for a second-trimester termination of pregnancy. She suffered a cardiac arrest during her anaesthesia and sadly passed away due to global cerebral ischaemia. The Victorian Coroner found that the urban GPA responsible for Mrs Poke’s care should have completed a full set of vital signs including obtaining oxygen saturation level prior to delivering the anaesthetic and that this represented ‘a gross departure from accepted clinical practice standards’, which ‘contributed to the cause of Delta’s death’41. Although several systems issues were identified in the coronial inquest, the Victorian Coroner did not make any recommendations directed at the facility and concluded that these did not contribute to Mrs Poke’s death. Through the process of this coronial inquest the fact that there was a lack of anaesthetic specific CPD for GPAs was highlighted. This resulted in the Coroner making a specific recommendation calling for the JCCA to implement a CPD program. These changes came into effect for the 2017–2019 CPD triennium42 with the aim of improving anaesthetic safety and promoting the professional standing GPAs41.
The impetus for the development of the current JCCA CPD program appears to have occurred in response to a single, albeit tragic, event and the conduct of a single, urban-based GPA. This raises questions about the factors that shape standards and education for the entire cohort of Australian RGAs. Future research is needed into the RGA CPD program. This research could focus on the achievement of stated CPD aims and ensuring the program is fit for a rural and remote context. Important issues to address could include barriers to CPD access, multidisciplinary involvement in CPD and in-situ team training that is tailored to locally available resources and adherence to the relevant ANZCA Professional Services documents. Additional to this is ensuring a focus on the development of non-technical skills40.
Serious adverse outcomes in anaesthesia are relatively low in frequency. For example, the latest ANZCA Safety of Anaesthesia Report details 239 deaths from 13.65 million anaesthetic events (1/57 112) in the 3-year period 2015–2017, and this figure has remained relatively constant over the previous four trienniums5. In the 2015–2017 triennium, 90% of the deaths (215) involved specialist anaesthetists, 5.4%13 involved trainee anaesthetists, and 4.6%11 are classified as ‘other’. In previous ANZCA Safety of Anaesthesia reports, there were three further categories: ‘not reported’, ‘no anaesthetist in attendance’ and ‘GP/non specialist anaesthetist’. Therefore, of the 11 deaths attributed to ‘other’, it is not clear in how many anaesthetic-related deaths was an RGA the principal anaesthetist. Furthermore, it is not known is how many anaesthetic events GPAs or RGAs were responsible for delivering anaesthesia in this period. It follows on that studies with relatively smaller numbers, such as those identified in this review, are unable to elucidate the likelihood of rare events, let alone the identification of contributing factors and how to judge whether incidents were potentially preventable7.
Comparing complication rates between the published studies is tempting; however, there are multiple critical junctures where numerous clinical decisions can be made in any given anaesthetic technique. These junctures include, for example, the location of the procedure, the type of procedure, choice of equipment, choice of agents and dosing of agents. In addition, decisions relating to study design create a second layer of confounding factors including, for example, different definitions of what constitutes a complication, the specific purpose of the research and whether anaesthetic complication was a primary or secondary focus, the make-up of the research team and the personal and professional experiences each member brings to the team, the research methods employed, and the resources available to the research team.
This article demonstrates that retrospective comparison of complication rates is complicated. The research currently available relating to RGA complication rates is insufficient to make any meaningful evidence-based assertions. If rates of complications are to be used as a surrogate marker of the safety of RGA practice, prospective, high-volume clinical audits are needed. Given the inherently low volume of many rural and remote anaesthetic services, this may require multiple comparably designed smaller studies to be merged.
It is crucial for rural anaesthesia research to consider the multifarious nature of RGA contexts and the inextricable role that context has in shaping RGA practice. In relation to patient safety, RGAs are continually balancing the tension between patient safety and patient access to medical care. This tension causes rural generalists to push themselves to the limits of their scope of practice and has been termed ‘clinical courage’43,44. It would be valuable to assess and understand how RGAs provide leadership in the management of safety and the mitigation of risk in rural anaesthesia clinical practice. ANZCA is considered the anaesthesia content expert; however, RGAs possess the context expertise and an adaptive expertise required to provide generalist health care to their communities. The recommendations made by Orser et al focus on facilitating rural anaesthetic service leadership by urban specialist anaesthetists21. Furthermore, they state that ‘ultimately, we believe that it is the responsibility of specialist anaesthesiologists and academic health science centers to facilitate access to high quality care’. Orser and colleagues recently published the outcomes of a 2020 symposium45. This article further develops the concept of providing anaesthetic networks of care and articulates a clear desire for community-led solutions. Rural context is highly nuanced, therefore should we be seeking local leaders regardless of their specialist or generalist qualification, rather than presuming leadership will come from specialist urban centres?
Ongoing caseload refers to the total number of anaesthetic cases in any given period, usually 12 months. Appropriate scope of practice refers to the caseload mix and includes patient factors such as age and ASA classification, the range of surgical cases anaesthetised, the range of anaesthetic techniques employed, the range of airway management techniques employed, and supplementary procedures performed (eg fibreoptic intubation, insertion of arterial lines, insertion of central venous catheters). The results of this scoping review suggest that the majority of RGAs embark on procedures, for which they are appropriately trained, on patients deemed safe to have a specific procedure in a particular rural locale12-14,16.
The study findings highlight the unique nature of two concepts: that of ‘a safe practice’ and that of ‘a safe profession’. Medicine as a profession is inherently urban-centric and there is an entrenched and growing investment in specialisation that focuses on depth rather than breadth of care46,47. Specialisation enables individual practitioners to limit their scope and increase the depth of expertise in a focused area, hence limiting risk. The health benefits of specialisation are now less than the health outcomes foregone by its inherent inflexibility47,48. In contrast, rural medicine is highly dependent on, and invested in, both generalism and integrated interdisciplinary practice23,49,50. The cultural shift in medical practice toward specialisation influences how generalism is viewed, and that an extra level of skepticism is imposed on rural settings because they are further removed from what are considered to be progressively concentrated urban centres of excellence. The findings of this study demonstrate the need to consider the safety of RGA practice within the context of ensuring patient access to care, while managing with limited human and physical resources to provide safe anaesthesia in rural and remote communities that cannot support specialist anaesthetists. Future research in this area could focus on what is the optimal standard of care in a particular rural and remote context. This is, potentially, another extensive area of research.
It is an ongoing cause of concern to the RGA profession that an urban-centric view informs what is considered safe practice without regard to patient access. Concerns about what constitutes an appropriately safe scope of practice for RGAs continue to be raised. Examples of decisions that have been made in rural locales include the cessation of the following: elective anaesthesia to children under 10 years of age, caesarean sections requiring a general anaesthetic, and elective anaesthesia to anyone with a body mass index above 40. Decisions in health care with limited evidence, underpinned by ‘safety concerns’ hold gravitas7,10,11. These decisions can often have a profound impact on the provision of health care in rural communities.
A key body of future research would be to describe RGA geographical areas of practice, and their scope and volume of practice, via a nationally consistent clinical audit. This information would prove useful for state, territory and federal agencies that are responsible for rural healthcare workforce planning and service delivery.
Inequities in health care between metropolitan centres and rural and remotes areas of Australia have been well established in the literature17,23,49-51. Given the inherent high-risk nature of anaesthesia, one would imagine that equipment designed to deal with adverse outcomes or complications would be readily at hand. However, the references included in this review suggest otherwise. As the most contemporaneous research in this area was 201215, updated data is required to identify areas of need and foci for equipment training and development.
Case selection is arguably one of the most important skills for RGAs. It is a complex decision-making process that considers patient factors, surgical factors, facility factors and individual RGAs’ personal factors before making the final decision to proceed, refer, defer or cancel the proposed surgical procedure. Several of the references referred to the importance of case selection; however, there were no references identified in this review that explored the process of case selection by RGAs. It would be extremely valuable for health services and credentialling bodies to understand and respect the decision-making process undertaken by RGAs when assessing individual patient fitness for anaesthesia. Outcomes of such a body of work could include frameworks that support contextualised decision making. If done carefully, the process of implementing such frameworks in individual rural and remote hospitals would stimulate valuable discourse among key staff.
Conclusion
The current thin evidence in relation to the outcomes of RGA practice has allowed anecdote to characterise the profession4, leading to generalisations being made about RGAs based on isolated cases. This has led to an image of RGAs as poorly trained, risk-taking practitioners. Further peer-reviewed evidence is required to ensure safe, affordable health care for people living outside of urban locations leading to minimise the gap in emergency and surgical outcomes for rural and remote Australians.



