Introduction
There has been an increase in the frequency and magnitude of disasters and emergencies in recent years. Research has estimated a 60% increase in disasters worldwide, resulting in 2 million deaths, 4.2 million injuries, 33 million homeless people, and 3 billion people affected1-3. The recent Ebola outbreak in West Africa and the ongoing COVID-19 pandemic are examples of serious recent disasters that affected many countries in Africa, and highlight the need for effective preparedness interventions across sectors.
Disaster preparedness encompasses all measures taken before a disastrous event that aim to minimize loss of life, disruption of critical healthcare services, and damage when a disaster occurs. These measures include the development of emergency response plans, effective warning systems, maintenance of inventories, and training of human resources for effective disaster management3-6. Arguably, nurses, as the largest group of the healthcare workforce particularly in rural contexts, are often on the frontline in disaster management, providing care to patients with emerging physical, mental, and emotional turbulence, and acting as educators for health promotion and disaster prevention3,4,7-9. However, current evidence indicates that they are inadequately prepared to respond to disasters7-9, and disaster preparedness/management appears to be a novel specialty for nurses.
Although the healthcare system is an important entry point for disaster response, limited research has explored disaster preparedness in Tanzania. A recent study by Koka et al10 acknowledged the existence of disasters in Tanzania that contributed to disabilities, infrastructure destruction, and loss of life; 92% of regional hospitals had experienced disasters in the past 5 years, including large motor vehicle accidents, floods, and infectious disease outbreaks. However, the results indicated disaster preparedness was inadequate in regional hospitals. Specifically, the issue of nurses’ preparedness for disaster response in primary healthcare (PHC) settings in Tanzania remains unclear, although they comprise the majority of the hospital workforce (eg 5390 nurses vs 830 doctors with 214 nurses vs 27 doctors per hospital)10. Furthermore, a quick scan of nursing school curricula indicates that disaster preparedness and management are not covered. To address this knowledge gap, this study examined nurses’ preparedness for disaster response in PHC settings in rural and urban Tanzania.
Methods
Design
This was a qualitative descriptive study involving qualified nurses and nurse administrators working in rural and urban PHC facilities in Tanzania. Descriptive design was selected because it is an appropriate design to answer the key research questions and to develop an understanding and description of a phenomenon (disaster response and preparedness) without testing an existing theory.
Study population, sample size, and sampling method
Thirty-one purposefully selected nurses and nurse administrators from PHC facilities were interviewed to facilitate data source triangulation. Although equal representation is not a primary focus in qualitative studies11, facility level (dispensary, health centers, and district hospitals) was considered during participant enrollment. Eleven nurses and nurse administrators in urban areas in Dar Es Salaam were selected to participate in this study. Given that disasters are also common in rural areas, 20 participants working in Shinyanga were selected as rural participants. No gender or age preferences were set for this qualitative inquiry other than nurses/midwives who had worked in healthcare settings in Dar Es Salaam or Shinyanga for at least 2 years, to increase the likelihood of them having experienced a disaster situation.
Participant recruitment
This study used telephone-based interviews to collect data from nurses and nurse administrators in PHC facilities. The telephone interviews aimed to reduce the cost of face-to-face interviews and took advantage of remote interview technologies, the use of which increased during the recent COVID-19 pandemic. Recruitment for the interviews was as follows. First, telephone numbers for prospective participants were obtained from the Nursing Council registry and peer referrals. Next, a short message (SMS) containing information about this study and an invitation to participate was sent to potential participants. Those willing to participate were asked to reply with their preferred time and date for an interview. Information about the study was also shared through professional WhatsApp groups.
Data collection tool
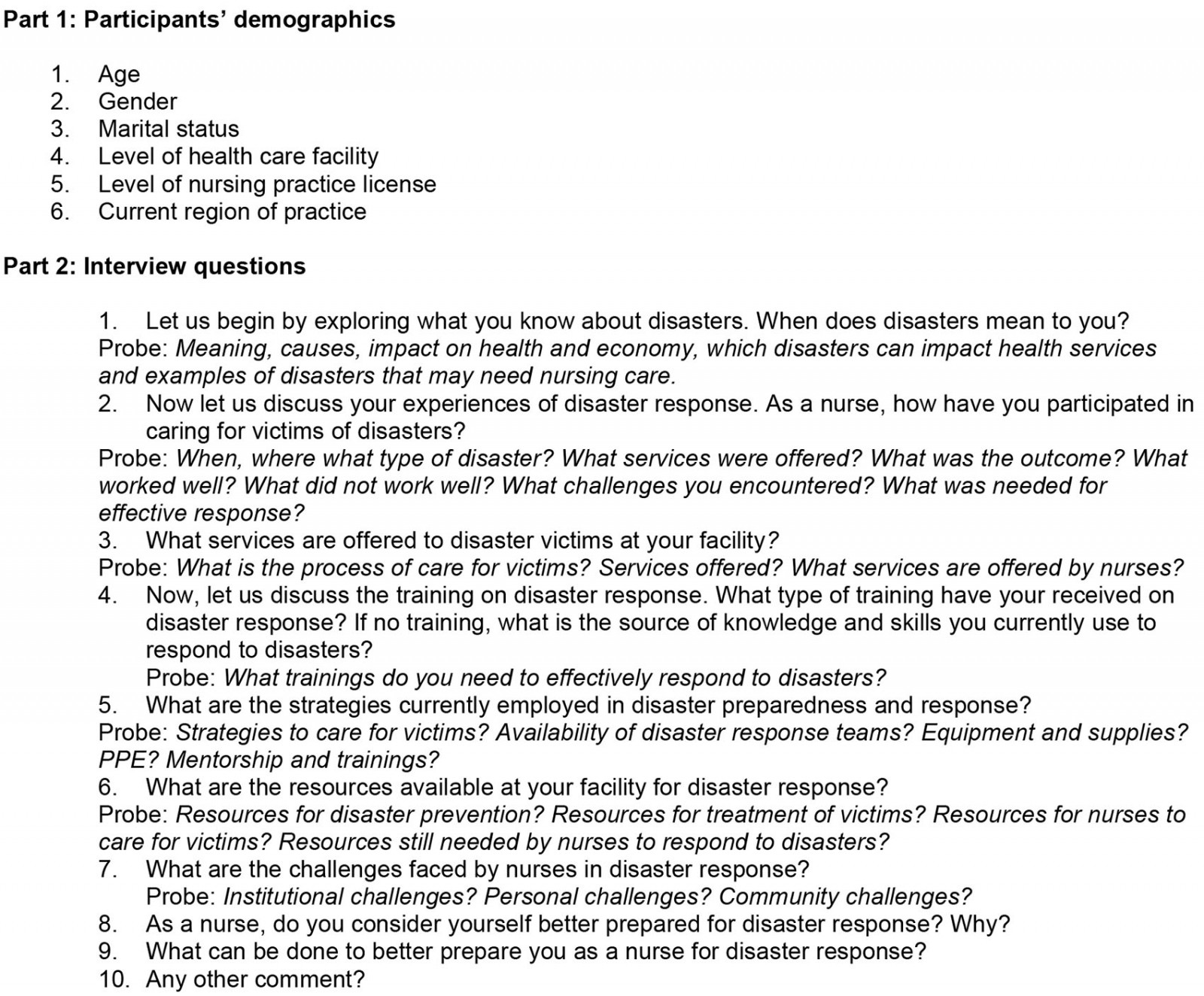
A semistructured interview guide was developed and translated through a consultative process involving experts from Aga Khan University. The English version of the interview guide was translated into the Swahili language, then back-translated into English and checked for conceptual equivalence. The interview guide covered previous experiences of disaster response, current practices for disaster prevention and management, and existing resources for disaster response and preparedness.
Three research assistants were recruited and trained on the use of the interview guide and techniques pertaining to this study. The interview guide was pretested in purposefully selected rural and urban settings. After pretesting, the guide was refined to ensure readiness for use in the actual data collection process. Close and supportive supervision of research assistants was implemented throughout the data collection and analysis stages to ensure data quality.
Telephone interviews
An initial call was made to each participant to schedule an interview based on their preferences. A second call was made on the day of the scheduled interview. Before starting the interview, participants were given information about the study, including the risks and benefits of participation (an information sheet was part of the interview material). Verbal consent for the interview and voice recording was obtained in advance. Prolonged engagement, which is critical for qualitative research rigor, was ensured during the interviews. Each interview lasted for 30–60 minutes and interviews were conducted at times preferred by participants. No monetary reimbursement was offered for participating in this study. However, after the interview, participants were sent a mobile phone voucher (equivalent to US$4.30 (A$6.40)) for their time.
Data analysis
The qualitative data analysis used the thematic analysis strategy described by Braun and Clarke12. A stepwise approach was used for a deductive thematic analysis of the interview transcripts. First, the research team examined the research questions and generated several themes based on consensus. This resulted in an analytical matrix of the main themes and subthemes using NVivo v12 (Lumivero, https://lumivero.com/products/nvivo). Individual transcripts and phrases (codes) representing participants’ responses to investigators’ probes were exported to relevant themes and related subthemes in the data analysis matrix. A consensus-based approach was used to decide whether to include codes, subthemes, and themes that did not fit within the matrix and discard those that were subjectively and objectively deemed of no critical value to this study. Upon reaching data saturation when no new information emerged from subsequent interviews6, the data in the matrix were exported to Microsoft Word for report generation.
Ethics approval
This study received ethics clearance from the National Institute for Medical Research (NIMR/HQ/R.8a/Vol. IX/3722) and local approvals from the regional medical offices. The authors ensured the responsible conduct of the research by obtaining verbal consent from all research participants before the telephone interview session.
Results
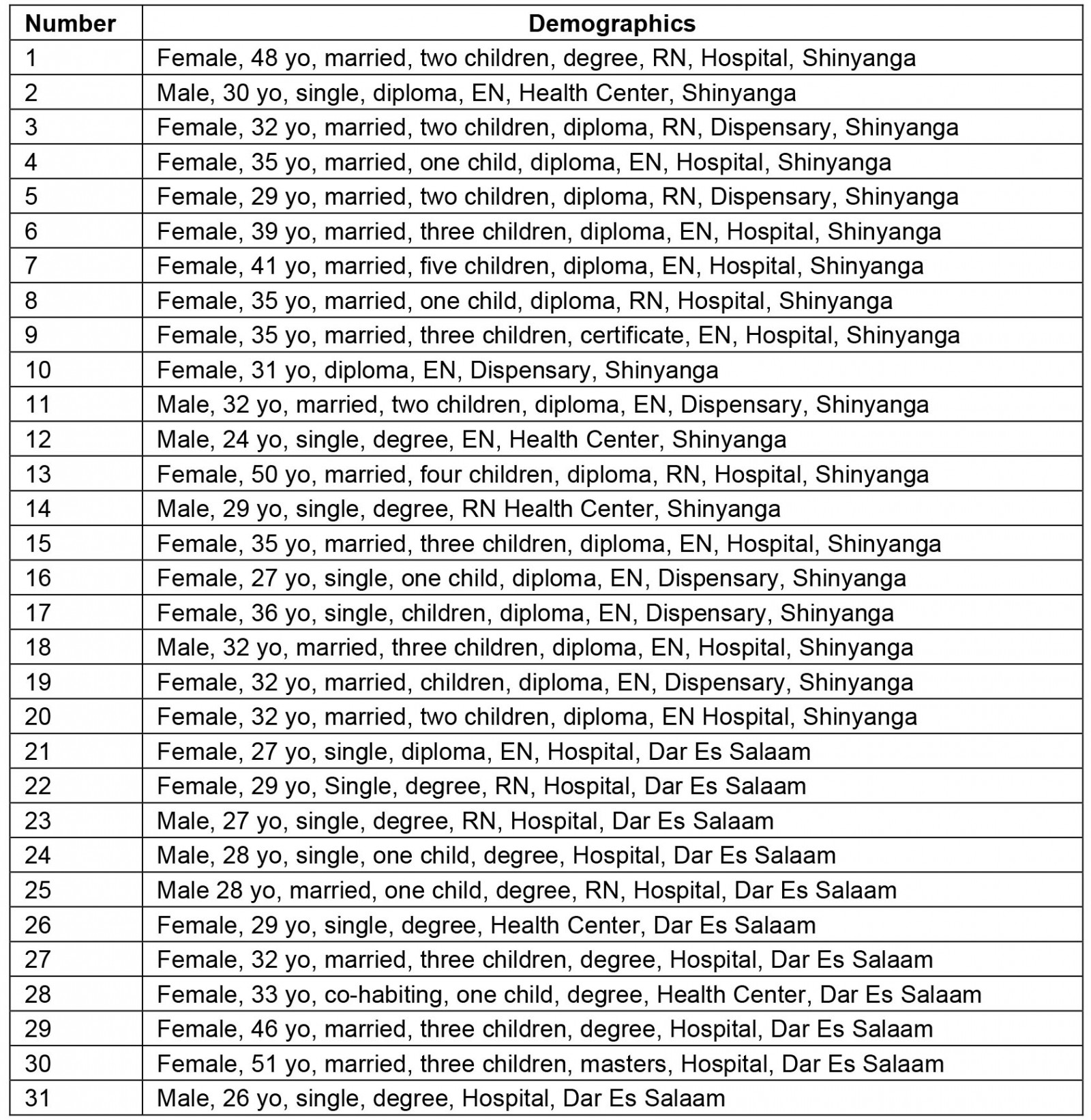
This study involved 31 nurses and administrators, of which the majority were from the rural region of Shinyanga (68%), were female (71%), had a diploma-level education (58%) and were aged 31–40 years (45%) (Table 1). Detailed demographic information for participants, and the interview guide used, are shown in Appendix I and Appendix II, respectively.
Table 1: Summary of participant demographics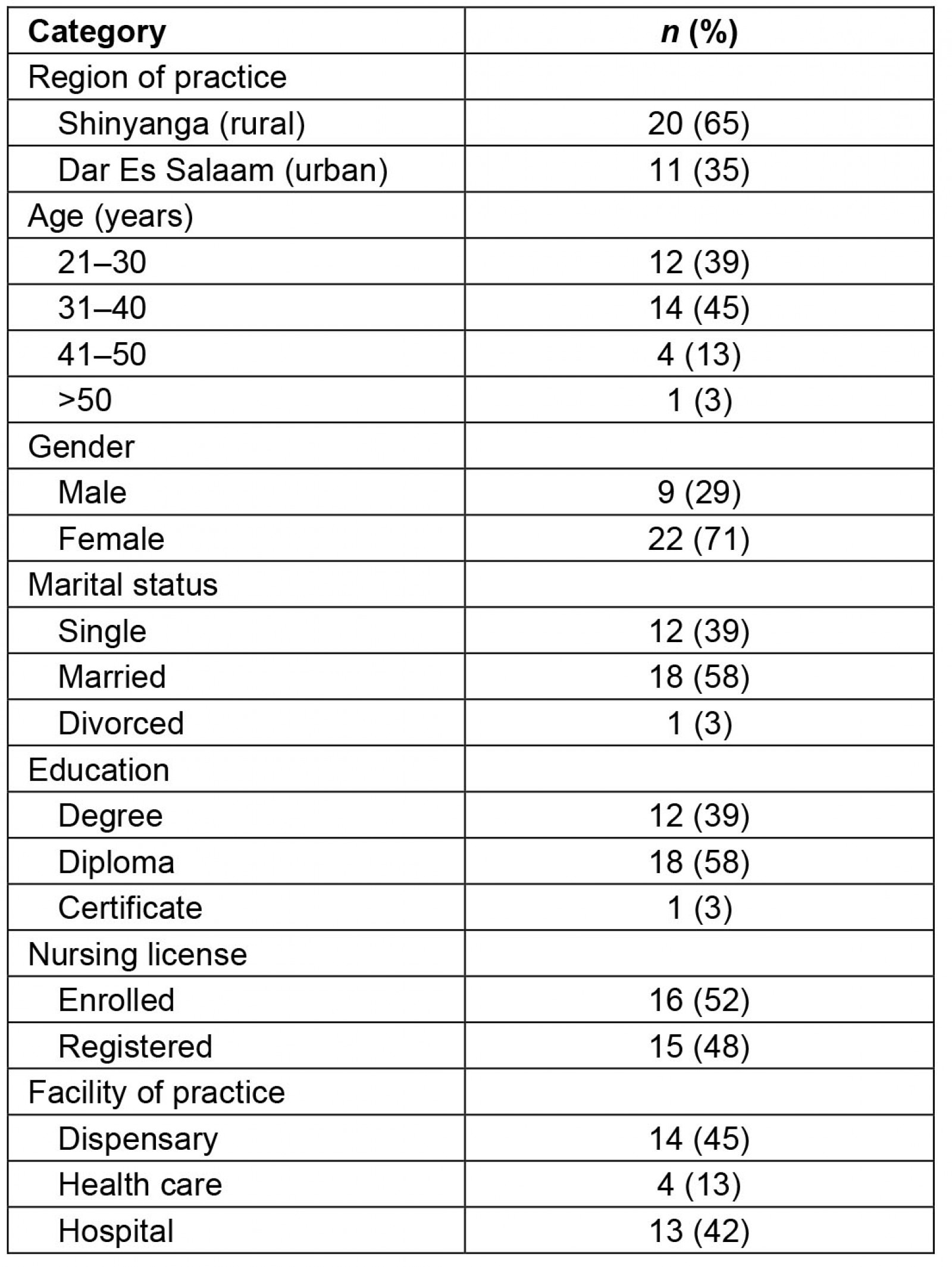
Theme 1: Previous experiences of disaster response and nursing services offered
There was a general consensus among nurses in both rural and urban contexts that they had previously been engaged in disaster management. These experiences included, first, personally offering nursing care to disaster victims of water-related accidents such as floods or heavy rain, victims of motor vehicle accidents, and people suffering from disease outbreaks. Nursing services offered at rural low-level health facilities included first aid and stabilization (wound cleaning and dressing, fluid replacement), monitoring and referral to higher-level facilities when advanced care was needed. The nursing services offered at rural and urban hospitals included emergency care, feeding support by insertion of nasogastric tubes, medications, fluid replacement, and general nursing care. Some participants described their experiences of caring for COVID-19 victims in isolation centers and offering oxygen therapy to those with advanced infection. A participant commented:
I remember offering care to victims of a car accident that affected many people. They were brought at our facility for first aid and most had injuries. We cleaned and dressed the wounds, and some were in shock, so we inserted IV lines and gave the fluids, and some were referred to a higher level because our facility is small. (Nurse, Dar Es Salaam)
Second, experience included being part of disaster response teams. These teams existed at the facility, district, and regional levels, but were currently perceived as ineffective, particularly in rural areas because of human resource and equipment limitations. The roles performed by nurses included visiting disaster areas and offering medical care to victims.
Third, experience included administrative roles during disasters. An example of this role was performing supervisory duties during the COVID-19 response, including ensuring the availability of frontline nurses and essential personal protective equipment (PPE).
Fourth and final, participants described experiences of conducting community sensitization on disaster prevention and management. Some rural nurses described experiences of offering health education at healthcare facilities and in the community on prevention (eg in the COVID-19 response). Some also described offering first aid services to victims in their communities of residence and then referring them to healthcare facilities. Some of these issues are discussed in the following comments from participants.
My experience is that there used to be disaster response teams from low levels at the dispensary, health centers, district, and region. Those teams were ready [to handle disasters] in terms of human resources, equipment, and infrastructure. But most recently, these teams have been ineffective because of the deficit or absence of staff. We also don’t have enough equipment to manage disease outbreaks, which needs a high level of protective gear. (Nurse, Shinyanga)
I have offered care to many victims. There was a flood in Ikonda village in 2014 and we participated by going there … We volunteered and went on foot and arrived but the working equipment was very poor and very few. The infrastructure was very poor, and cars could not reach there, and it was very difficult to evacuate victims, but we worked tirelessly and helped them. (Nurse administrator, Shinyanga)
As part of descriptions of their previous experiences, nurses cited a range of challenges encountered that were more pronounced in rural settings. Most rural participants cited unpreparedness of response teams, absence of experienced disaster experts, inadequate staff, disorganized care for victims in healthcare facilities, large numbers of victims, inadequate equipment for service delivery to victims, and unreliable victim transportation facilities. Inadequate equipment for disaster victim care, including PPE, emerged as a dominant concern among nurses in both rural and urban settings. Consequently, medical equipment including PPE, diagnostic equipment (X-rays and ultrasound), patient monitors, and life-support machines topped the list of resources that were needed for effective disaster response, which included establishing disaster response teams, hiring additional nurses, improving hospital infrastructure for emergency care for victims and transport infrastructure (including ambulances and roads), and having a dedicated disaster response budget. Other challenges were related to disaster assessment, such as delays in identifying, characterizing, and quantifying the impacts of a disastrous event. This was perceived as affecting the timeliness of the disaster response. One participant commented:
The first challenge I encountered is that services (in rural facilities) are disorganized and there are delays in organizing the response team because it is not well prepared. The second challenge is the limited availability of equipment, and you find that only a few pieces of equipment are available during disasters. The third challenge is the delays in the identification of disasters and determining their impact, which contributes to delayed care because nurses are unprepared, are few in number and equipment may be very few. (Nurse, Shinyanga)
Additional challenges cited were related to the victims themselves and community members, including lack of health insurance and low awareness of disasters, particularly in rural communities (reference made to COVID-19). Low awareness was also linked to language barriers in rural communities where victims and relatives were described as having poor comprehension of the national language (where tribal languages such as Sukuma are dominant). The final challenge was related to concerns about low knowledge and skills among some nurses. One participant commented:
The main challenge is understanding. There are some nurses [that] do things, but they do not have the relevant knowledge to ensure adequate care to victims. For example, victims of accidents always require emergency care, but nurses are not trained on how to handle victims of accidents and when they come, we don’t know where to begin. (Nurse, Dar Es Salaam)
Theme 2: Nurses’ technical capacity for disaster response
Almost two-thirds of nurses across all facility levels, mostly in rural areas, had not received training on disaster management, even in the context of the ongoing COVID-19 pandemic. Most described using past experience and knowledge received as part of nursing training in college or school. However, some nurses expressed concern that the knowledge from nursing school was outdated given recent disasters that needed new skillsets to respond. Some went on to mention the use of knowledge from internet sources when offering nursing care to clients. For example, one rural nurse from Shinyanga had learnt through the internet, including ‘YouTube’ and ‘watching movies on disasters’. Others described observing what their peers did, receiving support from peers who had been trained, or engaging doctors for more serious cases. For example, one participant commented:
I never received training. We just use our experience. We see what our fellow does, and we do what they do although we have not been trained on what to do if disasters occur. Regarding first aid, I know from nursing school that when a patient comes, I have to insert IV drip and if I see a more serious patient, I call a doctor. (Nurse, Shinyanga)
On the contrary, about one-third of participants had received training on disaster management. A common training program cited by rural participants focused on maternal and childcare in the context of COVID-19, which was delivered by Aga Khan University in Shinyanga. One participant had been trained in emergency care in Dodoma, another at the Comprehensive Community Based Rehabilitation in Tanzania, and another at Kahama College. These accounts suggested that there may be limited training on disaster management among nurses in the study settings apart from the COVID-19 response. One participant commented:
A doctor [principal investigator KI] from Aga Khan trained us on issues of provision of care to mothers and children during COVID-19. He trained us for 5 days where I think was at the beginning of the year or the end of last year. We learnt about what is COVID, when and where it started, prevention strategies and how to offer care to COVID-19 suspects and patients when they come to us and mothers and children. The training has been very useful to me personally and I continue to use what I learnt even today. (Nurse administrator, Shinyanga)
Furthermore, there was consensus among participants in both rural and urban contexts (those who had and had not received previous training) that they needed specific training on disaster management. A justification for the need for training was that nurses were at the frontline of disaster response in healthcare settings. Specific training topics requested included general disaster management skills, emergency care, critical care and trauma skills, international guidelines on disaster response, use of life-saving equipment, and management of context-specific disasters (eg fire accidents, motor traffic accidents, disease outbreaks, and floods in Shinyanga). It is important to note that the demand for more specialized training (eg in critical and trauma care) was more common among participants from Dar Es Salaam and hospital settings where intensive care units (ICUs) are commonly available. One nurse commented:
… personally, I need to be trained on critical care and trauma and how to operate within ICU settings and also if they can train me on emergency care because that is where victims of disasters are received [emergency department]. These are the training I need to start with. (Nurse, Dar Es Salaam)
Theme 3: Current disaster response strategies
Although some rural participants reported the absence of concrete plans for disaster management, others described how their facility had current disaster response strategies. The first such strategy was disaster response teams, which generated mixed responses. Some rural participants indicated the absence of an active disaster response team, with teams created reactively when disasters occurred. For example, a nurse from Shinyanga described the creation of an ‘emergency response team during the clinical meetings when a disaster occurs’. This suggested that rural facilities may be poorly prepared to respond to disasters and may explain why most nurses from dispensaries noted the absence of such teams.
The second strategy was essential equipment and supplies for disaster response, including an emergency kit. Some urban participants indicated they had PPE for disaster response, with equipment including gowns, aprons, boots, masks, gloves, resuscitation kits, and oxygen concentrators, but noted that supplies were often seriously inadequate. Ambulance services were available at the hospital-level only. Conversely, other participants, mostly in rural areas indicated the absence of essential equipment and supplies for disaster response. Some comments from urban participants indicated reliance on other entities during disasters such as Red Cross because they had ‘basic equipment for disaster response’ (Nurse, Dar Es Salaam).
The third strategy was dedicated infrastructure for the management of victims of disasters. Giving an example of COVID-19, a rural nurse from Shinyanga indicated the existence of room for the management of suspected cases.
The fourth strategy was capacity building through training. Although most rural participants indicated they had not received formal training, some had received training on disaster management through the COVID-19 training offered by Aga Khan University (frequently cited in Shinyanga). The issues with training have been explored in detail in previous sections.
The fifth and final strategy was community sensitization by nurses and community health workers (CHWs). Rural nurses reported they continued offering community education on prevention and early care seeking, and trained CHWs to refer clients to hospitals during household visits. Health education offered by nurses and CHWs appeared to be related to disease outbreaks that may present with clinical symptoms.
The strategies depend on the type of disaster but now we offer education on prevention … we educate them to rush to the hospital upon noticing symptoms so they to receive appropriate care. We also use CHWs by training them so that they can refer. (Nurse administrator, Shinyanga)
In addition to mentioning the five current strategies for disaster response, participants described factors that affect the effectiveness of these strategies. Factors that seriously affected disaster responses in both rural and urban contexts included concerns about the absence of resources or the availability of inadequate resources for disaster response. Only a few rural participants cited the existence of some resources for disaster response, such as equipment and medical supplies, but they were considered inadequate. One participant mentioned the availability of buckets of sand and water supply in reference to materials commonly used for fire disasters in the local context, in the availability of materials for non-fire related disasters. Likewise, most rural participants described human resources as inadequate. Despite these concerns, there was an acknowledgement of nurses and doctors who could adequately respond to disasters in urban healthcare facilities. Financial resources were another issue, with few rural participants reporting the existence of funds budgeted for medical equipment or reliance on funds from insurance schemes such as community health funds and national health insurance funds that could be used to purchase materials needed to care for victims of disasters. Descriptions of budgeted funds for medical equipment emerged in the account of one rural nurse working at a hospital-level facility in Shinyanga. However, the translation of the cited budget to ensure the availability of equipment for disaster response appears to be limited, as described in theme 4 below.
Theme 4: Current challenges in disaster response among nurses
The challenges in disaster response discussed by nurses could be divided into three groups. The first group were institutional challenges. These included inadequate resources (infrastructure, equipment, and medical supplies) as well as insufficient human and financial resources. These were the dominant challenges emerging in all participants’ narratives but were more pronounced in the accounts of rural participants. Other challenges were understaffing and a lack of experts at low-level facilities. Some rural participants indicated the absence of ‘educated nurses’ (with degrees) at low-level facilities and noted that nurses were tasked with multiple responsibilities, including meeting the demands of other development partners, which resulted in exhaustion and the inability to fully participate in disaster response efforts. The second group of challenges were individual challenges, including inadequate capacity (knowledge and skills) to respond to disasters. Some rural participants indicated that nurses lacked adequate knowledge and skills to offer care to victims of disasters. Another individual challenge was the fear of infection among nurses. Fear of infection during disease outbreaks was said to contribute to the absence of a ‘volunteering spirit’ among nurses. It is important to note that such fears may partly be linked to inadequate PPE. A critical individual challenge was poor interpersonal relationships among nurses, clients, and families, which was partly linked to inadequate education. The final group of challenges were rural community challenges. These included: (i) inadequate education among rural community members and language barriers (discussed previously); (ii) poor reporting systems for disasters; (iii) delayed healthcare seeking, and (iv) long distances to the facility and poor road infrastructure to reach disaster sites, indicating the need for infrastructure improvement in rural areas at high risk for disasters. Inadequate education was partly linked to delayed and underreporting of disasters, delayed healthcare seeking, and non-adherence to preventive measures when assisting or accompanying victims of disasters (disease outbreaks) to hospitals. One participant commented:
The rural community members do not know when and where to report disasters. For example, if there is a fire, most do not how to contact firefighters, even the hospital number to report an outbreak as it is done in Western countries may be a free call so that they can explain where the disaster is happening. We do not have a such system, which causes delays, consequently some come to the hospital in near-death conditions and some lose their life. There is no specific reporting system for disasters happening in communities. (Nurse, Shinyanga)
Theme 5: Overall preparedness for disaster response among nurses
Despite the institutional, personal, and community challenges faced by nurses in disaster response, there was a general consensus among participants that they were well prepared to respond when a disaster occurred. Some indicated readiness and willingness to respond partly because they had been trained in disaster response. Surprisingly, even those who had not received previous training on disasters and requested additional training said they were ready and well prepared. This suggested that the affirmation of readiness and preparedness was rooted in nurses’ willingness to care for those in need rather than being prepared with adequate knowledge, skills, and resources for disaster response. This was evident in the descriptions of many rural nurses who, after affirming their readiness, highlighted the need for additional training and acknowledged the existing challenges (cited above) as barriers to their preparedness. It is therefore logical to suggest that nurses in both rural and urban contexts may have a high willingness to fulfil their professional duties towards victims despite being inadequately prepared to respond to disasters.
Yes, I am prepared. If a disaster occurs, I am ready and willing to go but it is very important for nurses to receive appropriate training to improve their knowledge and skills, but since nurses are expected to be ready to offer care at any time, we are prepared to handle anything that may happen in our settings although not to the recommended international standard. (Nurse, Shinyanga)
I am well prepared but just that those challenges I mentioned above are the ones that pose difficulties. But in terms of preparedness as a nurse I am well prepared that if a disaster occurs, I can assist as I can but when the challenges (mentioned above) emerge then I fail [to understand] how to address them. (Nurse, Dar Es Salaam)
Participants made several suggestions regarding how to better prepare nurses for disaster response. A recurrent suggestion was technical capacity building in terms of training. Training (seminars and refresher courses) was considered necessary to build nurses’ knowledge base and skillsets in managing disasters as well as community sensitization efforts. Cognizant of the wide acceptance of the distance learning model, some participants suggested establishing online modules on disaster response. Another common suggestion was ensuring the availability of essential equipment and medical supplies for disaster response, including PPE, diagnostic and life-support machines, and medications. Participants also suggested increasing the number of nurses, particularly in rural areas, to address inadequacies noted during disasters and improving the disaster reporting system to facilitate timely response and dissemination of existing local guidelines on disaster response. Although this study did not examine the existence of local guidelines, some rural nurses suggested the need to be given local guidelines on prevention and response to disasters. Another suggestion was establishing, strengthening, and adequate engagement in disaster response teams. Financial incentives for nurses willing to take part in disaster response efforts were also suggested, with one nurse recommending risk/extra duty allowances for effective disaster response. Other nurses suggested psychosocial support through encouragement and support by leaders. Finally, participants suggested improvement of the nursing training curriculum to include topics on disaster management. This was because there were concerns that no specific content on disaster management was included in nursing curricula. Curriculum improvement was advocated by a rural nurse from Shinyanga, although some participants affirmed that they were currently using knowledge and skills gained during nursing school when responding to disasters (see above). This indicated there was a need to improve the nursing curricula in view of the changing global landscape of disasters.
We need more training. If not face to face at least there must be content online or online classes or modules that we can study since online learning has now been simplified. We can be trained online without necessarily meeting physically in a classroom. We can also be trained through the social media that we use every day. (Nurse, Shinyanga)
We need sufficient medical equipment and supplies. They also need to improve reporting systems for us to be able to act quickly but also the inadequacy of nurses needs to be addressed by hiring more so that we have enough nurses and avoid taking people from wards when there is a disaster creating deficits in the wards. (Nurse, Dar Es Salaam)
Discussion
This study explored preparedness for disaster response among nurses in rural and urban PHC settings in Tanzania. The findings included rich descriptions from rural and urban nurses and nurse administrators who were responsible for decision-making during disaster responses; this contributed to data triangulation, which is a critical criterion for ensuring the trustworthiness of qualitative research11. Nurses from a rural regional hospital in Shinyanga were included because the few existing studies on the disaster in Tanzania indicated inadequate preparedness at this level despite the experiences of caring for victims of large motor vehicle accidents, floods, and infectious disease outbreaks10. These findings, therefore, provide a building block for interventions to better prepare nurses in both rural and urban settings for disaster response.
Limited research is available on disaster response in rural and urban PHC settings. However, these findings indicate that almost all nurses in the study settings had experienced at least one form of disaster in their nursing practice. Nurses’ previous experiences were characterized by activities such as personally offering nursing care to disaster victims where improvement in victims’ health or death were common outcomes; being part of disaster response teams at the facility, district, and regional levels; performing administrative roles during disasters; and experiences of conducting community sensitization on disaster prevention and management. These findings were similar to nurses’ roles in disaster response reported in previous studies. Previous research in Western countries highlighted the role of nurses in disaster management as extend beyond implementing disaster plans, conducting triage for victims, providing emergency care for victims, and transporting of victims13-20. In Western countries, however, PHC nurses are involved in the direct treatment of victims7, a role that did not emerge in the current data. Nevertheless, nurses in rural and urban Tanzania play a significant role in disaster response in health care.
The study identifies factors limiting the successful engagement of nurses in disaster response, particularly in rural areas, as including unprepared response teams; absence of experienced disaster experts; inadequate staff; disorganized care for victims in healthcare facilities; large numbers of victims; inadequate equipment for service delivery to victims and unreliable victim transportation facilities; delay in identifying, characterizing, and quantifying impacts of a disastrous event; victims without health insurance; low awareness of disasters; and low knowledge and skills among some nurses. Institutional challenges (eg inadequate resources, understaffing, lack of expertise at PHC facilities, and tasking nurses with multiple responsibilities), personal challenges (eg inadequate technical capacity, fears of infection, poor interpersonal relationships), and community challenges (eg inadequate knowledge, poor reporting systems, delayed healthcare seeking, and long distances to facilities and poor road infrastructure) further strained nurses’ contribution in disaster response. It is important to note that most of these issues were identified in the previous literature as barriers to effective engagement of nurses in disaster response initiatives and barriers affecting disaster management in healthcare systems as a whole regardless of the settings21-24. Lack of health insurance is of particular importance because insurance coverage is still low in the country25,26. Although an emphasis has been placed on the community health fund, which is a reliable low-cost health insurance scheme for the poor and low-income population (about US$12.7 (A$19) per year for a family of six), it has been considered as a failure with poor enrollment, poor performance, and benefit packages that may not be sufficient to meet the cost of advanced care during disasters25,26. This suggests that maximizing the role of nurses in disaster response requires strategies that seek to address the multiple barriers faced in nursing practice and the whole healthcare system in both rural and urban contexts.
Lack of or inadequate training on disaster management mostly among rural nurses was a key factor that limited their full engagement in disaster response initiatives. Existing literature from Western countries identified inadequate training among nurses as an important barrier to the efficient and effective response to disasters6,22,24,27,28. For example, a qualitative study conducted in the USA28 explored willingness to respond to disasters among pediatric nurses and indicated that lack of training in disaster response was a key driver of unwillingness. The current findings show that almost two-thirds of rural nurses had not received training in disaster management. Most nurses in this study settings relied on previous experience, knowledge from nursing schools (despite concerns of such knowledge being outdated), observing peers, and knowledge from internet sources and movies for disaster response. Internet sources such as YouTube and disaster movies were common sources of disaster response skills for some participants. The Aga Khan University was recognized for running a short course on maternal and childcare in the context of COVID-19 in a rural region of Shinyanga, which was the only formal training on disaster management cited. These findings indicated a need for continued formal capacity building among nurses on disaster response, prioritizing rural settings to increase their engagement in future disasters.
Although a number of strategies were cited as currently being implemented as part of disaster response, concerns about the weaknesses of these strategies particularly in rural settings emerged. For example, disaster response teams were described, but most rural participants considered these teams as either weak or formed on an ad hoc basis during disasters, possibly contributing to delays in response. Lack of existing disaster response plans in PHC was cited as partly contributing to the weakness of disaster response teams. Similarly, as adequate financial, human, and material resources were needed for disaster response19-30, the participants noted the need to ensure the availability of equipment and supplies for disaster response. However, concerns of the inadequacy of such resources dominated most in rural settings. Participants discussed the availability of dedicated infrastructure for the management of victims of disasters and community sensitization by nurses and CHWs. Despite the existence of buildings in some rural PHC settings and healthcare workers and CHWs providing opportunities for disaster responses, other institutional and community challenges (cited above) continued to limit the effective use of these tools in PHC settings.
A general consensus among participants was that nurses were well prepared to respond when a disaster occurred despite facing institutional, personal, and community challenges. Surprisingly, even those who had not received previous training on disasters, work in rural facilities and requested additional training, noted they were ready and well prepared for disasters. This suggested this readiness was rooted in nurses’ willingness to provide care rather than preparedness with adequate knowledge, skills, and resources for disaster response. The nursing profession seeks to ensure that nurses are readily available and willing to offer care to patients in need during both normal healthcare service delivery and disasters7-9,13-24,31. This may explain why the suggested strategies to better prepare nurses for disaster response included training, ensuring the availability of essential equipment and medical supplies, increasing the number of nurses, improving disaster reporting systems, disseminating existing local guidelines on disaster response, establishing/strengthening and adequate engagement in disaster response teams, financial incentives for nurses, and improvement of nursing training curricula to include topics on disaster management. Much emphasis, however, must be placed on rural PHC settings, which appear disadvantaged in many aspects of disaster preparedness.
Limitations
This study had two main limitations. First, the study largely relied on nurses and nurse administrators’ understanding their preparedness for disaster response. While the accounts of these healthcare workers provided insight into their experiences and perspectives, the insights of other healthcare providers (eg doctors, physiotherapists) who are often engaged in disaster response were not explored. Second, while the findings shed light on disaster preparedness among nurses in rural and urban PHC, participants’ accounts may mostly reflect the COVID-19 pandemic response. However, since other disasters such as water-related and motor traffic accidents were described, the findings are relevant and may be applicable to all disasters of public health interest.
Conclusion
Nurses form the largest group of healthcare providers and continue to play a critical and significant role in the provision of healthcare services to patients and families. The findings indicate that nurses in rural and urban settings of Tanzania are continually involved in disaster response by offering nursing care to victims, being part of disaster response teams, performing administrative roles during disasters, and conducting community sensitization on disaster prevention and management. However, a range of institutional, individual, and community issues affect nurses’ preparedness for disaster response in PHC settings. These challenges, however, appear to be more pronounced in rural PHC settings than in urban counterparts. Addressing these challenges requires multiple strategies extending beyond the capacity building of nurses to strengthen the health system disaster preparedness in general, prioritizing rural contexts.
Funding
This work was supported by the Dean’s Fund at the School of Nursing and Midwifery, Aga Khan University.
Conflicts of interest
The authors declare that this research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest.
Acknowledgements
The authors acknowledge the financial and technical support from Dr Eunice Ndirangu-Mugo, the Dean of School of Nursing and Midwifery at Aga Khan University; the technical guidance of Dr Eunice Siaity, Associate Dean of School of Nursing and Midwifery in Tanzania; and the tireless efforts of research assistants Ms Zabibu Mruttu, Ms Joyce Kaswamila, and Mr Elibariki Petro. The authors thanks Ms Audrey Holmes of Edanz Editing (www.edanzediting.com) for editorial assistance.