Introduction
Health professionals’ maldistribution and retention in underserved areas are global problems in developed and developing countries, including Indonesia. The Indonesian government has implemented strategies to increase health workforce recruitment and retention in underserved areas, such as rural compulsory work for new graduates through the internship and PTT (pegawai tidak tetap; 'temporary employment') program1, Nusantara Sehat program, and incentives2-4. However, retention is still low5.
Retention factors vary according to geographical location, age, sex, family status, practice duration, and professional duties6. There are many factors related to retention: personal, financial, working and living conditions, mandatory service, career and education, family, community7, professional considerations6, and employer management style8. Among those factors, rural GPs in Australia ranked on-call arrangements, professional support, and a variety of rural practices as the top three factors6.
Nurses are at the frontline of the health workforce and a critical component of health service facilities. Based on Indonesian regulations, the target is 180 nurses for the 100 000 population9. In 2020, the ratio in Nusa Tenggara Timur (NTT) province was 12 414 nurses per 5 325 000 population or 1:42810 – below the national target11.
The lower the nurse-to-population ratio, the more work nurses must do. High workloads may lead to nurses’ stress and burnout12, disrupting their work–life balance and mental wellbeing13, and even causing depression. Health professionals may leave rural areas because of the high workload and poor work–life balance13. Physical, mental, and spiritual health also influence rural health workforce retention14.
Depression is a global problem, with 5% of adults suffering from depression15. Depression is a leading cause of disability in terms of total years lost due to disability16. Depression may also lead to suicide. There are more than 700 000 suicide deaths every year globally15,16. It is estimated that, for each suicide death, about 20 people have attempted suicide16. In Indonesia, about 6.1% of adults experience depression, which is higher than the global prevalence. NTT province has the third-highest rate in Indonesia (9.7%), below Sulawesi Tengah (12.3%) and Gorontalo (10.3%) provinces17.
Depression prevalence in the general population has increased since the COVID-19 pandemic. A study concluded that depression prevalence in US adults increases three-fold during pandemics18. A similar phenomenon is also seen in health workers. A meta-analytic study involving 33 062 participants reported that 22.8% of health workers experienced depression worldwide during the COVID pandemic19. An umbrella review of seven meta-analyses conducted in four countries concluded that 24.83% of health workers experienced depression during the pandemic20. A systematic review of 59 studies reported that healthcare workers’ prevalence of depression during the pandemic ranged from 5% to 51%, with a median of 21%21. A study in Wuhan involving 2014 nurses from two large hospitals concluded that 60.5% of participants experienced emotional fatigue and 10.7% experienced depression in the pandemic22. A national online cross-sectional study in China involving 1103 emergency nurses stated that 43.61% of participants were depressed during the pandemic23.
Health workers, including nurses, have a higher risk for depression than the general population. Caring professions such as nursing involve emotional attachment to patients. So, nurses are more vulnerable to burnout, grief, and feelings of guilt20. This risk has been even higher during the COVID pandemic, in which they are the frontline workers exposed to hazards21, such as pathogens22,23, psychological distress22,24,25, long working hours, occupational burnout, high workload22, stigma, and physical and mental violence21. A decrease in family income also plays a role in depression18.
During the COVID pandemic, many schools have been closed, and children are at home, causing more significant burdens and work–family conflict, especially for female healthcare workers. This conflict has increased the risk of depression26. Working in rural areas with limited resources and support for healthcare workers (such as lack of public facilities, health equipment, medicine, and transportation) may complicate the problem further. It is logical to assume that these rural limitations may burden the nurses further, increase their depression level, and reduce their retention in rural areas.
Resilience is a person’s capacity to survive amid challenges, adversities, and stress27. A systematic review suggested that increasing resilience may reduce nurses’ emotional distress and other adverse effects, and improve nurses’ work performance12. Other studies found that resilience was negatively correlated with depression22,28. In other words, higher resilience has a protective effect from depression.
Understanding resilience is a crucial resource to increase nurses’ capacity to explore their potential and improve their capacity to handle challenges12. Resilience also enhances their engagement in the workplace, their job satisfaction, and their retention12. A study of rural doctors in NTT province, Indonesia, found that the longer doctors work in rural areas, the higher their resilience29. To the best of our knowledge, the literature says little about the effect of resilience on nurses’ rural retention.
This study aims to understand the effect of resilience and depression on nurses’ retention in rural areas. Our hypotheses were that resilience would affect retention, resilience would increase with seniority, and nurses identifying as depressed would have lower retention and lower resilience scores.
Methods
Study design
This study was an online, cross-sectional survey30. The variables involved were depression level (no depression, mild, moderate, severe), scores for the six dimensions of resilience (determination, endurance, adaptability, recuperability, comfort zone, life calling), and nurses' retention in a rural area (practice duration).
Setting
This study was conducted in July – August 2021 in NTT province, Indonesia. Most of this province’s areas (18 of 22 regencies) are rural31. Most of the working population (age >15 years) work in agriculture, forestry, and fishing industries, with 51% of them having elementary school education or less32.
In NTT province, 16 558 registered nurses serve a population of 5.3 million32. According to Indonesian Nurse Association (PPNI NTT) data, almost half of them (46.2%) work in underserved areas.
This study was conducted during the COVID pandemic, with 59 185 positively confirmed patients (around 1% of the population) and 1175 deaths (2% case fatality rate) in the province on 30 August 202133.
Participants
Participants were registered nurses living and working in rural NTT province, Indonesia. Participants were excluded from the study if they could not be contacted, refused to participate in the survey, or had been approached three times without any response. A consecutive sampling approach was applied with a minimum sampling size of 240 participants (calculated using the Lemeshow formula)32.
Instrument
The resilience score was obtained using an adapted Adult Personal Resilience Scale and presented as a profile of scores calculated separately for each resilience dimension34. This scale was validated for use among NTT province rural doctors, and the Cronbach’s alpha scores were 0.809–0.960 for each dimension34. There were six resilience dimensions with five items on each dimension, ranging from 1 (‘highly disagree’) to 5 (‘highly agree’). The subtotal score for each dimension had a range of 5–25, and its mean score range was 1–5. We used the mean score of each dimension in the analysis process. No final composite resilience score was calculated because each dimension measured different facets of resilience and may give more meaningful information29,34.
Depression level was measured using the Beck Depression Inventory-II (BDI-II) Scale35. There were 21 items with a four-point Likert scale ranging from 0–3. The final score was calculated as the total score of 21 items (range 0–63). The higher the score, the more depressed the participant. The total score was then classified as no depression (0–9), mild (10–18), moderate (19–29), or severe (30–63). The validity and reliability of this scale were measured in Indonesia with a Cronbach’s alpha score of 0.9036.
Retention in rural areas was measured using practice duration in the province, in years. The participants were categorised as junior (<5 years experience), mid-career (5–10 years), and senior (>10 years)29. WHO defines rural health workforce retention as health workers remaining employed in rural areas for specific periods7. WHO suggested some indicators to measure retention: turnover and vacancy rates, duration of stay and service, survival rates, the proportion of health workers staying in rural areas (stability index), and density of health workers in rural areas compared to urban areas7. This study measured retention by practice duration to compare with a similar study on GPs29 and to fulfill the future goal of intervening in graduates’ retention through health professions education. Thus, the length of time the graduates serve in rural areas is a valuable measure of the project outcome.
Procedure
Data were collected through an online survey using Google Forms. The detailed process is illustrated in Figure 1.
Potential participants’ data were collected from the PPNI NTT and using the snowball method. A survey link was sent by SK, one of the committee members in the PPNI NTT, to all regencies’ WhatsApp groups for nurses in the province. All investigators sent the survey link to their related personal contacts. WhatsApp was chosen instead of email because it is more widely used by Indonesian people. It was explained in the informed consent that 50 randomly selected participants would be rewarded 25.00 rupiah (A$0.003) in the form of a mobile phone load. One survey item (optional) asked participants for a mobile phone number, and the rest of the e-survey was anonymous.
The participants gave informed consent after reading the study information provided on the first page of the e-survey by clicking on the ‘consent to participate’ button. SK sent reminders every week for three consecutive weeks through the WhatsApp groups. The e-survey data were automatically stored in the first researcher’s (NH) Google Drive. Only NH, SK, and a research assistant had direct access to the e-survey form on Google Drive.
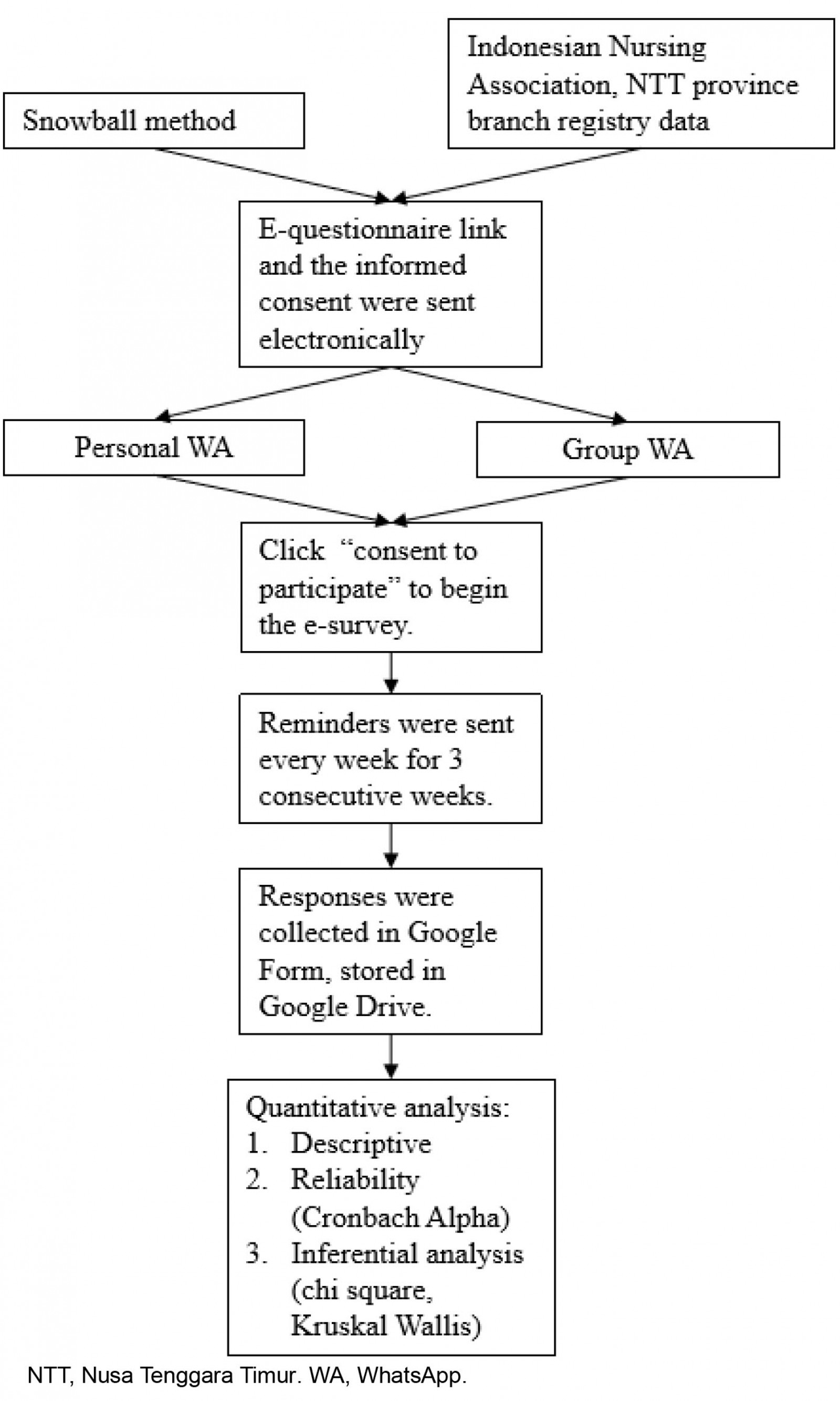 Figure 1: Flow chart of data collection procedure.
Figure 1: Flow chart of data collection procedure.
Data analysis
Missing data were excluded listwise. Data were then analyzed quantitatively using the Statistical Package for the Social Sciences v20 (http://www.ibm.com/SPSS/Statistic) through several steps as follows.
For the descriptive analysis of participant characteristics, frequency and percentage were calculated for nominal variables. Mean, minimum, maximum, and standard deviation were calculated for numeric variables.
Reliability for each resilience dimension was calculated using Cronbach’s alpha.
In the inferential analysis, the variables were depression level (ordinal), resilience dimension scores (numeric), retention in the province (numeric), and retention in the most recent regency (numeric). The distributions of the numeric variables were checked using the Kolmogorov–Smirnov test, and all showed non-normal distribution. Thus, the relationships between variables were measured using a non-parametric test (Kruskal–Wallis) and Spearman’s rank correlations37. When a Kruskal–Wallis analysis showed a significant result, we conducted a further pairwise comparison analysis to see which groups differed.
We repeated the analysis in which the retention variables were classified ordinally as junior (<5 years experience), mid-career (5–10 years experience), and senior groups (>10 years experience). This grouping referred to a previous study29. The statistical analysis performed was also adjusted to Kruskal–Wallis and χ2 tests.
Some steps were conducted to reduce potential biases. Before collecting data, two questionnaire evaluation meetings with the PPNI NTT representatives were conducted. This meeting was conducted to improve the questionnaire readability, suitability, and acceptability for nurses. A nurse representative of the organization (SK) was invited to join the study team to ensure the correctness and fairness of the data interpretation. PPNI NTT representatives of all regencies were involved in the data collection to increase participation and ensure all regencies were represented in the study.
Ethics approval
Ethical approval was granted by Nusa Cendana Medical School Research Ethical Committee (51/UN15.16/KEPK/2021).
Results
Demographics
A total of 1050 participants joined the study, and 902 participants’ data were analyzed after cleaning (Fig2). The response rate is difficult to determine because the questionnaire was delivered online through the WhatsApp group.
Outliers in the variable retention were removed using the filter ‘< 21 years’. Characteristics of the 902 participants are presented in Table 1.
Most participants were female (54.4%), with a mean age of 32.7 years, and only a small proportion were married (22.5%). More than half (54.4%) were born rurally and raised in the studied province (94.2%). The majority of the participants identified as ‘Catholic’ or ‘Christian’. Their mean work duration in the province and the current regencies were 8.6 years and 7.1 years, respectively. The mean work duration difference showed that some participants were moving across regencies. The proportion of participants working in non-underserved regencies was almost 1.5 times that of those working in the underserved regencies: 58.9% and 41%, respectively. Participants were representatives of all 22 regencies, with 13 underserved regencies. However, there were no differences in work duration, depression, and resilience scores between the underserved and non-underserved groups.
Table 1: Study participant characteristics (n=902)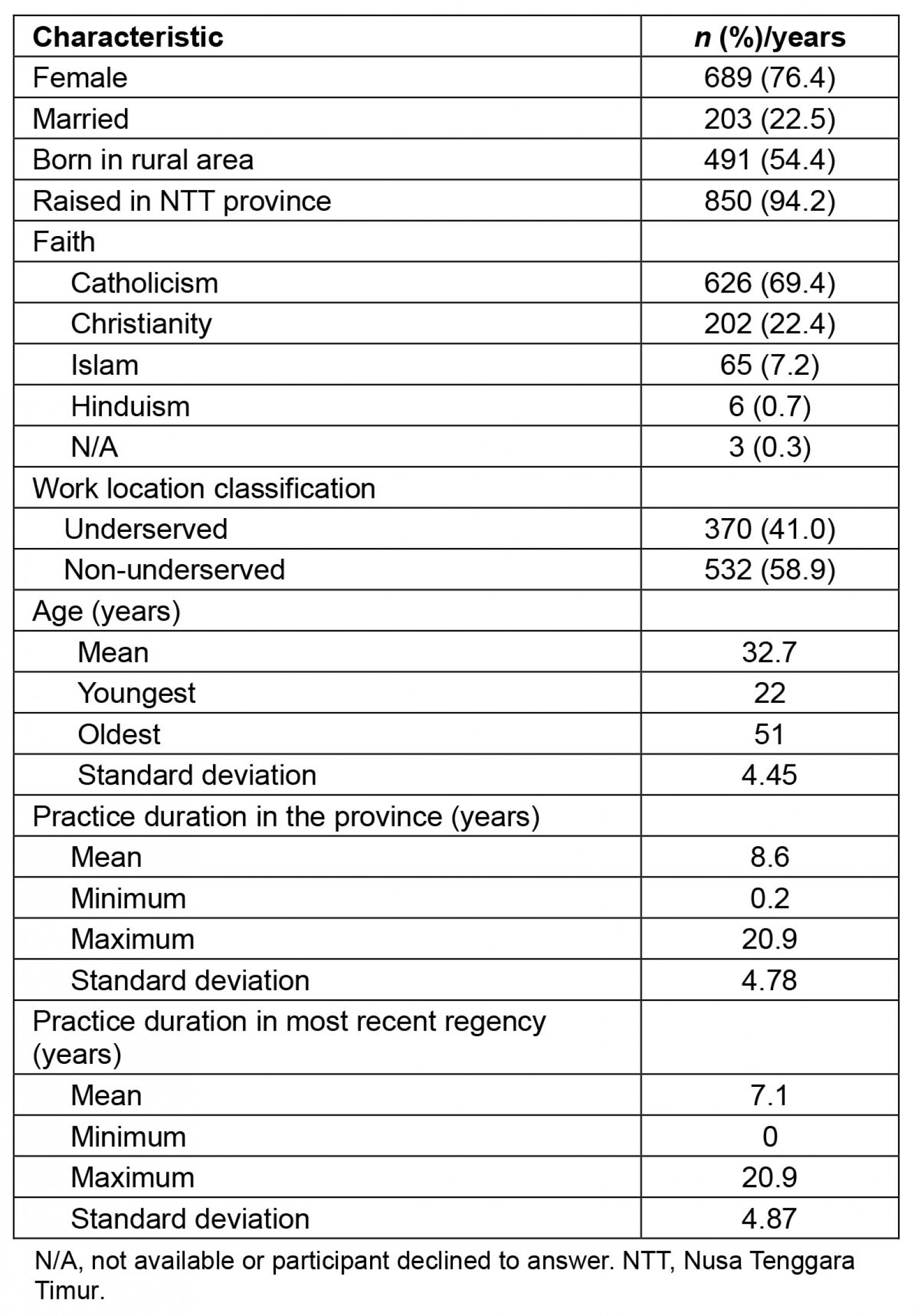
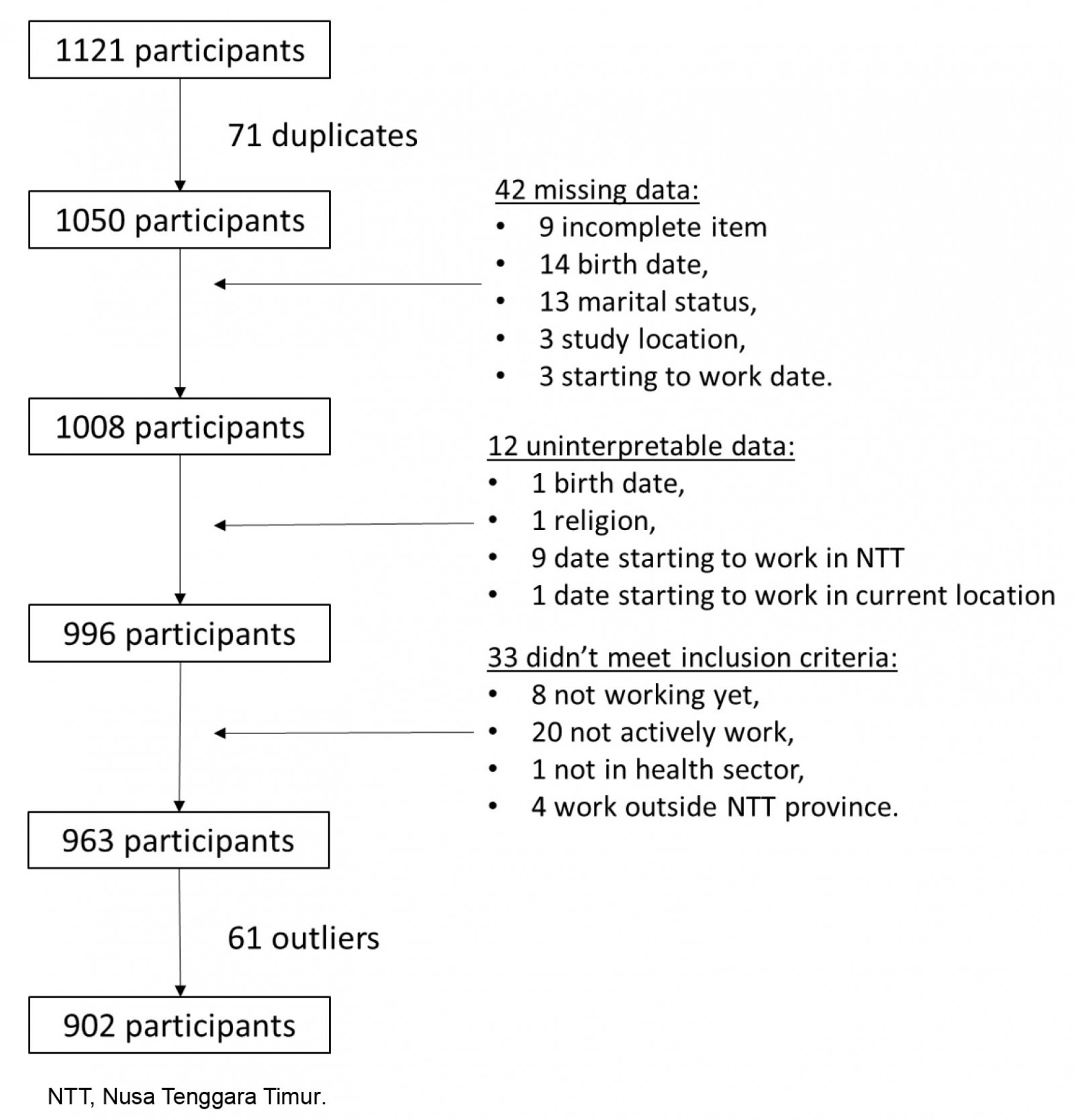 Figure 2: Flow chart of study participant selection.
Figure 2: Flow chart of study participant selection.
Resilience and retention levels
Spearman’s rank correlations measured the strength of the associations between resilience and retention (Table 2). All dimensions showed a minus coefficient, except the comfort zone. The minus coefficient meant that the higher the resilience scores, the lower the retention.
The participants were then divided into three groups based on their work duration: junior (<5 years), mid-career (5–10 years), and senior (>10 years) to enable comparisons with a preceding study and explore which group to focus intervention on for our subsequent investigation. The six-dimension resilience profile is presented in Figure 3 and Table 3.
We used the Kruskal–Wallis test instead of ANOVA because the data were not normally distributed. The results showed that three dimensions were significantly different between groups: determination (p=0.001), recuperability (0.000), and life calling (p=0.018). Further pairwise comparisons were performed to see which groups differed from each other (Table 4). The senior groups differed significantly from the younger groups (junior and mid-career). This difference also applied to the adjusted significance, except between junior and senior groups in the life-calling dimension.
Table 2: Spearman’s rank correlations between resilience and retention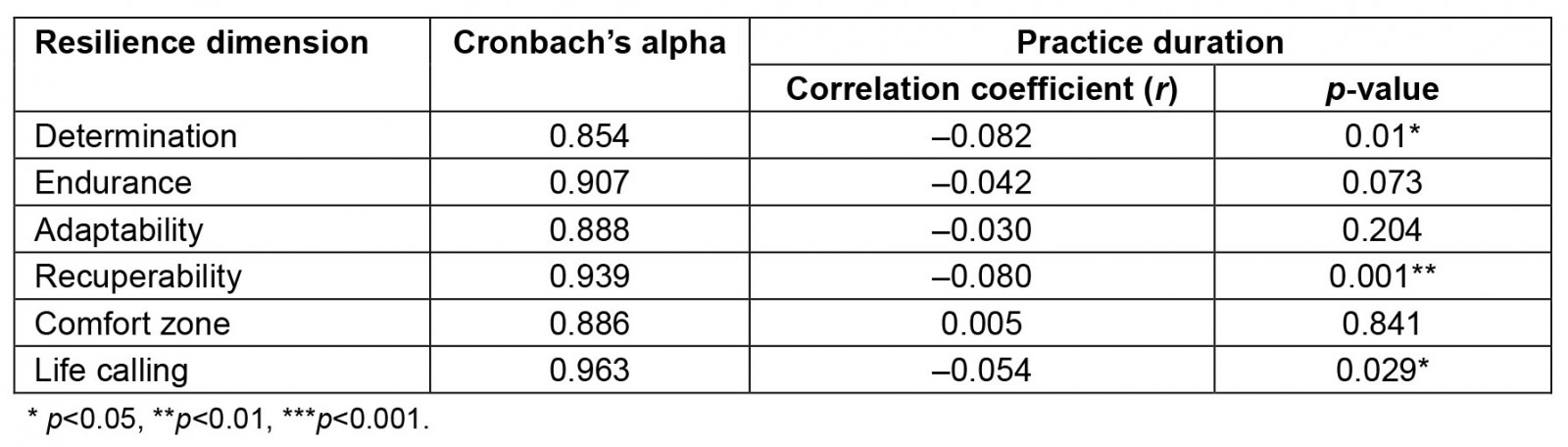
Table 3: Six resilience dimensions profile by practice duration in province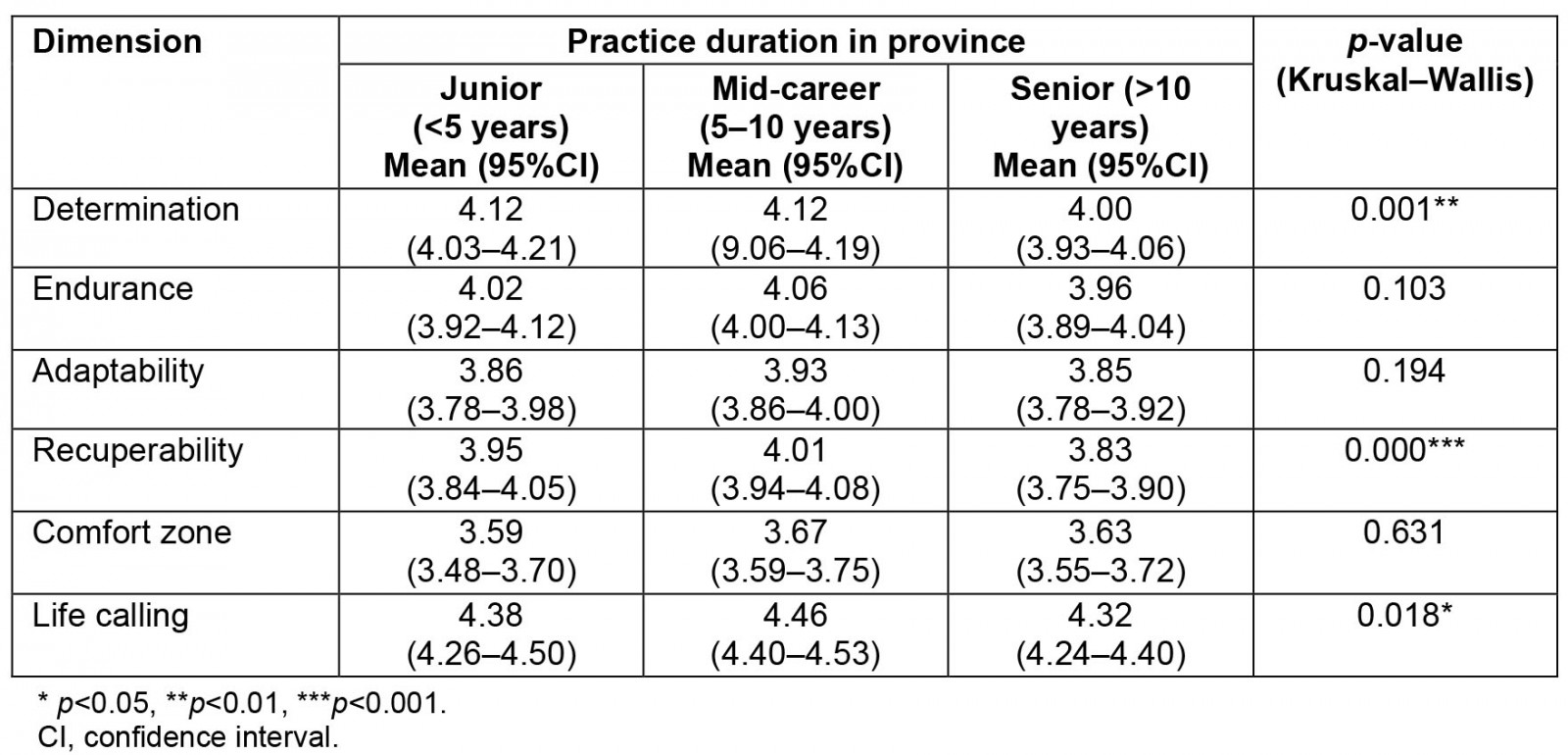
Table 4: Pairwise comparisons following Kruskal–Wallis test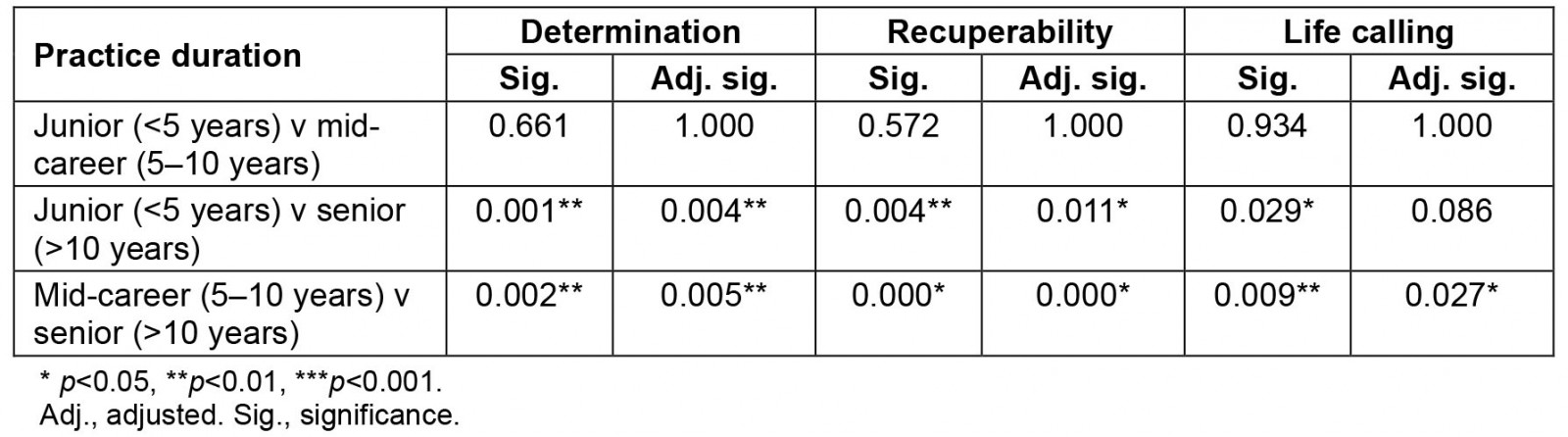
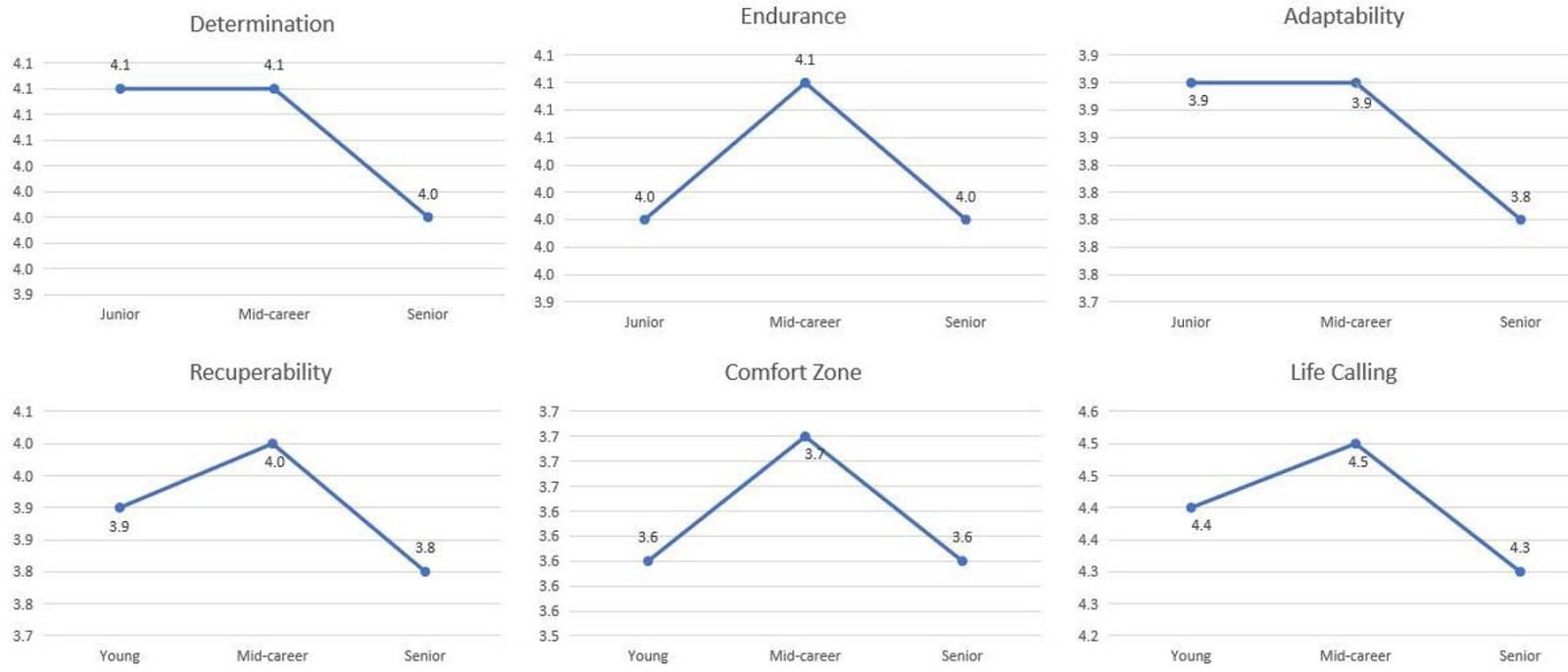 Figure 3: Six resilience dimensions profile.
Figure 3: Six resilience dimensions profile.
Depression and retention levels
The Kruskal–Wallis test results between depression groups showed a significant difference in retention for the most recent regency only (p=0.032). However, they did not show an effect on the overall work duration in the province (p=0.164) (Table 5). Further pairwise comparisons showed that only the mild and moderate depression groups differed in their practice duration in the most recent regency (Table 6).
The χ2 for k sample showed a significant difference between groups (p=0.007, degrees of freedom=4). The participants reported experiencing mild (11.5%) and moderate (5.1%) depression (Table 7). Fortunately, no participants had experienced severe depression.
Table 5: Practice duration by depression level 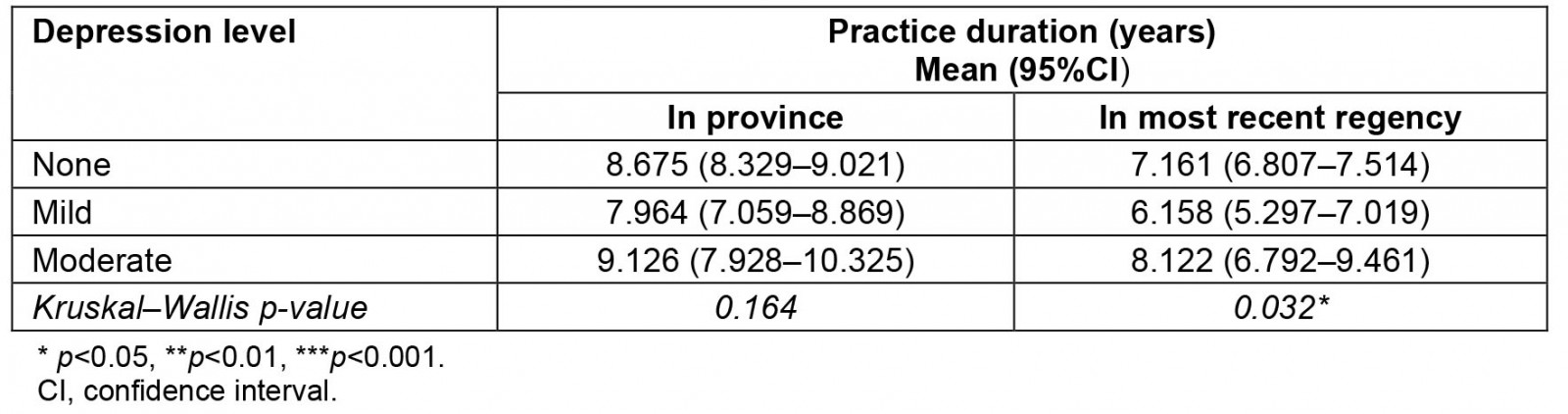
Table 6: Pairwise comparison, by depression level, of practice duration in most recent regency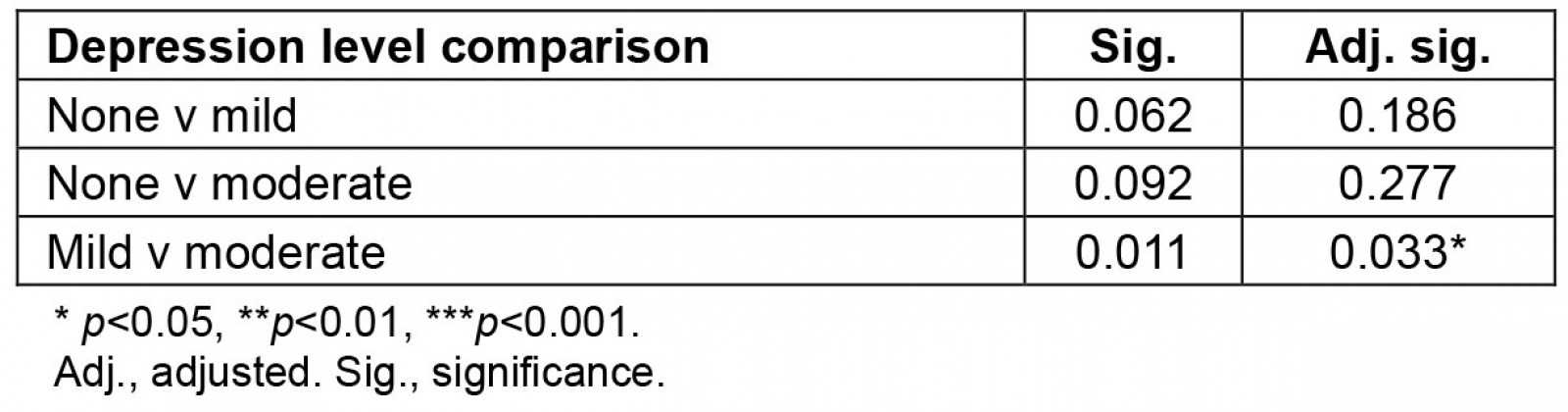
Table 7: Practice duration in most recent regency by depression level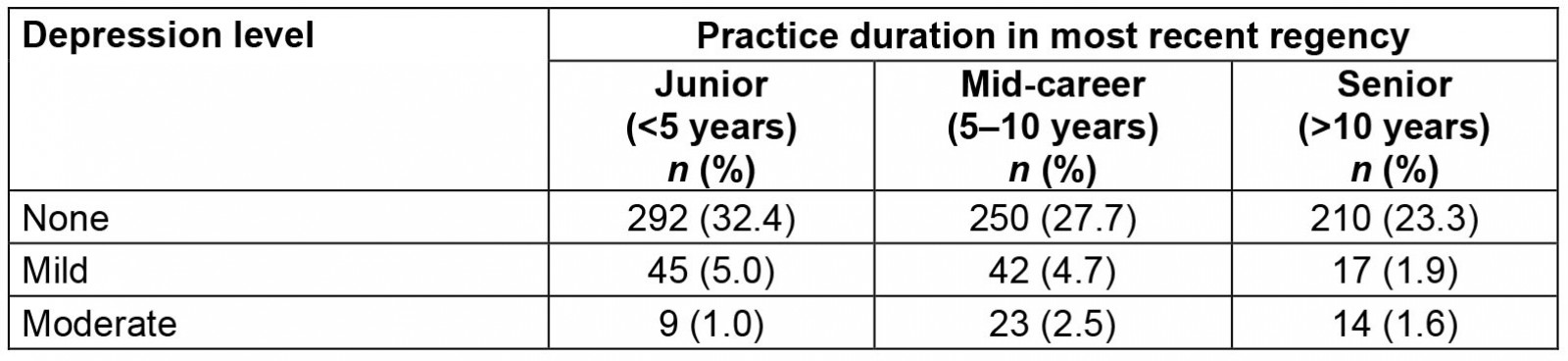
Resilience and depression levels
The Kruskal–Wallis results showed significant differences between depression levels in all resilience dimensions (Table 8). We conducted further pairwise comparisons to see which groups differed from each other (Table 9). The pairwise comparison showed that the moderately depressed group differed significantly from the non-depressed group in all dimensions except endurance. However, this moderately depressed group was not different from the mildly depressed group in any dimensions. In addition, half of the dimensions (three out of six) differed between the non-depressed and mildly depressed groups.
Table 8: Resilience profile by dimension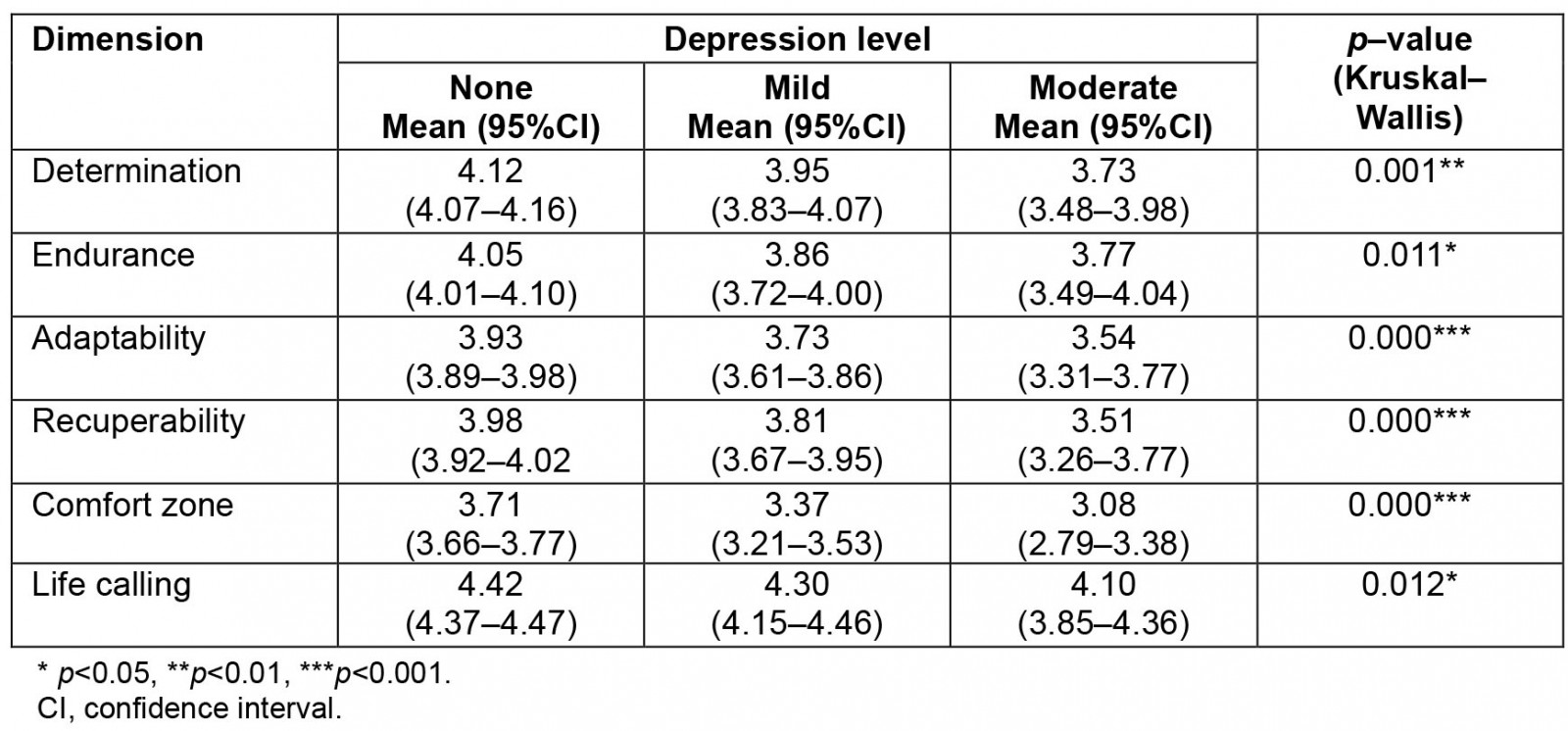
Table 9: Pairwise comparison results of resilience dimension scores between depression levels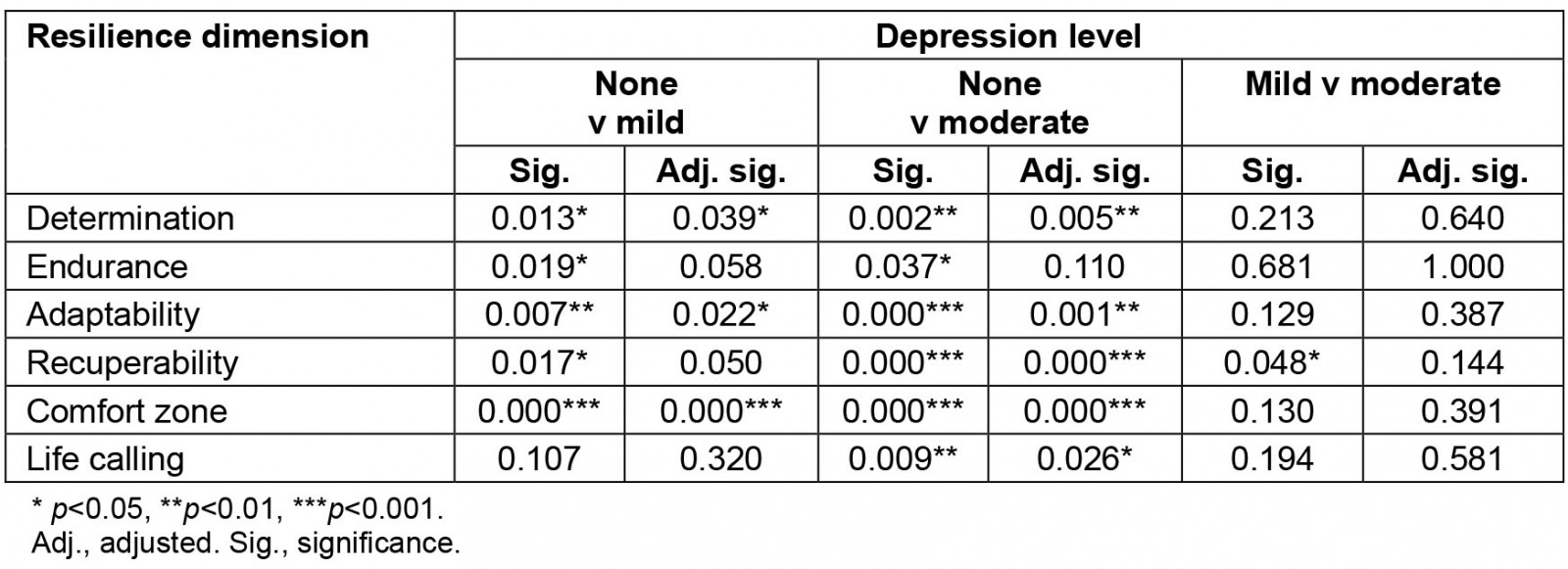
Discussion
This study measured the effect of resilience and depression on nurses’ retention in rural areas. Consistently, the senior group reported the least resilience, and the mildly depressed group reported the shortest retention. Also, the higher the depression level, the lower the resilience scores in all dimensions. Although not all hypotheses are met, some interesting phenomena are observable in the data.
Many studies have talked about improving health practitioners retention in rural and underserved areas2,38-41 but only a few compare urban–rural retention rates, depression prevalence42, and resilience. A previous study found that depression prevalence is higher in rural than in urban populations (6.1% v 5.2%) due to different population characteristics. However, the odds of depression are not different when the data are adjusted for rural–urban population characteristics42. Our study confirms no difference in the work duration, depression, and resilience scores between underserved and non-underserved regencies. A possible explanation is that the population under study is relatively homogenous (nurses). A more comprehensive study involving several regions with more heterogeneous characteristics is needed to confirm this finding.
Our first hypothesis, that the more senior the nurses, the higher their resilience, was not supported. The Spearman’s rank correlations showed significant negative results (opposing our hypothesis) for all dimensions, except for comfort zone. However, a more detailed analysis (Table 3) dividing the retention groups into junior, mid-career, and senior groups showed that the mid-career group reported the highest resilience, although not significant. Only the senior group is significantly lower compared to the other groups.
This finding contrasts with a previous study on rural doctors in which the senior doctor group had the highest resilience score29. Further detailed comparisons show even more contrasting results. The present study’s senior nurse group reported significantly lower resilience than the younger groups in three dimensions: determination, recuperability, and life calling. Conversely, the senior doctor group in the previous study29 reported significantly higher resilience than the young doctor group in two dimensions: endurance and comfort zone. It means the interventions to improve healthcare workers’ resilience or retention in rural areas should be tailored to each profession. Further studies are needed to answer these questions.
This result contradicts those of a previous systematic review stating that inexperienced or younger healthcare workers had lower resilience due to less social support43. However, there are some possible explanations for our findings. We collected data during the COVID pandemic in which the more senior a health practitioner is, the more vulnerable they are to severe health effects of COVID-1944. The low-resource setting (such as lack of personal protective equipment, medication, and facilities) in the studied province, lack of trust in the local health system’s capability to handle COVID-19, and the senior nurses’ health may have reduced their resilience during the pandemic. A previous study suggests that individuals with lower social and economic resources are more vulnerable to depression during pandemics18. The confidence in self-protection is related to healthcare practitioners’ mental health22,24. Furthermore, social distancing requirements may have reduced the social support that used to be available to seniors before the pandemic. For example, seniors are usually valued as leaders of social gatherings with extended families related to Indigenous traditions and ceremonies (such as burial and marriage) restricted during the pandemic. A previous study has discussed the importance of social support in preventing adverse mental health outcomes22.
Our second hypothesis, that the depressed groups would have lower retention, was partially met. In our study, the mildly depressed group had the shortest practice duration, for both province and most recent regency, compared to the other groups. This result supports our hypothesis. However, the moderately depressed group had the most extended working duration compared to the other groups. The logical explanations are that mildly depressed people would be unhappy, try to find a better place, and then move. So, retention is reduced. On the other hand, moderately depressed people may not be capable of finding another place and be reluctant to face changes and uncertainties in a new location. According to Beck, people experiencing major depression see only failures and a hopeless future45.
Our last hypothesis, that depressed groups would have lower resilience scores, was supported. Table 8 shows that the higher the depression level, the lower the resilience scores in all dimensions. Our findings confirm a previous preliminary study in which nurses’ resilience differed between the depressed and non-depressed groups46. However, the comfort zone dimension did not differ in the previous study, in which participants were nurses in the COVID ward of one hospital. Three dimensions (determination, adaptability, and comfort zone) in the present study differed between the non-depressed and depressed groups (mild and moderately depressed). In contrast, the other two dimensions (recuperability and life calling) differed only between the non-depressed and moderately depressed groups. Only endurance did not differ between the depressed and non-depressed groups, after adjustment. Since no difference exists between the depressed groups (mild and moderate), it is logical to conclude that resilience is essential in the preventive stage (before a person becomes depressed). In our opinion, any intervention to prevent depression should be directed toward strengthening the three dimensions of determination, adaptability, and comfort zone, which differ between the non-depressed and mildly depressed. Further studies are needed to explore the best way to strengthen these dimensions.
Implications of the findings
Our findings suggest mild depression may cause low retention, and that resilience negatively correlates to depression. Also, three dimensions (determination, adaptability, and comfort zone) differ between the non-depressed and mildly depressed groups. It is essential to strengthen these three dimensions to prevent depression and hopefully lead to better retention. Also, depression treatment should focus on those who are mildly depressed to support nurses’ retention. Further studies are needed to explore the best approach to strengthening the three dimensions and their impact on reducing depression and increasing retention.
Comparing our findings on nurses and a previous study’s findings on doctors in the same province shows large differences. In doctors, the more senior, the higher the resilience29. In the present study, the senior nurses’ group reported the lowest resilience among nurses. They also showed different significant dimensions of resilience. Thus interventions to improve healthcare workers’ retention in rural areas must be tailored to the each profession’s need. Unlike doctors, improving resilience may not directly answer the nurses’ retention problem. Further studies are needed to understand the reason for resilience differences in nurses and doctors and to explore better-tailored approaches to improve each profession’s retention.
Limitations
The questionnaire distribution through the WhatsApp group may have limited participants to nurses in those groups or to those with an internet connection. However, the proportion of participants suits the ratio of registered nurses. Thus, the generalisability of the findings is not compromised. The number of registered nurses’ data also shows differences between the nurses’ professional organization and the health ministry. We decided to use the nurses’ professional organization data since it is more up to date. A cross-sectional design of this study may limit our understanding of the changes in the resilience and depression levels over time on nurses’ retention. However, this study laid a good foundation for a more comprehensive study.
Conclusion
Our findings suggest that nurses’ resilience negatively correlates to depression and retention. However, mild depression shows the lowest retention. Thus, unlike doctors, resilience training in nurses may not be directly related to improved retention but may indirectly benefit retention through mild depression treatment.





