Introduction
Sarcopenia directly impedes daily activities in the older population, increasing the time spent in bed and shortening the healthy lifespan of the aging population1-3. The trunk of the human body includes a large number of skeletal muscles. Among them, the back extensor muscles, including the erector spinae and multifidus, play an important role in maintaining spinal stability4.The diminishing strength of the back extensor muscles leads to a reduction in the lumbar lordosis angle, which is known to impair an individual’s physical capacity and contribute to an increase in the prevalence of low back pain5. A lumbar magnetic resonance imaging analysis reported that the higher the degree of fatty degeneration of the erector spinae muscle, the greater the decrease in the height of the intervertebral disk and more extensive the degenerative changes in the vertebral body6.
Spinal sagittal balance (SSB), a key factor in spine health, is an important outcome indicator used to confirm the effectiveness of surgical and non-surgical spinal treatments7,8. The lumbar lordosis angle, a representative indicator of SSB, decreases with aging and causes lumbar kyphosis. Although vertebral compression fractures are an important pathologic mechanism of degenerative kyphosis, muscular atrophy and fatty infiltration of the back extensor muscles are closely related to degenerative kyphosis that causes a forward curvature of the upper back and flat back syndrome and a loss of the normal curvature of the lower back. Both can be associated with decreased body function and chronic lower back pain6,7. Therefore, a deeper understanding and a therapeutic approach to the back extensor muscles that affect SSB are needed.
Modern Korean society shows a large difference in the distribution of urban and rural populations because there is a significant difference in the occupational sectors between urban and rural areas. In particular, a lack of medical facilities and welfare are emerging as important health problems for older people in rural areas9. In addition, older individuals living in urban versus rural areas experience different daily activity levels, occupations, and environmental factors, which can greatly affect spinal health. In one study comparing physical activity and health status of urban and rural older women in Japan10, they reported that older women in rural areas had greater handgrip strength and walking speed than older women in urban areas but a higher prevalence of back pain. In particular, it is important to check and care for the health status of elderly women in rural areas. About 80% of elderly women in rural regions reported experiencing four or more health issues, in contrast to 63% of elderly men in rural regions. Additionally, a higher proportion of women than men (36% v 32%) reported encountering difficulties with activities of daily living11.
Therefore, it is important to compare the spinal health status and sarcopenia of older populations of urban versus rural areas and identify health indicators and variables for the prevention and treatment of spinal degeneration. Furthermore, preventing and treating sarcopenia and spinal degeneration in older adults is crucial in reducing medical expenses and enhancing quality of life.
This study aimed to: investigate the correlation between sarcopenia, SSB, and spinal function in older women aged more than 70 years living in a rural area (Sunchang County); and compare the sarcopenia variables of older rural and urban women to the data of previous study12 conducted on women more than 70 years living in urban areas (Seoul).
Methods
Study population
The study was conducted in September 2020 and included community-dwelling older women aged more than 70 years in Sunchang County, Jeollabuk-do province, South Korea. The number of participants for each 5-year age group was matched with those living in an urban area (Dongjak-gu, Seoul) included in the previous study12. If the target number of participants in a particular age group was first met, other age groups were recruited. Participants were recruited by the posting of ‘Announcement on Recruitment of Research Subjects’ notices on bulletin boards in Sunchang Medical Center. The inclusion criteria for the study were community-dwelling, ambulatory with or without an assistive device, willingness and ability to provide written consent before participating, and ability to comply with the study requirements.
The exclusion criteria were: lower back pain with moderate severity (score ≥5 on a numerical rating scale of 0–10); history of any type of lumbar spine surgery; history of hip fracture surgery or arthroplasty of the hip or knee; central nervous system disorder (eg stroke, Parkinsonism, spinal cord injury); communication disorder (eg severe hearing loss); musculoskeletal condition affecting physical function (eg limb amputation); long-term use of corticosteroids due to inflammatory disease; malignancy requiring treatment within the previous 5 years; other medical conditions requiring active treatment; and refusal to participate.
Demographic data and medical history
Demographic and socioeconomic data (eg marital status, family, education level), physical activity and exercise participation according to the Korean version of the Physical Activity Scale for the Elderly (K-PASE) survey13, and occupational status (current and past occupations under the Korean Standard Classification of Occupations) were investigated. The medical history and physical examination included vital signs (blood pressure, heart rate), past medical history (eg type of medication taken, history of hospitalization and surgery, history of falls), recent body weight change, and history of smoking and drinking.
Sarcopenia work-up
Bioelectric impedance analysis (BIA) (InBody 720; https://shop.inbodyusa.com/products/inbody720-result-sheets) was used to analyze body composition, including lean body and fat masses. Appendicular skeletal muscle mass (ASM) was calculated by obtaining the sum of the lean masses of the bilateral upper and lower extremities14 and dividing by the squared height value (ASM/Ht2 (kg/m2)). Handgrip strength (HGS) in both hands was measured using a handgrip dynamometer (TKK5401; https://www.pandamed.co.uk/product/takei-4501-digital-dynamometer)15,16 as described previously17. Briefly, while sitting in a straight-backed chair with their feet flat on the floor, participants were asked to adduct and neutrally rotate the shoulder, extend the elbow, and place the forearm in a supine position with the wrist at 0–30° of extension and 0–15° of ulnar deviation. The subjects were instructed to squeeze the handle as hard as possible for 3 s, and the maximum contraction force (kg) was recorded. Gait speed was measured using a 6 m usual gait speed test (m/s) with moving start as recommended by the Asian Working Group for Sarcopenia, guidelines from which the definition and cut-offs of sarcopenia were also adopted18.
Functional examinations and questionnaires
The functional examination used the short physical performance battery (SPPB) derived from three objective physical function tests (ie the time taken to cover 4 m at a comfortable walking speed, the time taken to stand five times from sitting in a chair without stopping, and the ability to maintain one’s balance for 10 s in three different foot positions at progressively more challenging levels)19. A score of 0–4 was assigned to rate the performance of each task, with higher scores indicating better lower body function.
The Timed Up and Go (TUG) test was administered; it has shown excellent test–retest reliability in older adults20. Participants were given verbal instructions to stand up from an armchair, walk 3 m as fast as possible, turn back at a cone set out by the researchers, walk back, and sit down in the chair. They were allowed to wear their regular footwear and use a walking aid if needed. A stopwatch was started on the word ‘go’ and stopped when the subject was fully seated with their back against the seat back. The time to complete the test was recorded in three consecutive trials, and the first trial was used to familiarize the subjects with the test. The best time from the three trials was analyzed21.
The Oswestry disability index (ODI), among the most commonly used instruments for measuring disability in spinal disorders, consists of 10 items that assess pain level and interference during several physical activities. We used the Korean version of the ODI22.
The back performance scale (BPS) consists of the sock test, pick-up test, roll-up test, fingertip-to-floor test, and lift test. These five tests are associated with each other, and each contributes to high internal consistency, implying that the tests share an ability to measure physical performance23. The BPS sum score (0–15) is calculated by adding the individual scores of the five tests.
Isometric back muscle strength
We measured isometric back extensor strength using a hand-held dynamometer (PowerTrack II; https://www.healthproductsforyou.com/p-jtech-commander-powertrack-ii-muscle-tester.html)24. Briefly, each participant stood in full extension with their back to a wall and feet flat on the floor with heels touching the wall. An inelastic belt was looped through the anchor rails and secured firmly 1 cm below the anterior superior iliac spine to restrain movement and maintain participant contact with the wall during the test. Participants were instructed to flex forward approximately 15° at the hips so that the dynamometer could be positioned posterior to the spinous process of the seventh thoracic vertebrae. In this way, counter pressure was provided by the fixed wall behind the back to avoid variations in resistance being introduced by the tester. This test showed a strong positive relationship with back extensor strength from the gold standard isokinetic dynamometry as well as inter-instrument validity and reliability25.
Spinal sagittal balance
SSB can be defined as the trade-off between outside forces acting on the spine and the muscle response of the trunk to maintain stable upright posture26, and can be measured through several indicators of the spine and pelvis using a simple X-ray examination. For each patient, a lateral radiograph of the whole spine was obtained and digitized. All measurements were performed using imaging software (INFINITT PACS M6; https://www.infinitt.com/about-us/our-story.php?ctr=g_eng) as previously described27,28. Briefly, the following spinopelvic radiographic parameters were analyzed: sacral slope, pelvic incidence (PI), pelvic tilt (PT), lumbar lordosis, thoracic kyphosis, and sagittal vertical axis.
Three-dimensional measurement of lumbar extensor muscle by computed tomography
All participants were examined by CT scan (Revolution EVO; https://www.gehealthcare.ca/en-ca/products/computed-tomography/revolution-evo-gen-3). Before each CT scan, calibration was performed using air as the standard. CT scanning was performed with each patient in the supine position with a routine lumbar CT scan protocol at 120 kV and 140 mA. Using 0.625 mm thin-section axial CT scan images, three-dimensional (3D) volume rendering and multiplanar images were reformatted using a radiological workstation (MEDIP; https://medicalip.com) specially designed for such purposes. We used a semiautomatic 3D segmentation algorithm, the graph-cut technique29, for volumetric muscle segmentation with MEDIP. During the segmentation procedure, the musculoskeletal radiologist with more than 15 years of experience repeatedly modified and confirmed the segmentation results using MEDIP.
The volume and mean density (in Hounsfield units (HU)) of the lumbar extensor muscle (LEM; multifidus and erector spinae) were calculated from the 3D segmentation of the LEM muscle. The total volume of the LEM, including intramuscular fat tissue, was measured by segmentation from the upper endplate of the first lumbar vertebra to the lower endplate of the fifth lumbar vertebra. The mean density of the LEM was also calculated as the average HU value of the pixels within the LEM volume and reflected the degree of intramuscular fat content because the HU values decreased as the fat content increased. Additionally, predefined HU ranges (–29 to +150 HU) were used to measure the volume of the LEM without intermuscular fat tissue (Fig1).
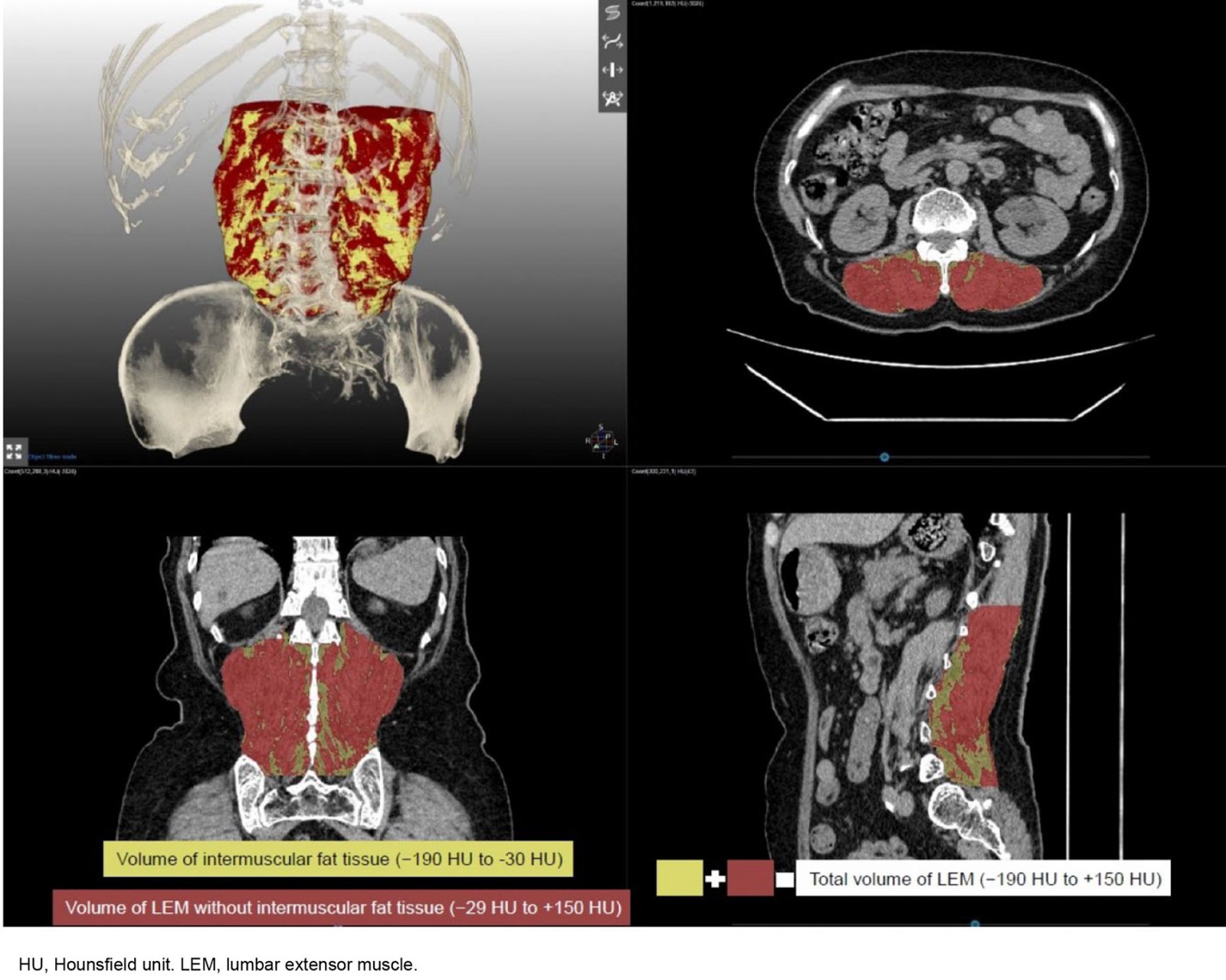 Figure 1: Three-dimensional segmentation of lumbar extensor muscle. The total volume of lumbar extensor muscle with intramuscular fat tissue displays between −190 and +150 HU, and predefined HU ranges were used to demarcate intramuscular fat tissue (yellow volume, −190 to −30 HU), and muscle tissue (brown volume, −29 to 150 HU).
Figure 1: Three-dimensional segmentation of lumbar extensor muscle. The total volume of lumbar extensor muscle with intramuscular fat tissue displays between −190 and +150 HU, and predefined HU ranges were used to demarcate intramuscular fat tissue (yellow volume, −190 to −30 HU), and muscle tissue (brown volume, −29 to 150 HU).
Statistical analysis
The relationships between sarcopenic indices and functional outcomes with SSB parameters, LEM volume, and density were measured using Pearson correlation coefficients. The average demographic, functional, and imaging test results were compared between the rural and urban groups and were analyzed using the Student’s t-test. In addition, the χ2 test was used to compare the ratios. Statistical Package for Social Sciences v21.0, for Windows (IBM Corp., https://www.ibm.com/products/spss-statistics) was used for all analyses. Statistical significance was set at p<0.05.
Ethics approval
This study was conducted in accordance with good clinical practice and the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. This study was approved by the Institutional Review Board of SMG-SNU Boramae Medical Center (30-2020-15). Written informed consent was obtained from all subjects.
Results
Demographic and clinical characteristics of rural versus urban areas
A total of 25 older rural women were enrolled in the study, and their data were compared with those of 24 older urban women in a previous study. There were no significant intergroup differences in age, height, weight, or body mass index. Among the indicators of sarcopenia, there was no difference in ASM and ASM/Ht2, but rural women had a greater mean HGS than urban women (22.7±3.7 kg v 20.0±3.4 kg, p=0.010). The mean gait speed also tended to be faster in rural women than in urban women, but the difference was not significant (0.93±0.14 v 0.87±0.16 m/s, p=0.176). The SPPB, chair stand test, and TUG test results did not differ significantly between the two groups, but the mean physical activity level measured by the K-PASE was higher in rural women than in urban women (130.4±63.6 v 95.5±32.8, p=0.024) (Table 1). There was no difference in the prevalence of sarcopenia assessed by the Asian sarcopenia diagnostic criteria (16% in rural area v 17% in urban area).
Table 1: Comparisons of body composition and performance between older women in rural (Sunchang) and urban (Seoul) areas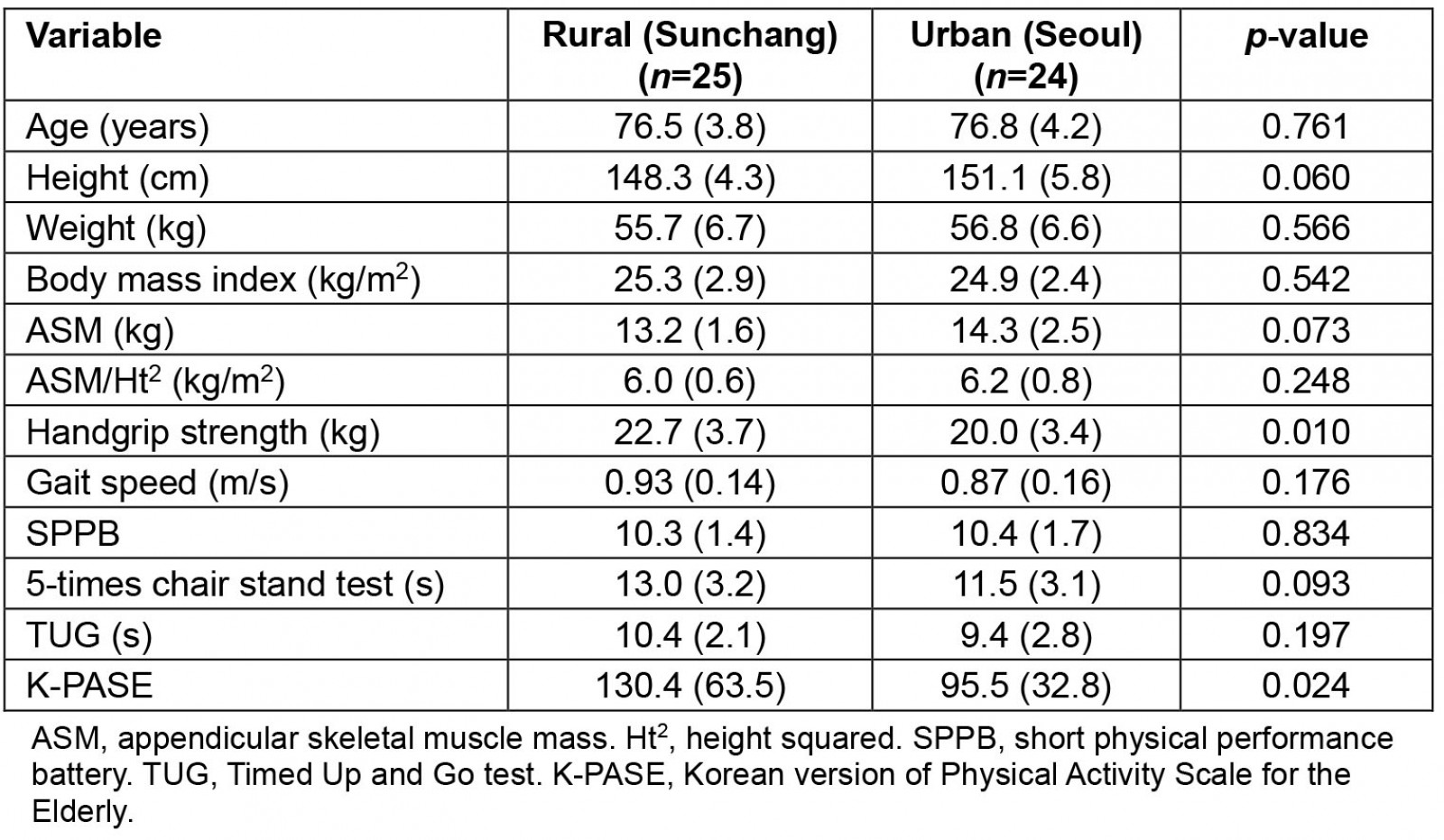
Spine imaging and spinal function
Mean lumbar lordosis angle was smaller in rural women than in urban women (31.7°±15.3° v 42.3°±11.2°, p=0.012). Rural women had greater mean PT and PI than urban women (26.5±6.4° v 22.1±6.9°, p=0.030; 62.9±10.9° v 51.7±12.7°, p=0.002). In the 3D volumetric analysis of the LEM, the total volume and mean density of the LEM with intermuscular fat tissue as well as that without intermuscular fat tissue did not differ between the two groups. In the spinal function evaluation, the mean isometric back extensor strength was smaller in rural women than in urban women (30.0±9.4 N v 40.0±12.6 N, p=0.002). The mean ODI score was greater in rural women than in urban women (13.1±7.4 v 8.3±5.8, p=0.017) (Table 2).
In the correlation analysis of the functional and imaging parameters of the spine, only PI showed a negative correlation with isometric back extensor strength (r=–0.472, p=0.001). There was a positive correlation approaching significance between the strength and volume of the LEM without intermuscular fat tissue (r=0.276, p=0.057) (Fig2A). Isometric back extensor strength and lumbar lordosis angle were not clearly correlated (r=0.028, p=0.854) (Fig2B).
Table 2: Comparisons of radiographic and functional outcomes between older women in rural (Sunchang) and urban (Seoul) areas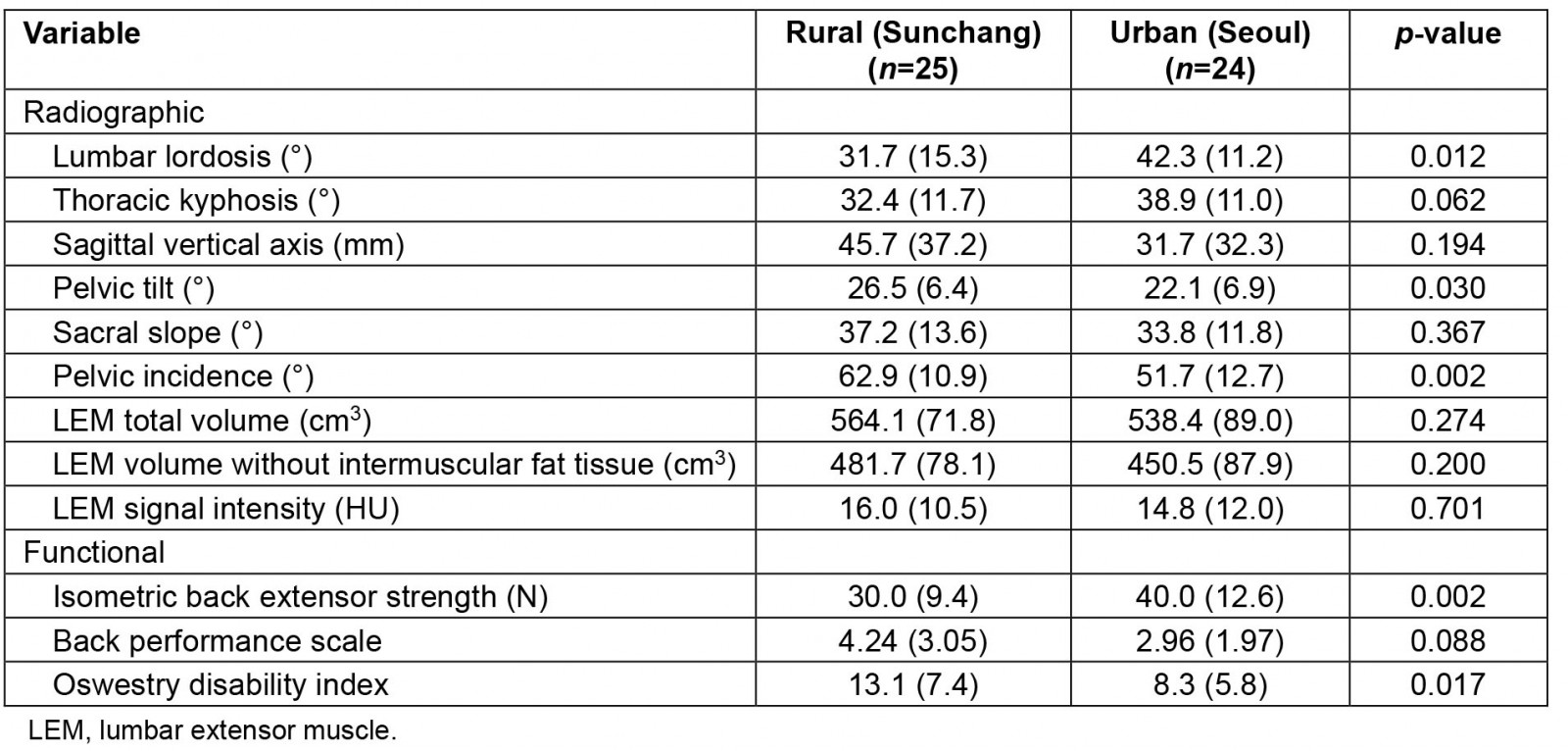
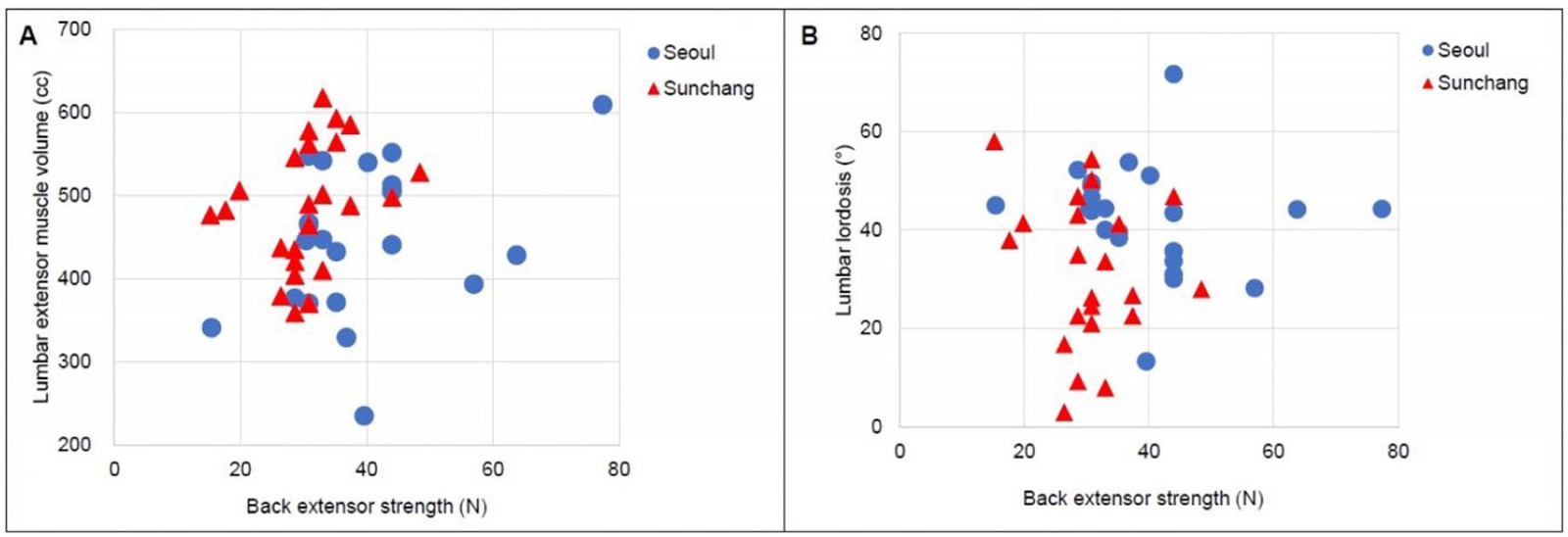 Figure 2: Correlation between back extensor strength and (A) lumbar extensor muscle volume and (B) lumbar lordosis angle.
Figure 2: Correlation between back extensor strength and (A) lumbar extensor muscle volume and (B) lumbar lordosis angle.
Occupational state and exercise participation
Only three of the 24 urban women versus 21 of the 25 rural women were employed (p<0.001). The largest proportion (26%) of the older women in Sunchang County were engaged in agriculture, forestry, and fishing, followed by simple labor (21%). The participation rate of light, moderate, vigorous, and resistance exercises performed more than once a week was lower in rural women than in urban women. In addition, the rate of exercise participation regardless of type was significantly lower in rural women (60%) than in urban women (92%) (p<0.001).
Discussion
This study investigated the sarcopenia, SSB, and spinal function of older women aged more than 70 years in a rural area (Sunchang County) versus an urban area (Seoul). Older women in rural areas had a greater HGS than those in urban areas, and significantly more of them were employed. However, they had weaker back extensor muscle strength and poorer SSB index scores than those in urban areas. In addition, their exercise participation rate was lower than that of older women in urban areas.
Sunchang County of Jeollabuk-do province in South Korea is a representative aging area, with 31.29% of the population aged more than 65 years, exceeding the Jeollabuk-do average (18.26%) as of 2016 statistics and more than doubling the Korean average (13.49%); thus, the county may already be classified as a super-aged area. We recruited older women in a rural area at 5-year age intervals (70–74, 75–79, 80–84, ≥85 years) to age match them with older women in urban areas included in a previous study12. As a result, the mean age of the rural and urban areas was 76.5 and 76.8 years, respectively, and direct group comparisons were possible. Rural older women had a greater mean HGS (22.7±3.7 kg v 20.0±3.4 kg, p=0.010) and tended to have a faster gait speed (0.93±0.14 m/s v 0.87±0.16 m/s, p=0.176) than urban older women. The difference was similar to the degree of physical activity measured by the K-PASE (130.4±63.6 v 95.5±32.8, p=0.024).
The greater HGS, gait speed and physical activity level in older rural women might be related to their higher employment level. Only 12.5% of older urban women are currently employed compared with 84.0% of older rural women. Despite being older women aged more than 70 years, our subjects continued to be engaged in high-intensity agriculture or simple labor jobs and performed more physical activity than older urban women. Koo reported the results of a comparative analysis between older urban and rural Korean individuals30. Similarly, they reported that older individuals in rural areas were twice as likely to be employed than those in urban areas; and older women in rural areas were 1.4 times more likely to be employed than older men in rural areas30.
The opposite result was seen with participation rates in leisure-time and occupation-related exercise. The K-PASE survey revealed that participation rates in light, moderate, and strength exercises performed at least once a week were lower in older rural women than in older urban women. However, participation rates in exercise regardless of type was significantly lower in rural women (60%) than in urban women (92%). This can be explained by the fact that interest in sports is higher in urban areas because the sports infrastructure is better and that older women in urban areas who are not engaged in vocational activities have more leisure time. Goode et al conducted a telephone survey of 2006 residents living in North Carolina, US, and compared the prevalence of chronic lower back pain and hospital utilization in rural versus urban areas9. Rural residents showed significantly lower rates of hospital use and physical therapy prescriptions than urban residents. As such, the difference between urban and rural infrastructure such as hospitals and exercise facilities, which are important for the good health of older community-dwelling individuals, has a significant impact on the early diagnosis and treatment prognosis of chronic diseases and degenerative spinal diseases31.
Contrasting labor and exercise participation rates between the two groups were associated with differences in spinal imaging and function. Although the volume and CT signal intensity of the LEM analyzed on 3D lumbar CT scans did not differ between the two groups, back extensor muscle strength was weaker in rural women than in urban women (30.0±9.4 N v 40.0±12.6 N, p=0.002). The mean ODI score was also greater (more disabled) in rural women than in urban women (13.1±7.4 v 8.3±5.8, p=0.017). This difference in spinal function was also related to the SSB index score, which ultimately represents the degree of spinal curvature. The lumbar lordosis angle was lower in rural women than in urban women, and rural women had greater PT and PI angles than urban women. Thus, we suggest that older women in rural areas, who are more engaged in occupational work rather than exercise, have lower spine function levels than older women in urban areas. As a result, the spines of rural older women are more kyphotic than those of urban older women.
Kim et al surveyed the overall activity and physical activity levels of 113 farmers living in Gangwon-do, Korea32. They reported that farming work increases the probability of musculoskeletal disorders because it involves motions performed repeatedly in the same posture for a long period of time, unlike the athletic activity of athletes and non-farmers. Similarly, in this study, older rural women were found to have higher ODI values associated with lower back pain than older urban women. It can be inferred that this group is more vulnerable to musculoskeletal diseases such as lower back pain because the occupation rate is higher in agriculture, forestry, fishery, and simple labor.
Dual-energy X-ray absorptiometry (DEXA) or BIA has been used to measure limb muscle mass for the diagnosis of sarcopenia. However, with DEXA and BIA, the muscle mass of the trunk is calculated together with the visceral muscles of the internal organs, so it is impossible to measure the independent skeletal muscle mass of the back extensor muscles. Therefore, to directly measure the spinal extensor muscle, it is necessary to measure the cross-sectional area of the muscle by tomographic methods such as CT or magnetic resonance imaging33. In this study, the LEM volume was calculated by reconstruction of the 3D lumbar CT scan. These data were analyzed in the same way based on the research results published by Kim et al12. However, instead of drawing the area directly, the researcher selected the muscles from the lumbar spine CT scan by a semiautomatic technique based on the graph-cut algorithm in this study. The process first used the algorithm based on several areas chosen by the radiologist, and the result was confirmed and corrected by the researcher. Through this process, the volume measurement time can be significantly reduced, and advanced methods can be applied to ensure accuracy and reliability.
This study has several limitations. First, we recruited subjects without severe lower back pain (<5 points on the numeric rating scale for the last 3 months) to evaluate the functional imaging of the spinal muscles of healthy older women. However, ODI score, which evaluates the degree of lumbar dysfunction, was greater in rural women than in urban women. Therefore, we cannot exclude the possibility that the difference in lumbar disability between the two groups might affect the differences in back extensor strength and lumbar lordosis angle. To prevent this bias expected in the research planning, participants without severe back pain were selected, but the sensitivity of 5 points for the numerical rating scale was considered inferior for screening the degree of lumbar disability.
Second, the main purpose of this study was to compare the spine and back muscle-related parameters of older women in rural areas (conducted in 2020) and urban areas (conducted as a preliminary study in 2018). However, the global COVID-19 pandemic and the resulting quarantine and social distancing have greatly affected the physical activity and exercise participation rates of older individuals. Therefore, we cannot completely rule out the impact of the COVID-19 pandemic based on the fact that older rural women contacted during field visits in 2020 had lower exercise participation rates than older urban women in 201834.
Third, this study primarily focused on the biomechanical aspects of back pain, and thus psychological, social, and environmental factors were overlooked. To address this, we compared the occupational participation rates between the two groups as one social factor, but were unable to compare other factors.
Finally, this was a comparative analysis of older urban and rural women aged 70 years or more. However, the sample size was very small, within 30 for each group, and the subjects were not sufficiently representative of the area. In addition, it is possible that older urban women lived in rural areas in the past or that older rural women may have returned home from cities. Therefore, it will be necessary to compare the results of this study with those of an analysis in which the number of study subjects is sufficient, using big data such as National Health Insurance data in the future on the same subject.
Conclusion
In conclusion, this study compared sarcopenia, SSB, and spinal function in older women in rural and urban areas. Older women in rural areas had greater HGS and higher vocational participation rates but less back extensor strength and lower exercise participation rates. Therefore, more attention for healthcare services is needed to support their spinal health and exercise habits.
Funding
This work was supported by the Sunchang County and Seoul National University Institute on Aging Grant funded by Sunchang County in 2019 (0564-20190012), the National Research Foundation of Korea grant funded by the Korean government (Ministry of Science and IT) (2022R1C1C1006283, 2022R1A5A2021216), and a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health and Welfare, Republic of Korea (HI19C0481, HC20C0157).
Conflicts of interest
The authors declare they have no competing interests.

