Introduction
Residents of rural and remote communities have well-established healthcare challenges that lead to poorer health outcomes than their urban counterparts, including recruitment and retention of healthcare professionals1. In order to recruit more rural healthcare workers and increase health services to these communities, efforts are being made in some Canadian academic programs to increase the number of rural students admitted, as they are more likely to return to rural areas to practice1. While important, these initiatives are hindered by the fact that health science programs struggle to recruit rural applicants; therefore, rural students are underrepresented in health science programs2. There is increasing recognition that early intervention strategies targeting rural youth should be explored2.
Rural youth face many barriers that discourage them from applying to healthcare programs2. As per the zone of proximal development theory3, most youth are capable of learning the skills and steps needed to do this on their own but might not do so without encouragement and assistance from others. Given that rural residents often obtain lower educational levels than their urban counterparts, and since rural communities typically have smaller networks of professionals, a notable barrier to entry for rural students is a lack of experienced people able to provide that support2. Without role models to promote and guide them towards healthcare careers, it can be hard for rural youth to imagine themselves as a healthcare professional, and they often must navigate the journey to a post-secondary health science program on their own2.
Mentoring programs have long been valued for their ability to connect youth with positive role models, as mentors have been shown to influence youths’ educational and career decisions and subsequently help youth achieve their future goals4,5. These benefits extend to mentoring programs promoting health sciences to rural youth6, although this has not been attempted on a large scale, as delivering services to rural areas is challenging5. Online mentoring, which has the same positive impacts as in-person mentoring7, is ideal for rural areas because it circumvents these challenges, which include issues with transportation to and from events, lack of institutional support and funding, and mentor recruitment5.
Although Canadian rural youth can join online mentoring platforms such as MentorCity, they must seek out these opportunities, which are not rural or healthcare focused. Online mentoring programs delivered in rural schools have been more successful at reaching rural youth, although the only program in Canada that attempted this is no longer operating, despite its positive impacts, and was not healthcare focused7. Therefore, although online mentoring shows promise as a way to inspire and support rural youth to pursue healthcare careers, it has yet to be attempted by the rural healthcare community, so its actual impacts are unknown.
We addressed this gap in knowledge by developing, implementing and evaluating an online mentoring program that matched rural youth in British Columbia with near-peer health science students, called Rural eMentoring BC (ReMBC). The program’s goal was to positively affect rural youths’ attitudes towards, and abilities to pursue, a rural healthcare career. We evaluated whether we met this goal by measuring our success against four anticipated outcomes, each of which is a necessary step towards building a career in rural health care:
- interest in healthcare careers
- intention to attend post-secondary education
- interest in working in a rural community
- resourcefulness in finding, and willingness to seek out allies.
This study brings us one step closer to understanding whether online mentoring can be useful in promoting and guiding rural students towards health science programs, in which they are underrepresented, and ultimately increasing the number of rural healthcare professionals.
Methods
Study design
We applied a design-based research (DBR) methodology to our program and study. DBR was originally developed as a means to improve the application of education research into practice8. As such, DBR involves developing and then making iterative changes to an intervention, the ultimate goal of the intervention being seamlessly integrated into real educational environments9,10. DBR is an appropriate methodology for our study, as ReMBC was developed based on an identified need (lack of connection to resources and role models with post-secondary experience) and was tested, evaluated and refined based on the research described below.
Program development
ReMBC was developed through a partnership between a faculty member at the University of British Columbia and the province’s Rural Education Action Plan. The program was structured so that each rural youth mentee was paired, one to one, with their own mentor, based on their shared career and educational goals. The dyads communicated via asynchronous messaging through an online platform, MentorCity, and were encouraged to write to their match a few times each week. We followed a ‘near-peer mentoring’ model rather than engaging healthcare professionals, as near-peers are more easily relatable and less intimidating for youth to interact with11. Throughout the program, mentors, many of whom were from rural areas, were expected to share their own journey to becoming health science students.
While most virtual mentorship models typically follow an unstructured approach, where mentors and mentees have free-flowing discussions, consultations with secondary school stakeholders led us to believe that, as adolescents, the mentees would benefit from some structure within their mentoring relationships. This led us to build a semistructured curriculum called the Personal Quest, which included readings, videos, or activities that the mentees would complete, and then discuss with their mentor through conversation prompts. The Personal Quest was organized into eight themed units intended to promote career exploration and prepare students for the transition to post-secondary education. We hypothesized that these would be useful discussion topics because, for many rural youth, this might be their only chance to talk to someone with experience in these areas. Students completed the units in the following order: study habits, internet safety, allies, goal setting, career decisions, money and spending, exploring post-secondary, and planning for post-secondary.
The curriculum was developed by a rural secondary school teacher in British Columbia, with the intent that its content would complement the learning goals for Career Life Education and Career Life Connection courses that secondary school students in British Columbia are required to take. Rather than design entirely original content, the curriculum aimed to harness already existing online content in order to increase participants’ awareness of the wealth of resources available to them beyond the program.
Mentee recruitment and participation
Mentees were recruited through their schools at the beginning of each school year. We advertised the program to schools in communities covered by the Rural Practice Subsidiary Agreement, as qualified by the Rural Coordination Centre of British Columbia’s community isolation rating system12. Five secondary schools, each from a different geographic region of British Columbia (Northeast, Thompson/Cariboo, Kootenay Boundary, East Kootenay, and North Vancouver Island), responded to our advertisements and, in total, these schools enrolled 364 students in the program.
Schools participated by requiring the program as part of their careers classes, or by advertising the program to students who could then participate voluntarily, although only two students chose this option. A total of seven careers classes ranging from grade 7 to grade 11, with most being grade 10, participated. Although mentees were encouraged to write to their mentors at least twice a week, this was unenforceable, so contact frequency depended on how the mentees participated, with most writing to their mentor when they were given class or homework time, which ranged from once or twice a week to once a month. Similarly, relationship length depended on how the mentees participated, with most limiting their relationships to the duration of their courses, which ranged from a few weeks to the length of the school year, although some students continued to participate voluntarily after their courses ended. The number of units completed depended on the length of the relationship and the frequency of communication; 210 students completed at least one curriculum unit and 55 students completed all eight units.
Mentor recruitment, training and participation
The ReMBC staff created a database of health science post-secondary programs in British Columbia and emailed program administrators at the start of each school year, asking them to share our call for volunteers. Prospective mentors contacted us and were screened based on an interview and criminal record check. This broad outreach provided us with a diverse mentor pool totaling 115 students from 15 different health science programs at 13 different post-secondary institutions in British Columbia. Mentors were studying medicine, nursing, kinesiology, pharmacy, psychology, social work, neuroscience, biology, respiratory therapy, public health, animal science, physical therapy, occupational therapy, biotechnology and dentistry. Mentors were invited to return to the program at the start of each school year, with more than one-third of mentors volunteering for more than 1 year.
Mentors received a training manual that contained our program’s policies, mentor expectations, instructions for navigating the program, and information on respectful engagement. Mentors were paired with one mentee at a time, except in a few cases, and were expected to remain engaged in that relationship until their mentee completed the curriculum or completed their course. Mentors were also required to respond to their mentee within 3 days, and unresponsiveness would result in removal from the program and rematching of the mentee.
Data collection and analysis
All participants were invited to partake in voluntary online surveys administered through the MentorCity platform. Survey questions were designed by the project team to gauge the impact of the program on participants and to evaluate whether the program was meeting the intended goals. We found that many of these survey questions were useful for this study and thus used the secondary data collected from these surveys. We applied a pre–post repeated-measures design to our study, as mentees were surveyed when they joined the program and then were asked the same questions after the appropriate curriculum unit. At the end of the program, mentees could also take part in a final program evaluation, which included short-answer type questions, designed to capture their overall impressions of the program. However, due to management error, the program evaluation was only offered to four of the participating classes and one of the two students who participated voluntarily – 209 students in all. Survey questions explored mentees’ career preferences, educational goals, interest in working rurally, resourcefulness in finding and willingness to seek help, and can be seen in Tables 1 and 2. Mentors were surveyed at the conclusion of each school year in order to capture their attitudes towards the program, how it helped them professionally, the adequacy of their training and the quality of their relationships. We used this feedback for program improvement purposes, and it is not included in this study.
We used thematic analysis13 to analyze participants' written responses to the program evaluation. We coded the responses and identified themes among them. Although we used an inductive approach, we looked for themes regarding participant-perceived program impact, including what participants learned, found helpful and enjoyed. Then we reviewed the responses to ensure the themes we identified represented the data. Finally, to determine the most prevalent participant-determined program impacts, we counted the number of times each theme was mentioned.
Survey data were analyzed using R v3.6.2 (R Foundation; https://www.r-project.org). For categorical-type data, we used McNemar tests to assess whether changes in answers between the pre- and post-program surveys were non-random. To analyze Likert-scale data, we used paired Wilcoxon tests with survey time (pre- v post-program) as the independent variable, and rating as the dependent variable. Non-parametric tests were used because our data did not meet normality assumptions, and we treated our Likert-scale data as ordinal.
Table 1: Number of students interested in healthcare careers and who anticipate attending post-secondary education; results of McNemar test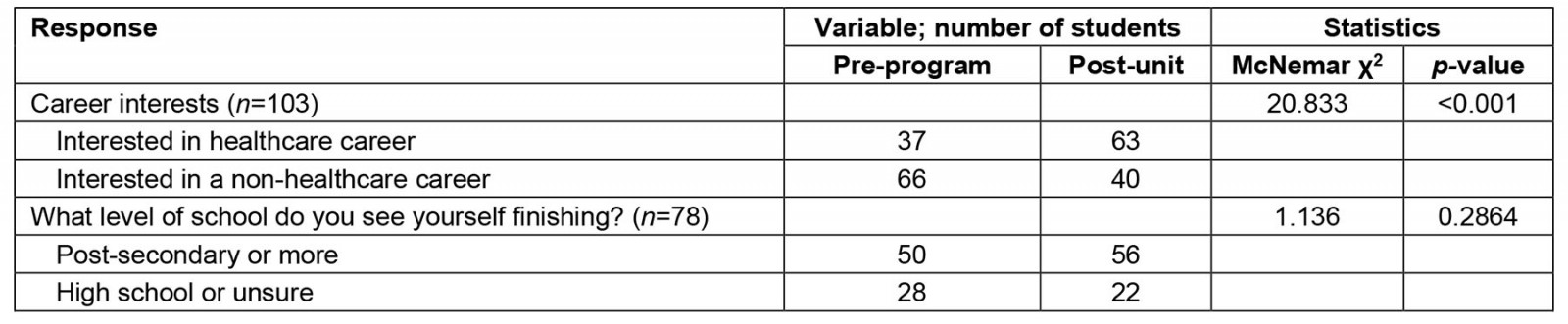
Table 2: Mean and standard deviation of responses to Likert scale survey questions, differences in means of responses and 95% confidence intervals, and results of Wilcoxon tests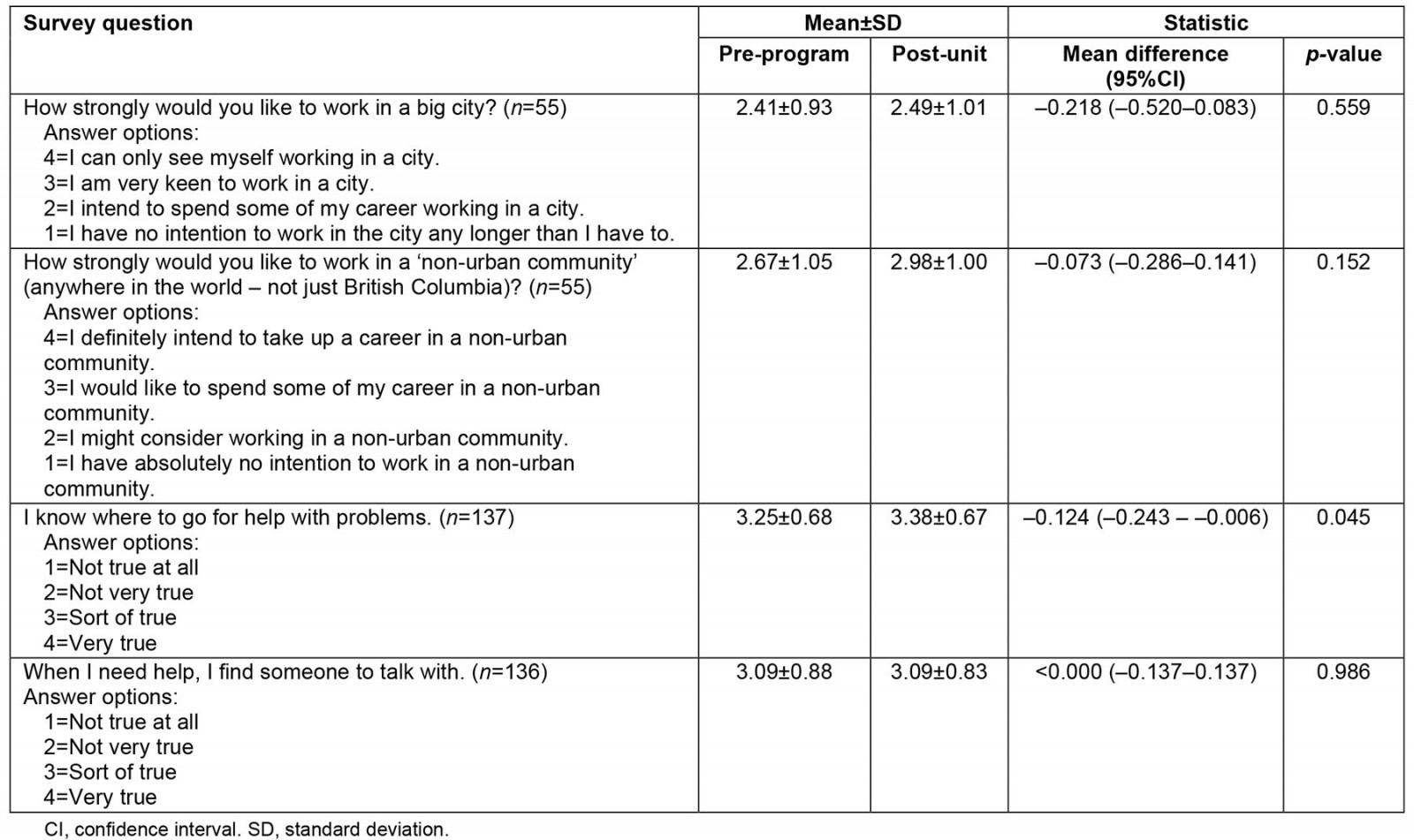
Ethics approval
All participants were informed during registration that ReMBC would collect data from the MentorCity platform to conduct a program evaluation. All data were de-identified prior to analysis. We obtained ethics approval through the University of British Columbia’s Behavioral Research Ethics Board (H18-02940).
Results
The following sections describe the intervention’s impact on the four constructs we sought to explore: interest in healthcare careers, post-secondary education, working in a rural community and resourcefulness and willingness to seek allies.
Overall program impressions – thematic analysis
Twenty percent of participants (41 students out of 209) elected to take the program evaluation survey and provide feedback on the program by responding to short-answer questions. Thirty-seven respondents indicated that they found the program helpful, and their responses fell into four themes: their relationships with their mentors, information on post-secondary education, career support, and learning life skills. Regarding post-secondary education, students appreciated learning about different institutions and their offerings, speaking with someone in a post-secondary program, and identifying the requirements for their desired programs. Responses mentioning career support highlighted the value of the resumé creation and career exploration activities. Life skills mentioned included learning how to pay for school and gaining an awareness of issues of equity and access. Finally, students enjoyed learning from their mentors and developing a personal connection with them. The four students who did not find the program helpful commented that it was too focused on healthcare careers, and this was not their interest, or that their mentor was unresponsive. The number of mentions for each theme, as well as representative quotes, can be seen in Table 3.
Table 3: Themes of responses to short-answer questions, with examples and number of mentions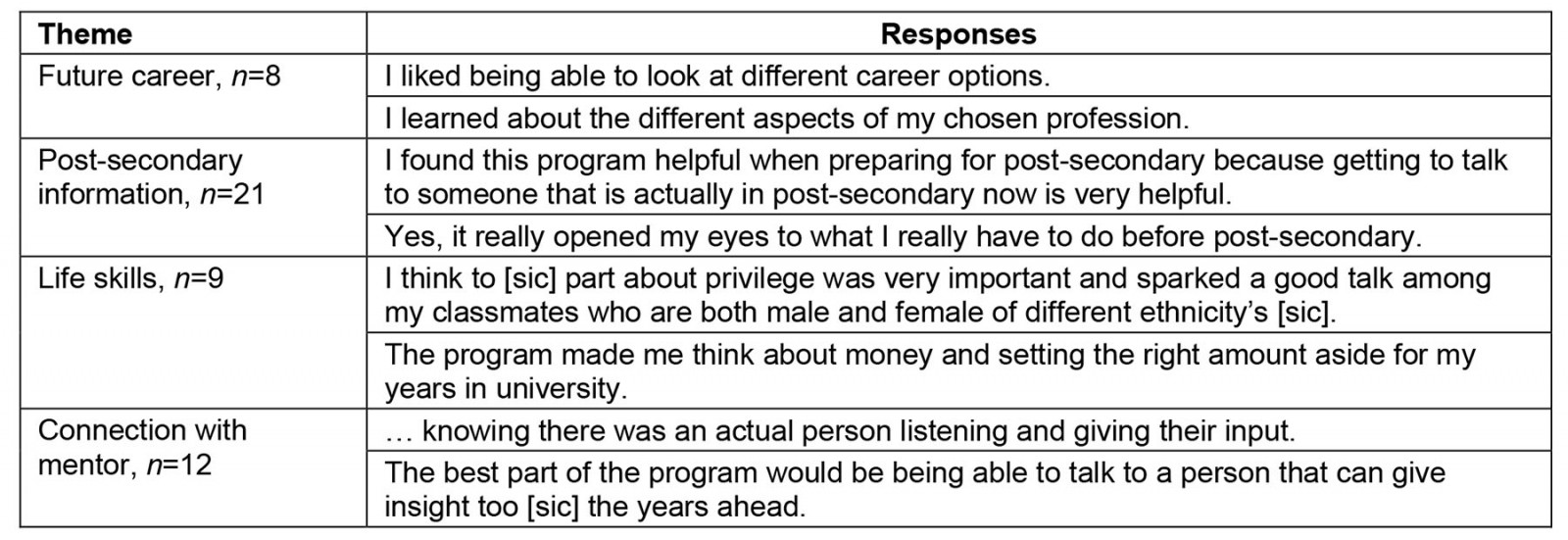
Attitudes towards healthcare careers, post-secondary education, working rurally, and allies
One hundred and three students completed the unit on career exploration and 78 completed the unit on post-secondary considerations. Significantly more students indicated that they were interested in healthcare careers after completing the career exploration unit than before (37 before and 63 after, Table 1); however, their attitudes towards post-secondary education did not change significantly after completing the units focused on post-secondary education (Table 1). After participating in the program, 14 respondents changed their answers from ‘not continuing past high school/unsure’ to ‘attending post-secondary’, and eight respondents switched their answers in the opposite direction; therefore, the overall number of students planning on attending post-secondary education remained relatively similar throughout the program (50 before the program, 56 after).
On average, both before and after completing the unit on allyship (137 students completed this unit), students indicated that it was ‘sort of true’ that they knew where to find help, and that they would seek help (Table 2). For ‘finding help’, we found a statistically significant pre- and post-effect in our Wilcoxon tests, as several students indicated that they felt more confident about finding help after this unit; however, the overall means shifted very little (3.24 before, 3.38 after, out of 4 on our Likert scale).
After the final unit, which 55 students completed, participants were re-asked about their attitudes towards working in a rural community. Most students indicated that they would at least consider working in a rural community (47 before and 50 after, out of 55) and that they intended to spend some of their career in an urban community (48 before and 47 after, out of 55). Their answers did not change significantly while they participated in the program (Table 2).
Discussion
Our study sought to understand how online mentoring relationships could affect rural youths’ decisions to pursue a career in rural health care, and their preparedness for transitioning to health science programs. We evaluated their career preferences, post-secondary school goals, interest in working in a rural community, and resourcefulness in finding and willingness to seek help, using surveys deployed before and after the program. We hope that our study can serve as proof of concept that online mentoring is a practical and effective tool for engaging rural students, who are underrepresented in health science programs.
Our results suggest that the program sparked interest in health care in a group of students who were, mostly, already willing to attend post-secondary education to meet their career goals, who were willing to work in a rural community, and who would ask for help along their journey. Qualitative answers suggest that these students would be more prepared to meet these goals due to the program, as they indicated that they found the program helpful in planning for post-secondary education, navigating financial aid, exploring their institution and program options, learning about admissions, and learning life skills. Given that conversations with a mentor can help reinforce and maintain goals and positive habits in the long term14, the intervention has the potential to set participants up for long-term success.
We attribute the shift in students’ attitudes towards healthcare careers to a few factors. First, the students indicated that the intervention helped them explore different career options, which could have exposed them to healthcare careers they had not considered or known about.
Also, the intervention could have shown students that a healthcare career is achievable, especially since the program left students feeling more prepared for the transition to post-secondary education. In addition, youth are often influenced by psychosocial factors, including exposure to role models and how they think others perceive them15, which helps explain why mentoring relationships have been shown to affect youth career preferences4.
Limitations
The order of the curriculum units could have factored into the responses we collected because the more motivated students were more likely to finish more units. For example, the unit on post-secondary education was last and had the lowest completion rate; it is possible that students who were already intending to attend post-secondary education were more likely to complete this unit, which could account for the observed lack of change in attitudes towards post-secondary education. Similarly, we did not have any content on rurality, so it is unsurprising that attitudes towards working rurally did not change during the program.
External influences on students during the program, such as interactions with peers, teachers or counsellors, could have also affected our results. Many of these students participated in the program as part of a careers class and concurrently received information about career options and requirements, and post-secondary education from their teacher. However, the short-answer questions asked students to write what they gained from their participation in the program, which allowed us to identify what they learned from the program versus what they learned from other sources.
Lessons learned
In line with the DBR methodology, after evaluating the intervention, we determined that the following refinements could help further the positive impact that this program has on rural youth. The efficacy of these changes as they affect rural student enrollment and ultimately rural healthcare practitioner recruitment should be assessed in future studies.
Focus on personalized goals: Since students already favorably viewed post-secondary education, practising rurally, and finding and using allies before participating in the program, its future iterations should help students maintain these values. Other studies4,14 have shown that students stay motivated, maintain good habits, and reach their goals when they trust their mentors, can ask them questions, and feel comfortable sharing their thoughts, feelings, and fears with them; thus, these actions should be encouraged within the curriculum. The curriculum should also feel personal to the mentees, and encourage them to define their values, identify their assets, and make a plan to meet their unique career and educational goals.
Moreover, the program might have a larger impact on students if they are able to customize the curriculum content by choosing the order in which to complete the units. This way, they are likely to complete the units most useful to them first, just in case they stop the program before completing all the units. Rural youth are not a monolith, so allowing for choice and personalization can help make outreach efforts to this group successful.
Other topics to include: We should also incorporate topics that were not covered in the curriculum but that pairs were discussing anyway. In particular, mentees were interested in discussing wellbeing/self-care, ‘adulting’, and the differences between high school and post-secondary education. Their popularity aside, these concepts are worth discussing because mentoring has been shown to improve both mental health and the outcomes of transitional phases in life4. Given that mentees opened up to their mentors about their feelings towards moving far from home and living in a city while attending post-secondary education, discussing these topics could have important impacts on how rural youth view the transition to health science programs.
Additionally, given the program’s goal to promote careers in rural areas, the curriculum should provide opportunities to discuss the values of living and working rurally, as well as promote conversations around demystifying the rural–urban transition – as many rural youth feel unprepared for this change when moving to an urban center for school.
Meet the needs of Indigenous participants: Given that 15% of our participants were Indigenous, our program should also meet the needs of Indigenous youth. Refinements to the intervention should include more Indigenous voices, resources and representation in the curriculum, and consider a less linear structure within the program, as a way to incorporate Indigenous ways of knowing. We encourage other mentoring programs to also incorporate these principles into their offerings to support Indigenous students’ transitions to health science programs and address issues of underrepresentation.
Conclusion
Based on the shortage of rural healthcare practitioners, and evidence that rural students return to their communities to practice, ReMBC was developed to encourage rural youth in British Columbia to pursue a career in rural health care and show them how to do so. We found that the program successfully increased participant interest in healthcare careers and helped them acquire the knowledge and skills needed to transition into post-secondary education. Our study also showed us where to improve, including enabling personalization within the curriculum, adding new discussion topics relevant to rural youth, and meeting the needs of rural Indigenous learners; we hope that those attempting to develop similar programs in rural areas will consider these points. Although our results are encouraging, future studies should determine if efforts like these actually increase rural student representation in health science programs, and ultimately increase the number of rural healthcare professionals. ReMBC is limited to British Columbia’s rural areas, but we hope that this study encourages health science programs, rural health organizations and rural communities to develop similar programs for rural youth worldwide.
Funding
The program described in this research was funded by the Joint Standing Committee on Rural Issues.
Conflict of interest
The authors declare no conflict of interest.




