Introduction
Universal health coverage (UHC) is a concept that seeks to ensure that all people have access to quality essential health care without financial hardship1. Achieving UHC requires expanding access to medical care, and while strengthening the primary healthcare (PHC) system is essential for all countries, it is particularly critical in low- and middle-income countries like Paraguay, where limited healthcare infrastructure, resource constraints, and workforce shortages make PHC the most effective and sustainable approach to delivering equitable healthcare services2. Broadening the universality of PHC services is an essential area of universal health care, and many studies are being conducted in this area3. However, studies evaluating the capacity of facilities providing PHC services in developing countries are not being actively conducted4. In recent years, policymakers in low- and middle-income countries have increasingly prioritized UHC and the expansion of healthcare services as part of their national health strategies. While significant progress has been made in expanding service coverage, capacity-building in PHC facilities remains a challenge due to resource constraints, workforce shortages, and health system fragmentation in many settings5-7. This often results in an imbalance where expanding access receives more focus than improving the quality and resilience of healthcare delivery systems. This situation hinders the effective provision and expansion of primary healthcare services in developing countries. Accordingly, the need for an assessment tool to evaluate and improve the capacity of PHC facilities in these countries has emerged.
The WHO has developed several tools to assess the quality and accessibility of health care, including the Service Availability and Readiness Assessment (SARA) tool8. The WHO SARA tool is used in various countries to assess the quality and accessibility of basic healthcare services, assess the capacity of facilities and personnel involved in the delivery of PHC services, and inform policymakers and decision-makers about how to improve healthcare services. The SARA tool is a standardized instrument designed to measure the availability of essential health services and the readiness of health facilities to deliver those services. It assesses key service domains, including basic amenities (eg water supply, electricity), basic equipment (eg diagnostic tools), infection prevention measures, diagnostic capacity, and the availability of essential medicines. Each domain is evaluated using specific indicators that provide quantitative data, enabling comparisons across health facilities and over time. The tool facilitates evidence-based decision-making by identifying gaps in service delivery and resource allocation.
Paraguay has set the National Health Plan 2014–2030: For a Healthier Paraguay (Plan Nacional de Salud 2014–2030: Por una Paraguay más saludable)9. This national plan sets out targets for health indicators in Paraguay from 2014 to 2030 and provides a roadmap on how to improve the quality of and access to health care in Paraguay. The four key areas of Paraguay's national healthcare strategy are (1) strengthening the healthcare system and services, (2) improving health outcomes and reducing health inequalities, (3) promoting healthy lifestyles and preventing disease and (4) ensuring the sustainability of the healthcare system10. Achieving these strategic goals includes improving the quality and accessibility of health care, increasing the availability of essential medicines and medical equipment, and extending health care to vulnerable populations. However, despite the Paraguayan government's efforts to improve the quality and accessibility of health care, several challenges remain. Paraguay faces challenges related to both the shortage and maldistribution of healthcare professionals, particularly in rural areas. According to the latest data, Paraguay has an average of 1.2 physicians per 1000 population and 2.8 nurses per 1000 population, which is below the regional average for South America11. However, the issue extends beyond overall shortages to include significant disparities in the distribution of healthcare workers, with urban areas having a higher concentration of medical professionals compared to rural and remote regions. This maldistribution contributes to unequal access to healthcare services, impacting the readiness and quality of primary healthcare delivery.
This study aimed to investigate the service readiness of public healthcare facilities in Paraguay, utilizing the WHO SARA tool. The study sought to identify areas for improvement, inform policy decisions, and enhance the overall quality and accessibility of healthcare services. Additionally, it addressed the necessity for an assessment tool that evaluates and enhances the capacities of PHC facilities in developing countries, specifically in Paraguay.
Methods
Research area
The research area of this study is Limpio, Central Department, Paraguay, which is approximately 40 minutes by car from Asuncion, the capital of Paraguay. The total population of Limpio is 155,465, and it is a mixed area comprising urban and rural areas12. The number of public health and medical centers in the research area increased from seven in 2018 to 20 in 2021. This increase in the number of public health centers was supervised by the Ministry of Health and Welfare of Paraguay, with financial support from the Korea International Cooperation Agency. The newly constructed health center began operating in May 2021.
Research design
This difference comparison study used a community-based control area to identify the effects of interventions such as public health and medical center construction, human resource training, and operational support provided in the research area before and after the intervention. The time points of the survey were 2018 (before the intervention) and 2021 (after the intervention), and the items of the WHO SARA tool common to the intervention and control areas were investigated (Fig1). The study included a total of 23 public healthcare centers, with 20 intervention areas and three control areas compared and analyzed. Then, the WHO SARA scores in 2018 and 2021 were compared, the differences were analyzed, and the effectiveness of the intervention was evaluated.
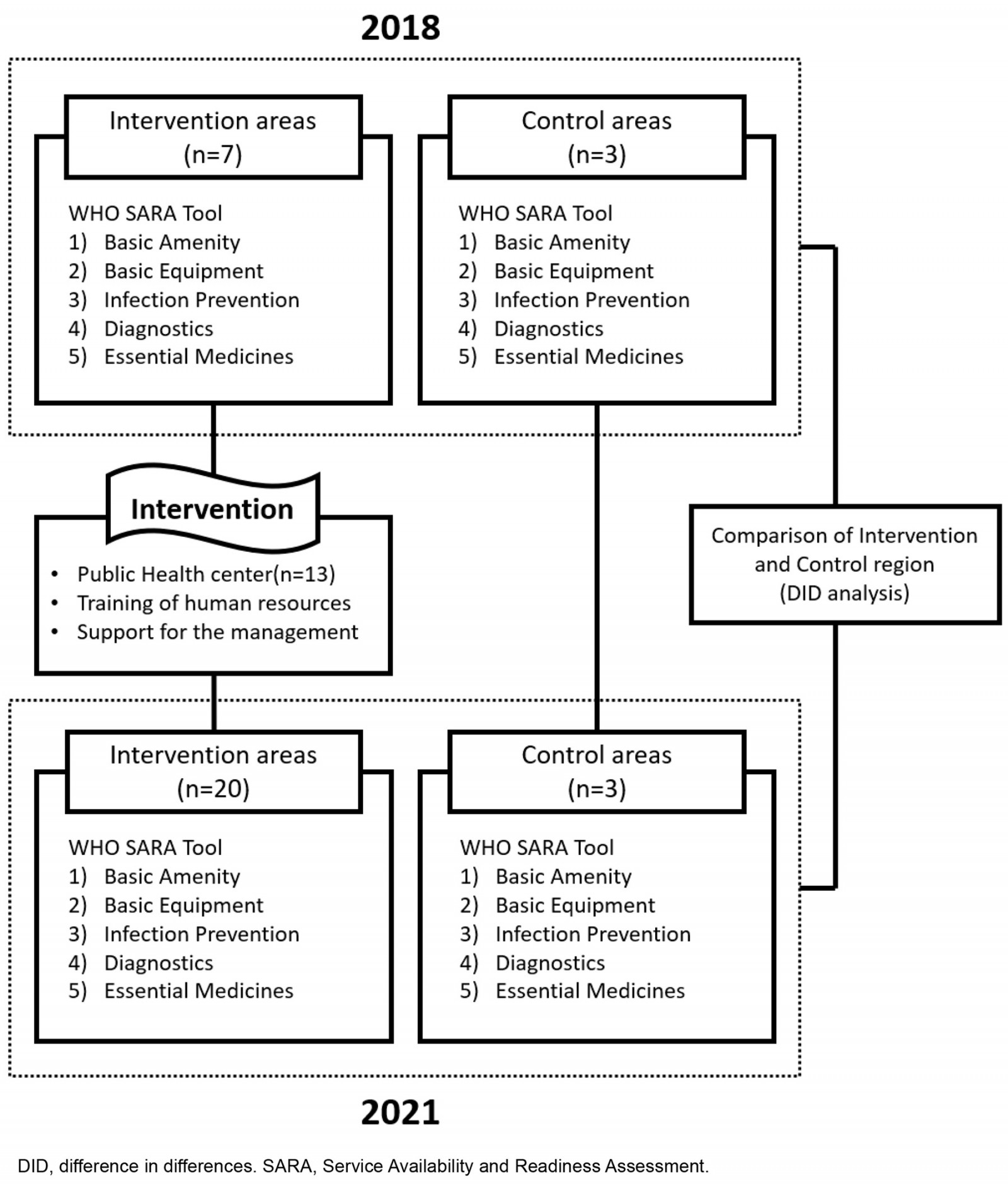 Figure 1: Research design, describing intervention and control areas.
Figure 1: Research design, describing intervention and control areas.
Study tool and data collection
Public healthcare facilities in Paraguay
Paraguay has public healthcare facilities called Unidades de Salud de la Familia (USFs), which are divided into standard public health centers (estándar USFs) and expanded public health centers (ampliada USFs) according to the function and role of the facility and personnel composition13. Paraguay's PHC center is the basic architectural infrastructure of Paraguay's health service, providing health promotion, prevention, diagnosis, treatment, and health education14. The standard health center provides PHC to approximately 5000 residents and ensures cultural, geographical, and medical access. The expanded public health center provides a higher level of PHC than the standard public health center, and functions such as maternal and child care, prenatal care, and dental care have been added.
Public health centers in Paraguay provide free medical services to visiting patients14. For public health care, the Ministry of Health and Welfare of Paraguay centrally manages all 18 regions nationwide and supports and operates medical personnel, essential medicines, and essential equipment.
WHO Service Availability and Readiness Assessment tool
The WHO SARA tool is a comprehensive approach to assessing the capacity of essential health services at the facility level using measurable standard indicators to determine the extent of minimum standards for healthcare delivery15. To evaluate the availability and readiness of medical services, the human resources of PHC facilities that provide medical services are identified and measured using evaluation tools. The evaluation tool consists of seven items for basic amenities, six items for basic equipment, eight items for infection prevention, eight items for diagnosis and treatment, and five items for essential medicines15.
Table 1: WHO Service Availability and Readiness Assessment tool variables used for constructing service readiness index (category score 0–100)
| Category | Items |
|---|---|
| Basic amenities (7 items) | Uninterrupted power source |
| Improved water source | |
| Private room for examination | |
| Client sanitation facilities | |
| Functional phone or shortwave radio | |
| Computer with email and internet | |
| Available emergency transportation | |
| Basic equipment (6 items) | Adult scale |
| Pediatric scale | |
| Thermometer | |
| Stethoscope | |
| Blood pressure apparatus | |
| Light source | |
| Infection prevention (8 items) | Safe sharps disposal |
| Safe infectious waste disposal | |
| Waste bin with lid and liner | |
| Surface disinfectant | |
| Single-use disposable syringes | |
| Hand sanitizer | |
| Latex gloves | |
| National infection guidelines | |
| Diagnostics (8 items) | Hemoglobin test |
| Blood glucose test | |
| Malaria test | |
| Urine protein test | |
| Urine glucose test | |
| HIV rapid test | |
| Syphilis rapid test | |
| Urine pregnancy test | |
| Essential medicines (5 items) | Calcium channel blocker and ACE inhibitor (antihypertensive) |
| Glibenclamide, and insulin injection (antidiabetic) | |
| Beclomethasone and salbutabom (anti-asthmatic) | |
| Fluoxetine and amitriptyline tablet (antidepressant) | |
| Amoxicillin syrup/dispersible tablet (antibiotic) |
Intervention
The intervention in this study was designed as part of a comprehensive health system strengthening initiative implemented in Limpio, Central Department, Paraguay. It aimed to enhance the service readiness of public healthcare facilities to deliver PHC services effectively. The intervention consisted of the following key components:
- construction of 13 Public Healthcare Centers: Thirteen new public healthcare centers were strategically constructed between 2018 and 2021 to improve geographical access to PHC services, particularly in underserved urban and rural areas. These centers included both standard health units (estándar USFs) and expanded health units (ampliada USFs), offering a range of services from basic outpatient care to specialized maternal and child health services.
- allocation of medical resources: Essential medical equipment, diagnostic tools, and pharmaceutical supplies were provided to each newly established facility. This included basic diagnostic kits, infection control materials, and life-saving medicines to ensure compliance with WHO SARA standards.
- human resource training and capacity building: Healthcare professionals, including doctors, nurses, midwives, and community health workers, participated in targeted training programs. The training covered critical areas such as infection prevention and control, chronic disease management, maternal and child health, and effective use of medical equipment. These programs aimed to enhance the clinical competencies and service delivery capabilities of healthcare workers.
- operational and technical support: To ensure the sustainability of healthcare service improvements, the intervention included ongoing operational support. This involved administrative assistance, health information system strengthening, and continuous monitoring and evaluation activities. Technical support was also provided to improve facility management, data reporting, and resource utilization.
Data collection
Data for this study were collected at two distinct time points to facilitate a longitudinal analysis of healthcare service readiness: prior to the intervention in 2018 and following the intervention in 2021. A standardized questionnaire, grounded in the WHO SARA framework, was employed consistently across both data collection periods to ensure methodological rigor and comparability.
The baseline survey, conducted from 13 September 2018 to 7 October 2018, established a reference point for assessing the pre-intervention status of healthcare facilities. The post-intervention follow-up survey, conducted between 29 July 2021 and 31 August 2021, was designed to capture changes in service readiness attributable to the implemented health system strengthening activities. Both surveys were meticulously administered by the same team of experts to maintain consistency and minimize inter-observer variability.
Data were obtained from 23 public healthcare centers, comprising 20 facilities in the intervention group and three facilities in the control group. The survey targeted key personnel within these facilities, resulting in a total of 68 respondents, including facility managers, healthcare professionals (such as doctors, nurses, and midwives), and administrative support staff. These individuals were selected based on their direct involvement in healthcare service delivery and facility management, ensuring that the data reflected informed, practice-based insights. Notably, the majority of participants possessed formal training in public health, healthcare administration, or clinical practice, thereby enhancing the reliability of the responses.
The data collection process incorporated both structured face-to-face interviews and direct on-site observations. Structured interviews were conducted to elicit detailed information regarding healthcare service delivery, resource availability, and operational challenges. Concurrently, on-site observations were employed to verify the physical presence of medical equipment, infrastructure adequacy, and the availability of essential supplies. To reduce the potential for recall bias, all data were collected contemporaneously with the facility visits, ensuring real-time verification of the reported information.
The multidisciplinary data collection team consisted of highly qualified experts, including one WHO/Pan American Health Organization coordinator, a health economist with a PhD, two statisticians with doctoral qualifications, as well as three public health physicians and one doctor of nursing. This diverse team provided a robust blend of technical, analytical, and clinical expertise, contributing to the comprehensiveness and accuracy of the data collection process. On average, each facility assessment required approximately 2 hours to complete, reflecting the thoroughness of the evaluation.
Analysis method
WHO SARA index
The WHO SARA index was calculated using the following equation:
WHO SARA index = total score obtained ÷ maximum possible score × 100
The WHO SARA index was scored according to the presence or absence of essential items for the five items and 34 indicators in Table 1, and the total score of the facility was obtained by summing the scores for each item. The total score ranged from 0 to 100, with a higher score indicating improved readiness and availability of essential health services12. The WHO SARA index is a useful tool for assessing the readiness and availability of essential health services in a healthcare facility or healthcare system. When comparing scores through the WHO SARA index, the scores for each item are evaluated by comparing them with the reference value, and the final evaluation is performed by comparing the total score of the WHO SARA index after comparing the scores for each item.
Difference-in-differences method
The analysis method used in the study is a difference-in-differences (DID) method, which is a method used to compare the difference in results between the experimental and control group before and after an intervention. DID examines the effectiveness of a specific policy or intervention program, judging whether the impact of change occurs and the extent of the impact16. It is an appropriate research method for evaluating the causal relationship between policies targeting developing countries and analyzing the difference in performance between the experimental and control group17. In this study, the results were measured by calculating the difference between the intervention group area and the control group area using the WHO SARA index for 2018 (before the intervention) and 2022 (after the intervention). Additionally, the difference in evaluation scores of the WHO SARA index was tested by conducting a Mann–Whitney U-test.
Ethics approval
This study was conducted with the approval of the Central Review Board (Institutional Review Board) of the Ministry of Health and Welfare of Paraguay (Ministerio de Salud Publica y Bienestar Social, MSPBS) (no. 136/05062018), and it was carried out on 8 December 2020, by completing the protocol approval of the Institutional Review Board of the Ministry of Health and Welfare of Paraguay (no. 156/2020).
Results
Healthcare human resources and WHO Service Availability and Readiness Assessment scores in the research area (2018, 2021)
Table 2 presents the healthcare human resources and WHO SARA scores for the intervention and control areas in 2018 (pre-intervention) and 2021 (post-intervention).
In 2018, the intervention area had an average of 0.4 doctors per facility across seven public healthcare centers, totaling three doctors. This indicates that most facilities did not have a full-time doctor, with doctors either shared among multiple centers or working part-time, leading to limited availability of medical consultations. The number of nurses was 0.6 per facility (total of four), and midwives were at 0.3 per facility (total of two), reflecting significant gaps in maternal and child healthcare services. The average number of community health workers (CHWs) was 1.7 per facility (total of 12), indicating that some centers operated with just one CHW, limiting their capacity for community outreach and preventive care. Additionally, there was one other personnel per facility (total of seven), including administrative and support staff.
In contrast, the control area in 2018, comprising three public healthcare centers, had one doctor per facility (total of three), ensuring consistent medical coverage. The number of nurses was two per facility (total of six), midwives were 0.3 per facility and CHWs averaged 2.7 per facility (total of eight), indicating better staffing levels compared to the intervention area. This discrepancy highlights the maldistribution of healthcare resources even before the intervention.
Following the intervention in 2021, the intervention area experienced significant improvements in human resources. The average number of doctors increased to 1.1 per facility (total of 22) across 20 healthcare centers, meaning most facilities had at least one dedicated doctor, improving service availability and patient access. The number of nurses increased to 1.5 per facility (total of 30), while midwife numbers increased to 1.1 per facility (total of 22), enhancing maternal and neonatal health services. The average number of CHWs increased markedly to 4.7 per facility (total of 94), significantly boosting community-based healthcare capacity, including health education, disease prevention, and follow-up care. The number of other personnel was 0.4 per facility (total of eight), reflecting an optimized workforce structure.
In the control area in 2021, the staffing levels remained relatively stable, with one doctor per facility (total of three), 1.7 nurses per facility (total of five), 0.7 midwives per facility (total of two), and 1.3 CHWs per facility (total of four). This minimal change underscores the impact of the intervention in the target area.
Table 2: Healthcare human resources, WHO Service Availability and Readiness Assessment index in research area
| Category | Human resources |
2018 n (n per facility) or SARA score |
2021 n (n per facility) or SARA score |
||
|---|---|---|---|---|---|
|
Intervention area |
Control area |
Intervention area (n=20) |
Control area (n=3) |
||
| Healthcare human resources | Doctor | 3 (0.4) | 3 (1.0) | 22 (1.1) | 3 (1.0) |
| Nurse |
4 (0.6) |
6 (2.0) | 30 (1.5) | 5 (1.7) | |
| Midwife |
2 (0.3) |
1 (0.3) | 22 (1.1) | 2 (0.7) | |
| Community health worker |
12 (1.7) |
8 (2.7) | 94 (4.7) | 4 (1.3) | |
| Others (eg cleaner, technician) |
7 (1.0) |
5 (1.7) | 8 (0.4) | 1 (0.3) | |
| WHO SARA index | Basic amenities (14 items) | 55.1 | 76.2 | 85.7 | 81.0 |
| Basic equipment (6 items) |
85.2 |
88.9 | 90.8 | 72.2 | |
| Infection prevention (9 items) |
71.0 |
77.8 | 78.3 | 81.5 | |
| Diagnostic capability (8 items) |
30.4 |
50.0 | 41.3 | 40.2 | |
| Essential medicines (5 items) |
56.6 |
58.5 | 59.4 | 52.8 | |
| Overall SARA score |
59.7 |
70.3 | 71.1 | 65.5 | |
SARA, Service Availability and Readiness Assessment.
Comparison of differences in WHO Service Availability and Readiness Assessment index score before and after intervention (2018, 2021)
The comparison of the WHO SARA index scores before and after the intervention (Table 3 and Fig2) reveals notable changes in service readiness across key domains. Using the DID method, we evaluated the extent to which the health system strengthening intervention influenced service delivery in the intervention area compared to the control area.
In terms of basic amenities, the intervention area scored 21.1 points less than the control area in 2018, indicating poor infrastructure conditions such as limited access to clean water, unreliable electricity supply, and inadequate sanitation facilities. However, by 2021, following the intervention, this gap had reversed, with the intervention area scoring 4.7 points more than the control area. The DID value for basic amenities was 25.8 points (p=0.003), demonstrating a statistically significant improvement. This positive change reflects the direct impact of infrastructure upgrades, including facility renovations and the provision of essential utilities, which contributed to creating a safer and more functional environment for both patients and healthcare providers.
For basic equipment, the intervention area had a 3.7-point deficit compared to the control area in 2018, indicating limited availability of essential medical devices such as stethoscopes, thermometers, and blood pressure monitors. After the intervention, this situation improved significantly, with the intervention area scoring 18.6 points more than the control area in 2021. The DID value for basic equipment was 22.3 points (p=0.018), signifying a statistically significant improvement. This suggests that the targeted provision of medical equipment as part of the intervention effectively enhanced the diagnostic and treatment capabilities of healthcare facilities.
In contrast, the results for infection prevention showed less dramatic changes. In 2018, the intervention area scored 6.8 points less than the control area, reflecting gaps in infection control measures such as sterilization practices, availability of personal protective equipment, and proper waste management systems. By 2021, the gap had narrowed slightly to 3.2 points, but the DID value was only 3.6 points (p=0.745), which is not statistically significant. This suggests that, although some improvements occurred, they were modest and may have been influenced by external factors, such as the national COVID-19 response, which likely affected both intervention and control areas similarly.
Regarding diagnostic capability, the intervention area was 19.6 points behind the control area in 2018, indicating severe limitations in access to basic diagnostic services like blood tests, urine analysis, and rapid diagnostic kits. After the intervention, the intervention area slightly outperformed the control area by 1.1 points in 2021, resulting in a DID value of 20.7 points (p=0.024). This statistically significant improvement highlights the intervention’s success in enhancing diagnostic capacity, enabling healthcare facilities to provide more comprehensive and timely diagnostic services, which are critical for effective patient management.
For essential medicines, the difference between the intervention and control areas was relatively small. In 2018, the intervention area scored 1.9 points less than the control area, and in 2021, it scored 6.6 points more. The DID value was 8.5 points (p=0.483), which is not statistically significant. This indicates that the availability of essential medicines remained relatively unchanged, possibly due to challenges related to national supply chain management or procurement processes, which were beyond the scope of the intervention.
Lastly, when considering the overall WHO SARA score, the intervention area scored 10.6 points less than the control area in 2018, highlighting substantial gaps in service readiness prior to the intervention. By 2021, this trend had reversed, with the intervention area scoring 5.6 points more than the control area. The DID value for the overall SARA score was 16.2 points (p=0.030), indicating a statistically significant improvement. This demonstrates the overall effectiveness of the intervention in enhancing the readiness of healthcare facilities to deliver quality primary healthcare services, particularly through improvements in infrastructure, equipment availability, and diagnostic capacity.
These findings suggest that, although the intervention had a substantial impact on certain domains, such as basic amenities, equipment, and diagnostic capability, other areas like infection prevention and essential medicines require additional targeted efforts to achieve similar levels of improvement. The results underscore the importance of integrated health system strengthening strategies that address both structural and operational components of service readiness.
Table 3: Evaluation of public healthcare facilities, according to the WHO Service Availability and Readiness Assessment tool (2018, 2021)
| Category | 2018 | 2021 | Effect (DID) | |||||
|---|---|---|---|---|---|---|---|---|
| Intervention (A) | Control (B) | D1 (A – B) | Intervention (A) | Control (B) | D2 (A – B) | D2 – D1 | p* | |
| Basic amenities (7 items) | 55.1 | 76.2 | –21.1 | 85.7 | 81.0 | 4.7 | 25.8 | 0.003 |
| Basic equipment (6 items) | 85.2 | 88.9 | –3.7 | 90.8 | 72.2 | 18.6 | 22.3 | 0.018 |
| Infection prevention (8 items) | 71.0 | 77.8 | –6.8 | 78.3 | 81.5 | –3.2 | 3.6 | 0.745 |
| Diagnostic capability (8 items) | 30.4 | 50.0 | –19.6 | 41.3 | 40.2 | 1.1 | 20.7 | 0.024 |
| Essential medicines (5 items) | 56.6 | 58.5 | –1.9 | 59.4 | 52.8 | 6.6 | 8.5 | 0.483 |
| Overall SARA score | 59.7 | 70.3 | –10.6 | 71.1 | 65.5 | 5.6 | 16.2 | 0.030 |
* Mann–Whitney U-test.
D, difference. DID, difference in difference. SARA, Service Availability and Readiness Assessment.
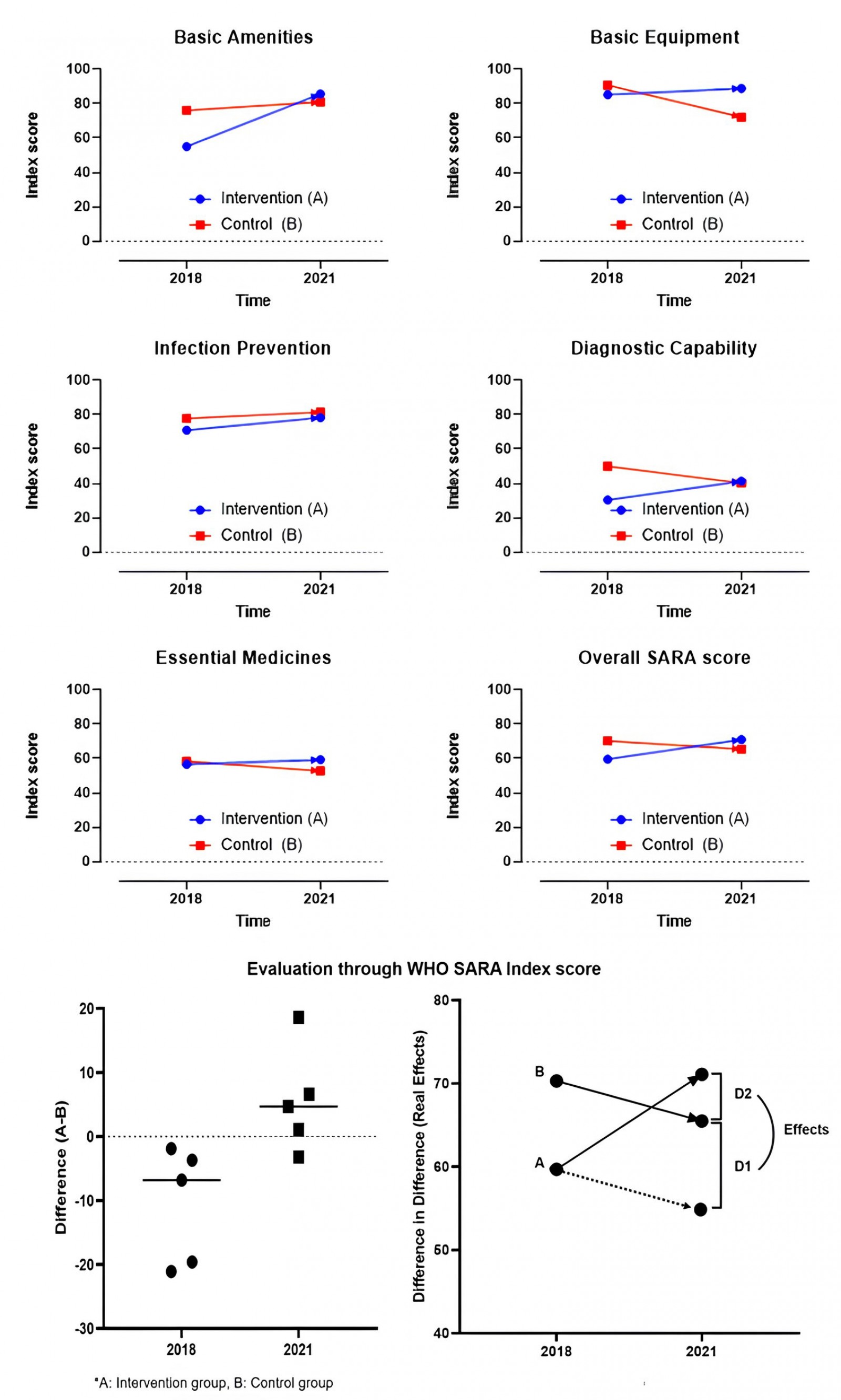 Figure 2: Service Availability and Readiness Assessment difference of intervention group to control group (2018, 2021).
Figure 2: Service Availability and Readiness Assessment difference of intervention group to control group (2018, 2021).
Discussion
This study employed the WHO SARA tool to assess the service readiness of public healthcare facilities in Paraguay for delivering PHC services. The aims were to identify areas that require improvement and provide insights to inform policies and decisions aimed at enhancing the quality and accessibility of healthcare services in the country. The evaluation results, encompassing healthcare human resources and WHO SARA scores, yielded significant implications for public healthcare centers in the research area.
WHO recognizes the significance of healthcare human resources18, as they play a crucial role in strengthening PHC by ensuring an adequate number and quality of healthcare providers and maintaining continuous healthcare delivery19. In this study, the intervention led to an increase in healthcare human resources, with the average number of doctors increasing from 0.4 per facility (total of three) in 2018 to 1.1 per facility (total of 22) in 2021, and CHWs increasing from 1.7 per facility (total of 12) to 4.7 per facility (total of 94). Insufficient healthcare human resources can impede the provision and quality of medical services, leading to disparities in healthcare access. Therefore, it is imperative to continuously strengthen and support healthcare human resources through effective policy measures.
The results of this study demonstrated an increase in healthcare human resources, including doctors, nurses, midwives, health workers, and other personnel, in public healthcare centers within the intervention area. This positive change indicates progress in securing an adequate and well-trained medical workforce to deliver high-quality healthcare services. However, it is noteworthy that Paraguay’s physician density was approximately 1.05 per 1000 people in 2020, compared to a South American average of around 2.0 per 1000 people, highlighting a shortage of physicians in the country20. To address this issue, Paraguay aims to strengthen the PHC delivery system through public healthcare and medical centers by 2030, as part of its major health strategies21. Prior to the intervention in 2018 the intervention area experienced a shortage of healthcare workers compared to other public healthcare centers. Consequently, local residents often faced challenges in accessing quality medical services due to the absence of doctors or nurses. In such instances, residents sought care at private medical centers or secondary and tertiary care facilities for basic medical treatment12. However, after the intervention in 2021 there was an increase in healthcare workers, with multiple doctors and nurses assigned to public healthcare centers in the intervention area. This development aligns with the need for a solid foundation in constructing a medical delivery system centered on public healthcare and medical centers.
The WHO also emphasizes the importance of healthcare human resources as a prerequisite for evaluating service availability and readiness22. The health workforce density in Paraguay remains a critical challenge, with 1.2 physicians per 1000 population and 2.8 nurses and midwives per 1000 population, according to 2022 national statistics23. Although there has been progress in increasing the overall health workforce density, there is significant maldistribution, with healthcare workers heavily concentrated in urban areas, leaving rural and remote regions underserved. This urban–rural disparity contributes to inequitable access to healthcare services and impacts the overall service readiness of primary healthcare facilities. Consequently, after the intervention, public healthcare centers in the research area were adequately staffed with essential healthcare professionals such as doctors, nurses, midwives, and healthcare administrators to provide high-quality medical services. The deployment of healthcare human resources, as one of the interventions, positively influenced the improvement of service availability, which likely contributed to increased utilization of public healthcare centers by residents in the research area.
The evaluation of facility availability and readiness in the research area, conducted by comparing the differences in the WHO SARA index scores before and after the intervention, revealed an overall increase in the total SARA index score within the intervention area. The overall WHO SARA score improved from 59.7 in 2018 to 71.1 in 2021, with a statistically significant DID value of 16.2 points (p=0.030), highlighting the intervention’s effectiveness in enhancing service readiness. Specifically, there were significant improvements in the scores for basic amenities, basic equipment, and diagnostic capability. The scores for infection prevention and essential medicines also increased, although the differences were not statistically significant.
The assessment of basic amenities served as an indicator for evaluating the physical environment of public healthcare facilities, and it showed that the intervention area had experienced significant improvements compared to the control area. For example, the basic amenities score increased from 55.1 in 2018 to 85.7 in 2021 (p=0.003), indicating substantial enhancements in infrastructure, including access to clean water, reliable electricity, and improved sanitation facilities. The physical environment of healthcare facilities plays a crucial role in influencing residents' decisions to seek medical care24. Factors such as access to sanitary facilities, clean water, and uninterrupted power supply are particularly important for facilities delivering primary healthcare services25. A clean and sanitary physical environment in PHC facilities contributes to increased access to safe drinking water, sanitation facilities, and disease prevention26,27.
Basic equipment is another important aspect of integrated PHC management, as it includes essential medical tools and devices such as thermometers and blood pressure monitors, which are vital for primary care28. The basic equipment score improved significantly from 85.2 in 2018 to 90.8 in 2021 (p=0.018), reflecting better access to essential diagnostic tools and medical devices. Additionally, the COVID-19 pandemic heightened the need for medical devices, and ensuring the availability of basic medical tools and equipment for delivering essential medical services has further improved access to health care29. The increases in the scores for basic equipment and diagnostic capability in the intervention area, compared to the control area, indicate the positive impact of the intervention in supporting medical devices. However, it is important to note that previous studies have cautioned about potential issues arising from a lack of follow-up management after the provision of medical devices. Therefore, continuous monitoring and maintenance are necessary to ensure the functionality of medical equipment, drawing lessons from the findings of previous research30.
Despite the efforts to strengthen PHC, the intervention did not have a significant effect on the items of infection prevention and essential medicines. Although there was an increase in the scores of these items in 2021 compared to 2018, the increase was not substantial and did not reach statistical significance. This result can be attributed to several factors. First, the occurrence of the COVID-19 pandemic between 2018 and 2021 had a significant impact. Paraguay was recognized as one of the countries in Latin America that effectively implemented COVID-19 quarantine measures by establishing a government-led regional medical delivery system31. The Paraguayan government initially invested in essential medical supplies in PHC facilities to respond to the pandemic32. As a result, both the intervention and control areas may have seen improvements in infection prevention and essential medicine scores due to the government's response to COVID-19. Second, there was a notable increase in confirmed cases of dengue fever from 2018 to 2021, which also had a significant impact. PHC facilities play a crucial role in the prevention of infectious diseases and health promotion, and the Paraguayan government implemented policies centered on primary healthcare centers to address the dengue fever outbreak33. These government policies may have influenced the results of the study. Furthermore, logistical challenges such as inconsistent supply chains and inadequate infection control training may have limited the intervention's effectiveness in these areas. It is important to note that a more accurate evaluation of the availability and readiness of PHC services using the WHO SARA index would require assessing the situation within 2 years after the completion of the intervention.
The analysis of the overall WHO SARA index scores using the DID approach showed that the intervention area scored 10.6 points less than the control area in 2018, but 5.6 points more in 2021, resulting in a net DID effect of 16.2 points (p=0.030). These findings emphasize the importance of government policies aimed at improving the quality and accessibility of healthcare services, with public healthcare centers playing a central role in Paraguay's medical system policy. The study's results indicate that the preparation for providing medical services in the intervention area was effectively carried out, leading to a positive impact on facility readiness. However, challenges such as workforce maldistribution, inconsistent supply chains, and limited infection control capacity remain critical barriers to achieving sustainable improvements in service readiness. Now that a conducive policy environment has been created, it is crucial to consider how public health and medical centers can be integrated into a unified system. Previous studies have shown that, even with well-planned infrastructure, operational challenges can arise, necessitating the exploration of alternative approaches. To avoid potential failures, policy efforts should involve local communities, fostering their active participation. For example, the ‘social prescribing’ program, which is being studied by WHO and many countries such as the UK, Canada, Australia, and South Korea, can be a successful alternative34. Social prescribing began with the theory that social determinants of health affect health; it is a concept that can create participatory PHC by utilizing community resources35,36. Integrating such community-driven approaches can strengthen the sustainability of healthcare interventions, ensuring that public health facilities become integral parts of the communities they serve. In this way, if a public health and medical center serves as a ‘setting’ to host various community events and provide medical services, it will become a facility that is essential to the community, not just a facility that provides medical services.
Limitations
Despite the valuable insights provided by this study, several limitations should be acknowledged. First, the study's quasi-experimental design with pre- and post-intervention assessments limits the ability to establish definitive causal relationships, as external factors such as national health policies and the COVID-19 pandemic may have influenced the outcomes. The pandemic, in particular, introduced confounding variables, including emergency health interventions and resource reallocations, which could have impacted service readiness independently of the intervention. Second, the evaluation relied heavily on the WHO SARA tool, which, while comprehensive, may not fully capture qualitative aspects of healthcare delivery such as patient satisfaction, service quality, or cultural barriers to healthcare access. Third, the data collection was limited to two time points (2018 and 2021), restricting the ability to analyze long-term trends or sustainability of the intervention’s effects. Additionally, the potential for information bias exists, as data collection relied on facility-reported information and onsite assessments, which may be subject to reporting inaccuracies or observer bias. Finally, the study focused on a specific region in Paraguay, limiting the generalizability of the findings to other regions with different healthcare infrastructure, population demographics, or resource availability. Future research should consider longitudinal designs with multiple follow-up periods, include qualitative assessments, and expand the study scope to enhance the robustness and applicability of the findings.
Conclusion
This study aimed to evaluate the service readiness of PHC facilities in a rural area of Paraguay using the WHO SARA tool. The results demonstrated significant improvements in key domains such as basic amenities, basic equipment, and diagnostic capability, with the overall SARA score increasing from 59.7 in 2018 to 71.1 in 2021 (DID = 16.2, p=0.030). These findings confirm that targeted interventions, including infrastructure development and healthcare workforce expansion, can effectively enhance PHC service readiness.
However, the lack of significant improvement in infection prevention (p=0.745) and essential medicines (p=0.483) highlights the need for integrated policies that address supply chain management and infection control practices. This suggests that merely implementing health policies is not sufficient; it is essential to strengthen the local healthcare system’s capacity to adopt these policies effectively, address regional health inequalities, and improve basic health infrastructure to achieve universal health coverage.
What distinguishes this study from previous research is its focus on measuring the direct impact of health system interventions using quantitative WHO SARA data in an upper middle-income country context. By applying the DID approach, this study provides new evidence on how service readiness can be significantly improved through targeted interventions, offering practical insights for policymakers aiming to strengthen PHC systems. The findings support the development of integrated healthcare policies that collaborate with local communities, ensuring sustainable improvements in healthcare accessibility and service delivery.
Funding
This work was supported by the Korea International Cooperation Agency under the title of ‘Formation & consolidation of MICRORED in Limpio Municipality, Central Department, Paraguay’ in 2016–2022 (no. P2016-00135-2).
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education (2022R1A6A3A01087288).
Conflicts of interest
The authors have no conflicts of interest to declare.
References
You might also be interested in:
2016 - Rural health service planning: the need for a comprehensive approach to costing
2006 - Essential tips for measuring levels of consumer satisfaction with rural health service quality


