Introduction
Each day, approximately 800 pregnant women die globally, with a predominant burden observed in low- and middle-income countries1. The leading causes include severe hemorrhage, infections, and preeclampsia, which substantially impair maternal health2. Fortunately, many of these threats are preventable or manageable. Timely identification of both individual and population-level risk factors, including consistent health care throughout pregnancy and access to essential services that promote wellbeing, can make a significant difference3,4. The profound societal, community, and familial repercussions of maternal mortality underscore its significance5, which has led to its inclusion as one of the Sustainable Development Goals6.
Maternal mortality does not operate in isolation. It is intricately tied to the distribution of resources and overall population health outcomes7. This perspective highlights that the incidence of such adverse events is rooted in the dynamics of the environments in which people live and the interactions that occur within them. Within public health discourse, this outlook aligns with the exploration of social inequalities in health8.
These health disparities epitomize systematic health outcome variations across social strata9. Grounded in differential exposures, susceptibilities, and vulnerabilities, these disparities evolve within a stratification framework, accumulating across the life course10. They are shaped by intersecting political, social, and economic forces10,11.
A range of markers – educational attainment, income, gender, to name a few – delineate social stratification. Among these, place of residence holds particular significance8. It accentuates the sharp divides between urban and rural areas, marked by differential exposures and vulnerabilities that influence maternal mortality rates12-14.
In Colombia, there has been a concerning increase in maternal mortality since 201315. Hypertensive disorders have emerged as leading causes, followed by hemorrhage, sepsis, and thromboembolic events. Regions with a higher prevalence of unsatisfied basic needs have demonstrated higher maternal mortality rates16. These trends also vary among pregnant women based on their educational attainment and type of health insurance coverage17. Compounding these challenges, the COVID-19 pandemic exacerbated maternal mortality nationwide, with municipalities experiencing greater deprivation bearing a heavier burden18.
Adopting a longitudinal perspective in analyzing social inequalities provides invaluable insights, enabling a nuanced understanding of changes and patterns in maternal mortality trends8. Globally, there is a call for nations to implement targeted strategies aimed at reducing maternal mortality19. In this context, developing a comprehensive understanding of the multifactorial factors influencing maternal mortality is essential for informed public health policymaking20. Consequently, this study aims to examine the intricacies of social inequalities in maternal mortality by area of residence in Colombia from 2014 to 2021.
Methods
Type of study and data source
This study adopts an ecological, longitudinal approach leveraging retrospective data. Information was extracted from the vital statistics registers maintained by Colombia’s National Administrative Department of Statistics (DANE). These records systematically document vital events, such as births and deaths, while offering insights into their individual characteristics.
DANE classifies maternal mortality into five distinct categories: pregnancy-related fatalities, maternal deaths stemming from obstetric sequelae, mortality from coincidental causes, postpartum deaths due to external reasons, and late maternal mortality. The scope of this study was limited to the initial three categories. For analytical clarity, pregnancy-related deaths and deaths from obstetric sequelae were amalgamated into a collective subgroup dubbed ‘maternal deaths due to complications of pregnancy, childbirth, and the puerperium’ (MMEPP). This classification is rooted in the underpinning that the primary death cause is attributed to the ICD-10 codes O00–O9921. The subsequent group incorporated the subset and was further augmented with maternal deaths from coincidental causes and was referred to as total maternal deaths (MMT). This group also included deaths resulting from neoplasms (ICD codes C00–D48) and external causes (ICD-10 codes V01–Y98). Deaths occurring beyond 42 days postpartum were intentionally excluded from this analysis.
Sourcing from the identical dataset, information on live births was retrieved and mapped against the mother’s place of residence. DANE’s typology for residential classification identifies three terrains: municipal center (formerly municipal seat or class 1), settlement (previously population center or class 2), and remote rural area (formerly dispersed rural area or class 3). The municipal center is synonymous with the administrative nucleus, whereas the settlement is characterized by a minimum congregation of 20 adjacent dwellings situated outside the municipal center. The remote rural area is discernible by its agricultural affiliations, lands designated for leisure or rejuvenation, and zones marked for mining or extraction activities22.
For this study, the maternal mortality ratio (MMR) was calculated as the ratio of maternal deaths to the number of live births each year. Calculations were conducted for each subgroup, yielding an MMR for pregnancy, childbirth, and puerperium (PPD) complications and a total MMR. These MMRs were further stratified by each type of residence: remote rural area, settlement, and municipal center.
Statistical analysis
Following the formulation of the distinct MMRs, they were scrutinized to deduce trends and discern social disparities. The trajectory analysis hinged on the joinpoint regression model. Within this framework, the dependent variables were derived from each MMR subset, while the calendar year functioned as the independent variable. This trend analysis was tailored for every group, setting a significance threshold at p<0.05. Within this regression, significance evaluations employed the Monte Carlo permutation method. This facilitated the calculation of the annual percentage change (APC) and its counterpart, the average annual percentage change (AAPC). Both these metrics considered the fluctuations in the dependent variable over time and were contextualized with their accompanying 95% confidence intervals. The computational aspect was managed using the open-license Joinpoint v4.9.1.0 (US National Cancer Institute; https://surveillance.cancer.gov/joinpoint).
Building on the foundational analysis, the slope inequality index (SII) and the Kunst and Mackenbach relative inequality index (RII) were computed, leveraging weighted linear regressions. The SII was estimated by following the methodology described in the WHO HEAT Plus tool (https://www.who.int/data/inequality-monitor/assessment_toolkit). This method uses a weighted regression model to calculate the absolute difference in the indicator (MMR) between the most advantaged and most disadvantaged subgroups, considering the entire distribution of the population.
To calculate the SII:
- A weighted sample of the population is ranked from the most disadvantaged (rank 0) to the most advantaged subgroup (rank 1) based on area of residence.
- The midpoint of the cumulative population distribution within each subgroup is used as the independent variable.
- The MMR is regressed against this midpoint value using a generalized linear model with a logit link.
- The predicted values of MMR are calculated for rank 0 (v0) and rank 1 (v1).
-
For adverse indicators such as maternal mortality, the SII is calculated as:
where a positive SII indicates higher mortality in the most disadvantaged group (eg remote rural areas), and a negative SII indicates higher mortality in the most advantaged group.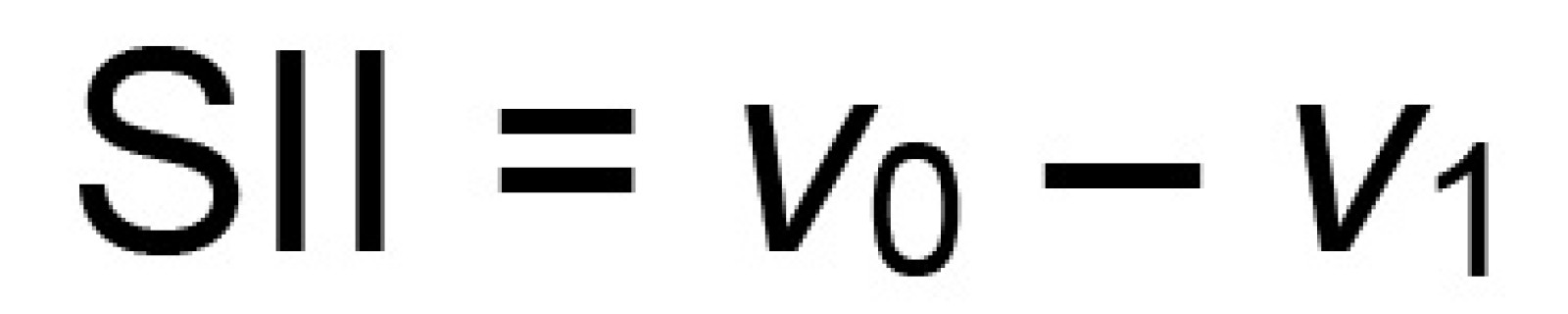
The RII was calculated to measure relative inequality, defined as the SII divided by the mean MMR in the population, reflecting the relative difference between the highest and lowest ranked groups in proportion to the mean:
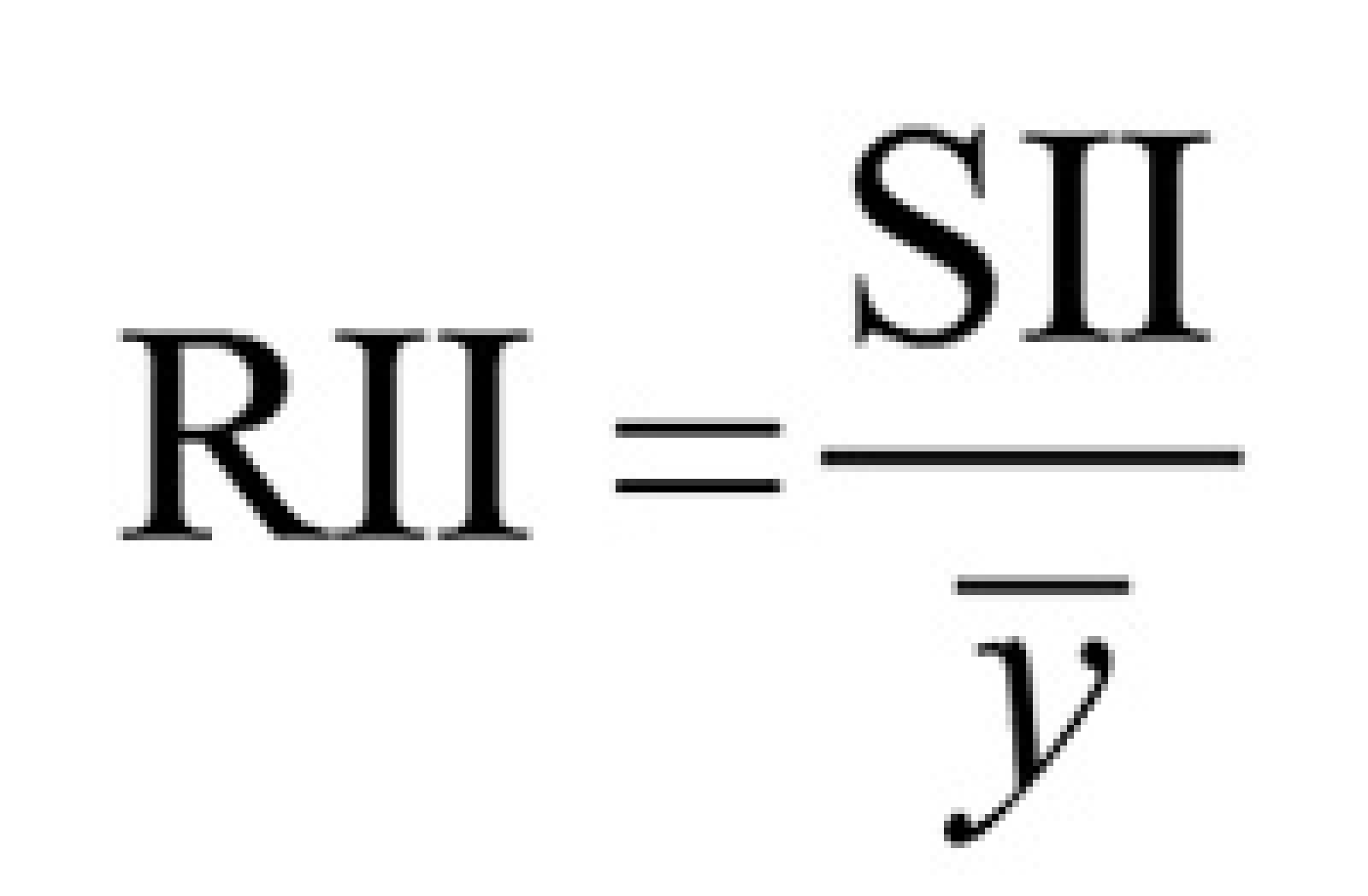 where ȳ is the mean MMR in the entire population.
where ȳ is the mean MMR in the entire population.
This analytical phase was pivotal in estimating both absolute and relative disparities between clusters defined by their socioeconomic positioning – herein, the area of residence. Adopting these measures is deemed apt when the groups in focus are naturally ordered23. The computational execution for these metrics was achieved using the Health Disparities Calculator v2.0.0 (US National Cancer Institute; https://seer.cancer.gov/hdcalc).
Ethics approval
The research was evaluated by the Health Research Ethics Committee of the San Martín University Foundation and received its approval in Act 002 of January 2023. In addition, this research utilizes secondary data that are publicly available. The information on the DANE platform is anonymized, making it impossible to trace the identities of the deceased women. As per Colombian legislation, this type of study is categorized as a no-risk investigation24.
Results
Maternal mortality ratio
During the study period, a total of 3,260 maternal deaths (MMT) and 2,885 maternal deaths due to complications of pregnancy, childbirth, and puerperium (MMEPP) were recorded. Of these, 68.6% occurred in municipal centers, 23.3% in remote rural areas, and 8.1% in settlements. The year 2021 recorded the highest number of maternal deaths, with 541 MMTs. The MMR for that year was 83.7 per 100,000 live births in municipal centers, 67.9 per 100,000 in settlements, and 120.6 per 100,000 in remote rural areas. Figures 1 and 2 illustrate the MMR trends across the study years. Notably, in 2018, municipal centers recorded their lowest MMEPP at 37.1 per 100,000 live births, while other regions consistently reported rates exceeding 62 per 100,000 live births. Throughout the study period, both MMT and MMEPP were highest in remote rural areas, except in 2015, when settlements recorded the highest rate at 92.8 per 100,000 live births.
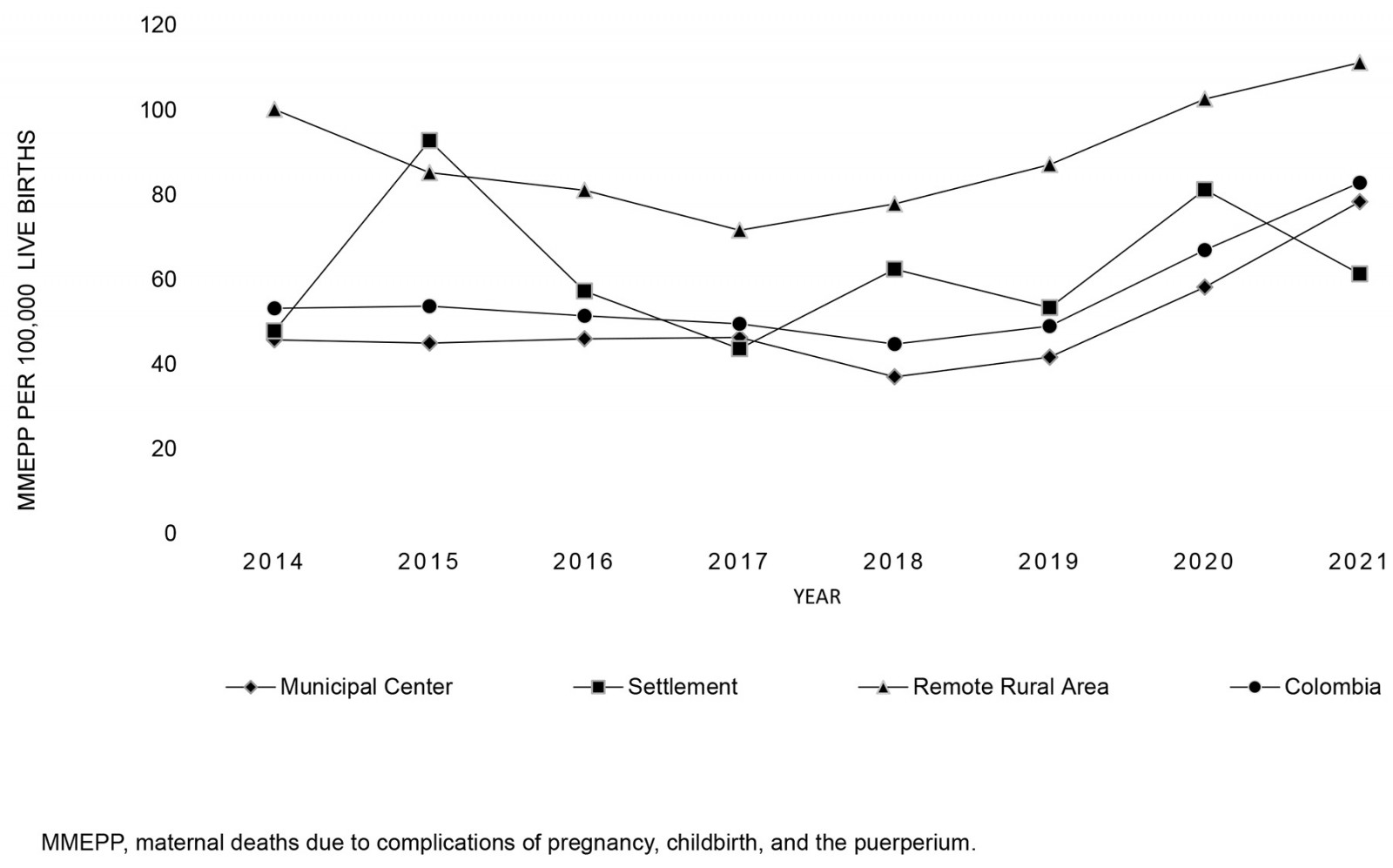 Figure 1: Maternal mortality ratio due to direct obstetric causes (pregnancy, childbirth, and puerperium) in Colombia and by area of residence, 2014–2021.
Figure 1: Maternal mortality ratio due to direct obstetric causes (pregnancy, childbirth, and puerperium) in Colombia and by area of residence, 2014–2021.
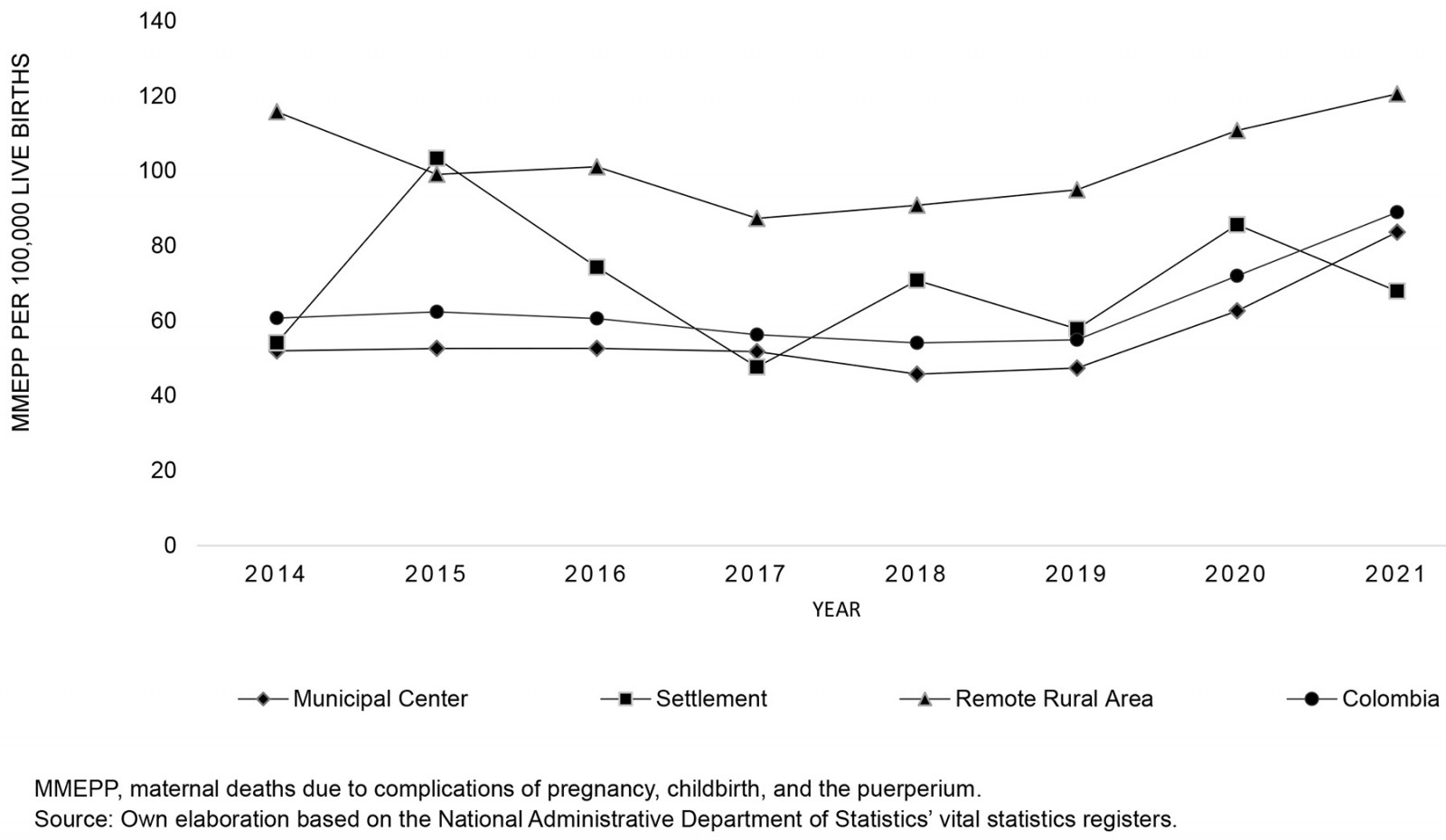 Figure 2: Total maternal mortality ratio (direct and indirect causes, and indirect obstetric deaths) in Colombia and by area of residence, 2014–2021.
Figure 2: Total maternal mortality ratio (direct and indirect causes, and indirect obstetric deaths) in Colombia and by area of residence, 2014–2021.
Trends in maternal mortality: maternal mortality related to pregnancy, childbirth, and puerperium
Table 1 presents maternal mortality trends by area of residence, showing that both the municipal center and remote rural area groups exhibited an inflection point, resulting in two distinct segments for each. For the municipal center, the APC during 2014–2019 was –2.6 (95% confidence interval (CI)= –10.3–5.9), increasing sharply to 38.8 (95%CI=1.7–89.4) from 2019 onwards. In the remote rural areas, the APC was –10.6 (95%CI= –17.2– –3.4) during 2014–2017 and 12.2 (95%CI=7.3–17.4) during 2017–2021. No inflection point was identified for the settlement group. The AAPC was 7.8 (95%CI=0.9–15.1) for the municipal center, while the settlement and remote rural areas had AAPCs of 0.2 (95%CI= –10.0–11.5) and 1.8 (95%CI= –0.8–4.5), respectively.
Table 2 details maternal mortality trends by area of residence, showing that both the municipal center and remote rural area groups displayed two trend segments. For the municipal center, the first segment spanned 2014–2019 with an APC of –2.5 (95%CI= –7.1–2.3), followed by a sharp increase to 32.9 (95%CI=10.2–60.4) from 2019 onwards. In the remote rural areas, the periods were 2014–2018 with an APC of –6.1 (95%CI= –12.2–0.4) and 2018–2021 with an APC of 11.9 (95%CI=1.4–23.4). Notably, no significant inflection point was identified for the settlement group. The AAPC for the municipal center, settlement, and remote rural area was 6.6 (95%CI=2.5–10.8), –0.9 (95%CI= –10.7–9.9), and 1.2 (95%CI= –2.3–4.8), respectively.
Table 1: Estimated inflection points for maternal mortality due to causes related to pregnancy, childbirth and puerperium, Colombia 2014–2021
| Residential area | Years | APC/AAPC | 95%CI | p |
|---|---|---|---|---|
| Municipal center | 2014–2019 | –2.55 | –10.32–5.89 | 0.395 |
|
2019–2021 |
38.76 | 1.67–89.37 | 0.044* | |
|
2014–2021 |
7.80† | 0.94–15.13 | 0.030* | |
| Settlement | 2014–2021 | 0.17† | –10.01–11.51 | 0.970 |
| Remote rural area | 2014–2017 | –10.57 | –17.18– –3.43 | 0.019* |
|
2017–2021 |
12.21 | 7.26–17.38 | 0.004* | |
|
2014–2021 |
1.81† | –0.78–4.46 | 0.170 |
*p<0.05, **p<0.01, ***p<0.001.
† AAPC.
AAPC, average annual percentage change. APC, annual percentage change. CI, confidence interval.
Table 2: Estimated inflection points for total maternal mortality, Colombia 2014–2021
| Residential area | Years | APC/AAPC | 95%CI | p |
|---|---|---|---|---|
| Municipal center | 2014–2019 | –2.49 | –7.05–2.30 | 0.190 |
|
2019–2021 |
32.96 | 10.20–60.43 | 0.020 | |
|
2014–2021 |
6.50† | 2.45–10.81 | <0.010* | |
| Settlement | 2014–2021 | –0.94† | –10.69–9.87 | 0.830 |
| Remote rural area | 2014–2018 | –6.14 | –12.22–0.36 | 0.060 |
|
2018–2021 |
11.85 | 1.37–23.41 | 0.040* | |
|
2014–2021 |
1.19† | –2.30–4.80 | 0.510 |
*p<0.05, **p<0.01, ***p<0.001.
† AAPC.
AAPC, average annual percentage change. APC, annual percentage change. CI, confidence interval.
Inequalities in maternal mortality
Throughout the study period, both types of maternal mortality consistently displayed negative values in the SII. In absolute terms, the disparity in remote rural areas ranged from 47 to 94 total maternal deaths and from 34 to 84 deaths due to pregnancy, childbirth, and the puerperium. Relatively, women in remote rural areas faced a 41–88% higher risk of maternal death than those in municipal centers, a pattern that was consistent across all mortality types. Notably, 2021 showed the smallest relative inequality, while 2017 recorded the lowest absolute difference between groups, a pattern consistent across both types of maternal mortality.
Table 3: The slope inequality index and relative maternal mortality inequality index, Colombia 2014–2021
| Year | Total maternal mortality | Maternal mortality due to causes related to pregnancy, childbirth and puerperium | ||
|---|---|---|---|---|
|
SII (95%CI) |
RII (95%CI) | SII (95%CI) | RII (95%CI) | |
| 2014 |
–90.78 |
1.86 (2.04–1.67) |
–77.6 (–110.76– –44.45) |
1.84 (2.05–1.64) |
| 2015 |
–94.3 (–130.15– –58.46) |
1.861 (2.04–1.7) |
–83.9 (–117.32– –50.49) |
1.88 (2.07–1.69) |
| 2016 |
–79.97 (–115.23– –44.76) |
1.79 (2.00–1.59) |
–55.33 (–86.97– –23.68) |
1.7 (1.96–1.44) |
| 2017 |
–46.87 (–78.43– –15.30) |
1.59 (1.86–1.31) |
–33.53 (–62.54– –4.52) |
1.51 (1.83–1.18) |
| 2018 |
–77.88 (–110.59– –45.17) |
1.84 (2.04–1.64) |
–72.04 (–102.30– –41.77) |
1.891 (2.09–1.69) |
| 2019 |
–73.87 (–107.42– –40.33) |
1.804 (2.02–1.59) |
–71.45 (–103.53– –39.37) |
1.843 (2.05–1.63) |
| 2020 |
–82.39 (–118.63– –46.15) |
1.73 (1.93–1.53) |
–76.92 (–111.89– –41.96) |
1.73 (1.94–1.52) |
| 2021 |
–48.85 (–86.01– –11.69) |
1.43 (1.69–1.18) |
–42.09 (–77.83– –6.36) |
1.41 (1.68–1.13) |
CI, confidence interval. RII, relative inequality index. SII, slope inequality index.
Discussion
Our study aimed to examine the patterns of social disparities in maternal mortality by area of residence in Colombia from 2014 to 2021. The findings reveal that maternal mortality was consistently higher in remote rural areas than in settlements and municipal centers. Notably, MMEPP exhibited a significant increase in municipal centers during the last 3 years of observation, while in remote rural areas, this escalation has been evident since 2017. For MMT, the increase in municipal centers was observed in the final 3 years, whereas in remote rural areas, it began in 2018.
The disparities in maternal mortality rates can largely be attributed to variations in access to health services, particularly for pregnant women. Previous research underscored the challenges faced by women in rural settings, including the need to travel long distances to access prenatal and obstetric care, coupled with a shortage of skilled healthcare professionals available for maternal care25,26. Consequently, complications such as prolonged labor, excessive hemorrhage, fever with bleeding, and childbirth-related convulsions are more prevalent among women in these areas27. Postpartum care, a critical component of maternal health, also reveals stark disparities; the most recent National Demographic and Health Survey of Colombia (2015) indicates that only 64.4% of rural women accessed postnatal consultations27.
Our study’s outcomes align closely with findings from the Technical Surveillance Report by the National Institute of Health of Colombia17, which reported disparities ranging from 50% to 90%. While Latin America lacks directly comparable studies, existing research has primarily focused on economic disparities among municipalities or provinces18,28,29. In high-income countries, it is well established that rural women face maternal mortality rates nearly twice as high as those of their urban counterparts14,30.
Additionally, our study highlights a concerning trend of rising maternal mortality rates even before the onset of the COVID-19 pandemic19,31. Globally, the most recent report on maternal mortality trends underscores stagnation in reducing maternal mortality during the Sustainable Development Goals era (2016–2020), with Latin America and the Caribbean being the only regions that did not experience a decline in maternal mortality during this period1.
While the underlying causes of this increase remain unclear, one plausible hypothesis points to improvements in public health surveillance. For instance, the US reported a significant increase in maternal mortality rates, which was partially attributed to enhanced surveillance and coding changes32, while Canada experienced a similar trend following the adoption of ICD-1033.
There is no doubt that the COVID-19 pandemic exacerbated maternal mortality rates, a trend observed not only in Colombia18 but globally34-36. The pandemic has highlighted systemic deficiencies in the early detection and effective management of pregnancy and childbirth complications, probably exacerbated by the overwhelming burden the pandemic placed on health systems worldwide34.
Our findings emphasize the unique health challenges and disparities faced by rural populations compared to urban residents. Based on our results, it appears that neither the health system nor broader socioeconomic policies effectively address these disparities in a timely or comprehensive manner37. This gap perpetuates and amplifies health-related inequities, as reflected in maternal mortality metrics. Addressing these disparities requires a coordinated intersectoral approach: on one hand, targeted strategies are needed to improve access to high-quality health care for rural populations38, while on the other, broader policies must foster conditions conducive to holistic health and wellbeing.
Limitations and strengths
While our study provides valuable insights, it is not without limitations. Primarily, the ecological design of our analysis means that direct causal inferences between residential areas and individual maternal outcomes cannot be established. Additionally, our study encompasses all municipalities and departments without incorporating granular analyses or controls based on these territorial classifications, suggesting that outcomes may be influenced by the economic status of these regions. Lastly, our reliance on secondary data from the National Administrative Department of Statistics presents inherent challenges. However, it is important to note that this official institution has actively worked to improve data quality and accuracy since 201939.
Conclusion
Maternal mortality rates have seen a troubling rise in recent years. Remote rural areas experience significantly higher mortality than settlements and municipal centers. Holistic, cross-sectoral interventions are imperative to cultivate environments that are more supportive and conducive to maternal health.
Acknowledgements
The authors extend their gratitude to the National Administrative Department of Statistics of Colombia.
Funding
This research received funding from San Martín University (grant number PYI-2022-008). The funders had no role in study design, data collection and analysis, publication decisions, or manuscript preparation.
Conflicts of interest
The authors declare that they have no conflicts of interest related to this work.

