Introduction
International perspective on health professional shortages in rural areas
The shortage of health professionals in rural areas is a recognised and constant issue globally. Rural areas are smaller communities that are very distant from the major population centres, and the local income is based on primary production and sustainable living1. Many countries have expressed significant concerns over the rural maldistribution of physicians2. High-income countries like Australia and the USA have developed numerous approaches to address the issue. The most effective is the establishment of rural medical education programs involving engagement in rural communities and highlighting rural practice that prepares medical students for careers in rural medicine3. Globally, numerous articles have been published about the issue, yet in Papua New Guinea (PNG) the literature on this topic is scarce4.
To address the shortage of doctors in rural areas, various countries have implemented different approaches in which rural clinical education program is a vital component.
Context of the rural health system in Papua New Guinea
The largest nation in the Pacific, PNG is classified as a low–middle-income country. According to a 2021 UNICEF report, the major health issues affecting the country are infectious diseases such as tuberculosis, malaria, diarrhoea and pneumonia5.
Other health problems are a high burden of trauma, poor child and maternal health indicators and numerous challenges in addressing socioeconomic determinants of health. A severe shortage of health workers is a serious problem in the health system, aggravated by uneven distribution. Inequity in health distribution contributes to twice the mortality among rural compared to urban children under the age of five6. Malnutrition contributes to about 30% of hospital deaths among children7. In July 2023, the PNG population was estimated to be more than 10 million, and the number of doctors was about 5007. This is a doctor-per-population ratio of 1 per 30,000. Taking into account the estimates that about 90% of doctors work for the urban population, while 85% of the population live in rural settings, the shortage of medical care for the rural population is even worse. Current analysis has shown that, out of 89 rural districts, the majority have no permanent medical doctor presence. PNG has two medical schools that produce yearly about 70 medical graduates: 50 from the University of Papua New Guinea and 20 from Divine Word University. Currently, due to limited funding, both medical schools are capable of a limited increase in the number of medical graduates.
In PNG more than 50% of rural primary health care is delivered by church health services8. Church health facilities receive most of the operational funds and supplies from the PNG government. A limited number of rural hospitals with the presence of doctors and accommodation facilities for students make rural clinical placement of students challenging.
In PNG, the Divine Word University Bachelor of Medicine and Bachelor of Surgery (MBBS) program has introduced rural clinical placement blocks for each medical student in the fourth year of study. This is a 5-year program with basic and premedical sciences and clinical skills in the first 2 years, followed by 3 clinical years. In the early years, the basic and premedical sciences are integrated with clinical sciences tailored to the students’ level. The 6-week rural clinical block takes place in the second semester of year 4. It aims to give the students first-hand exposure to rural medical training.
After completing the rural placement students should meet the following learning outcomes:
- Discuss differential diagnosis for common clinical presentations.
- Plan and implement management for common diseases at the primary level.
- Conduct health education and promotion to the community.
- Prepare and accomplish a mini project aiming at improving community health.
- Discuss the health needs of the rural population.
The faculty expected that the rural placement would give the students ample opportunity to attend to hands-on patients while working in a team, refine their clinical skills, enhance their confidence, practise health promotion skills, learn the settings in the primary health facilities and develop a better understanding of the health needs of the rural population.
Knowledge gap for factors associated with rural preference
In the literature, various factors were associated with preference to work rurally.
A scoping review of studies conducted in Asia-Pacific low–middle-income countries indicated various factors associated with the preference to work in rural locations9. These were grouped as educational, regulatory, financial incentive, professional and personal support, and factors related to the health system context. The review revealed that most studies (15) demonstrated an association between the rural background of students and their preference to work in rural areas. Further, the authors reported several studies indicating that a combination of rural origin, scholarship and a rural-oriented curriculum were correlated with actual work in rural areas9. Exploration of various educational strategies, such as the rural location of medical schools, rural clerkship and rural-oriented curricula, showed association with rural preference and work in rural areas9.
However, no studies have been carried out to evaluate the rural clerkship program in PNG. Therefore, this study aims to evaluate medical students’ perceptions of rural clinical placement, including their preference to work in rural locations. The objectives of this research were to:
- investigate factors that influence the perception of rural placements
- evaluate how this experience of rural placement impacts medical training
- assess how these perceptions project to future employment in the rural setting
- identify areas for improvement of the rural placement program.
Methods
We adopted a mixed-methods approach to obtain a more comprehensive answer to the research questions. To collect quantitative data, a survey was carried out using a self-delivered, semi-structured questionnaire. For the qualitative strand, we employed focus group discussion (FGD) as a data collection tool. The data collection was carried out in 2021. We included the MBBS program students who undertook the 6-week rural clinical placement in 2020 (year 5 students) and in the year 2021 (year 4 students).
Students were allocated to rural hospitals in groups of four to six students. In PNG, the rural population refers to people living in areas not designated as urban by the state. Rural hospitals selected for student placement were distant from the closest urban hospital by drives of about 1, 2 and 8 hours, respectively. The placements were in three rural district hospitals run by churches. Two were located in the coastal area and one in the highlands. Each hospital had basic sections including outpatient, adult, paediatric and obstetric wards, a small operating theatre, a small laboratory, ultrasound and a portable X-ray machine. Students were supervised by the rural doctor, and in some facilities also by resident doctors doing part residency in a rural block. Apart from the involvement in the clinical supervised work, including medical outreaches to villages, students conducted team community development projects.
For the survey, we distributed 42 questionnaires, 32 among year 4 and 10 among year 5 MBBS students. The semi-structured questionnaire comprised both closed- and open-ended questions. After each section of opinions, the participants were asked for additional comments. The semi-structured questionnaire employed a Likert scale to grade students’ perceptions of different aspects of the rural placement. We used a five-point scale: strongly disagree (1), disagree (2), neutral (3), agree (4), strongly agree (5).
For the quantitative data, we performed descriptive analysis using the Statistical Package for the Social Sciences v14.0 for Windows (IBM Corp; https://www.ibm.com/products/spss-statistics). The responses to the open-ended questions were analysed thematically with the qualitative data.
There were four FGDs based on the rural placement location for the qualitative part, with three to six participants per group. A total of 18 participants, 10 females and 8 males, participated in FGDs. All the sessions had a moderator (interviewer) and a co-moderator. All FGDs were carried out within a 1-hour limit. The co-moderator assisted with identifying the discussion's dynamic and taking notes of participants' views. The interview protocol framework focused on the study objectives.
Data were audio-recorded and then transcribed verbatim. We employed hybrid thematic analysis using both emergent (inductive) coding and framework coding methods (deductive; Fig 1).
An interview guide was adopted, underpinned by research objectives and socioecological theory. It provided a comparison framework while permitting the key informants to ask questions. To improve research validity and reliability, the data collection drew on three primary sources to triangulate data: surveys, FGDs and document reviews. The reviewed documents included the Rural Supervisor Guide and Rural Trainees Guide.
Figure 1 depicts how the themes were generated along the preconstructed framework.
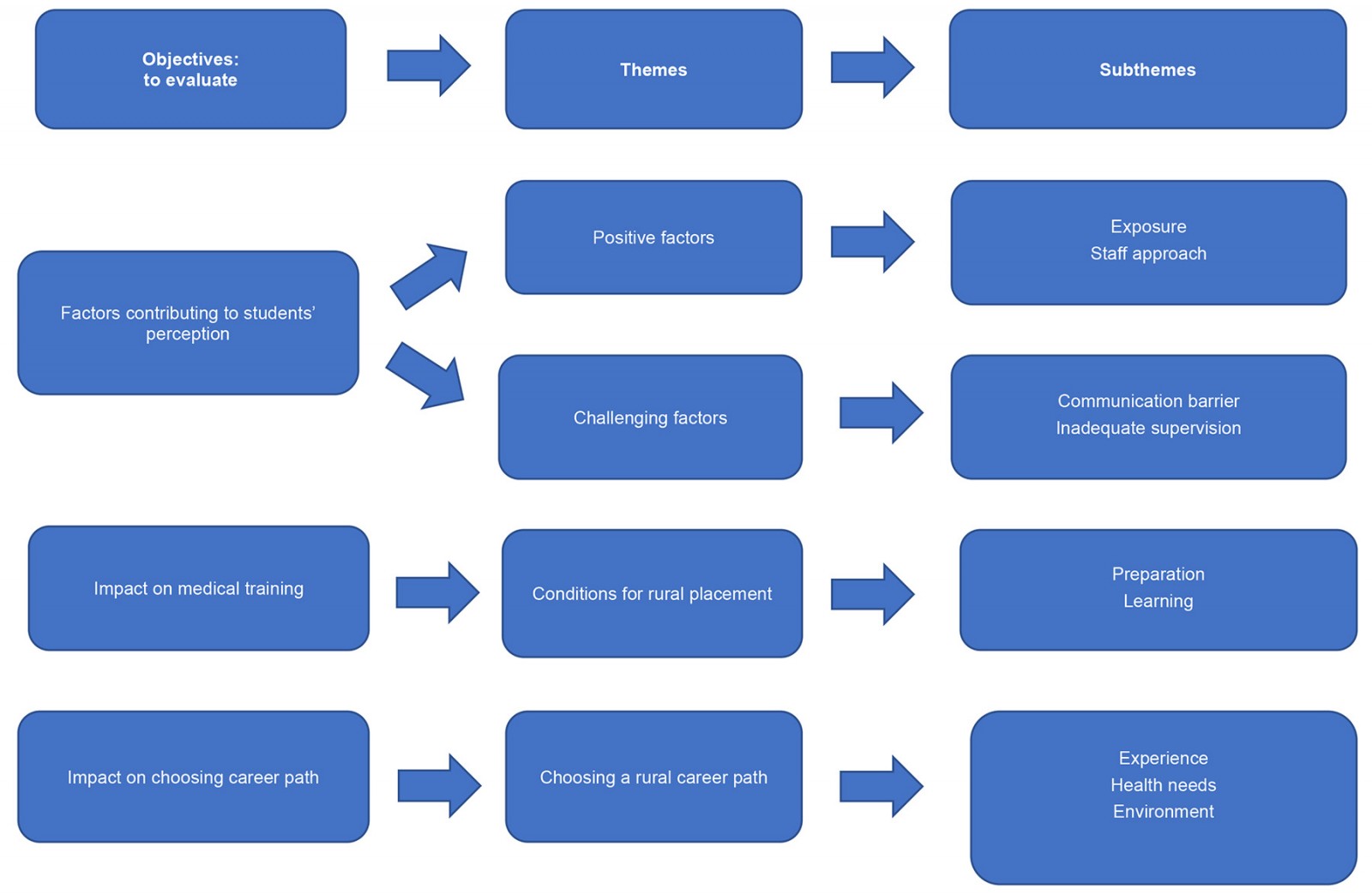 Figure 1: Relationship between the main objectives, themes and subthemes to explore medical students' perceptions of rural clinical placement in Papua New Guinea.
Figure 1: Relationship between the main objectives, themes and subthemes to explore medical students' perceptions of rural clinical placement in Papua New Guinea.
Ethics approval
The study received ethical clearance from the Faculty of Medicine and Health Sciences Research Committee at Divine Word University (approval number FRC/MHS/58-21).
Informed consent was obtained from all participants of the study.
Results
Quantitative strand
The survey response rate was 98% (41/42). The participants comprised 31 year 4 students and 10 year 5 students. The demographic characteristics of the survey participants (Table 1) showed that students’ backgrounds were evenly distributed between urban and rural areas.
The rural placement experience was generally evaluated highly by medical students (Table 2). Our findings showed that 76% of students (n=31) were satisfied (agreed or strongly agreed) with rural placement, 21% (n=9) had no strong opinion, and only one student (3%) had a negative experience. The highest score was assigned to rural clinical supervisors, highlighting attributes such as being respectful, approachable, enthusiastic and a good role model for the students. The level of supervision on patient management by the students (score of approximately 4) would need further discussion by the faculty seeking improvement in that aspect. Regarding the learning environment, the student’s perception was generally positive (4.4), indicating a need for improvement in learning resources. In terms of clinical training, rural placement was considered helpful in learning clinical skills, clerking and communication skills, and preparing for the clinical exams. It was underlined that the rural placement increased the understanding of rural health needs among medical students.
While the general perception of the rural clinical placement by the students was very positive, with suggestions to increase the duration, the majority agreed that the program needs improvement (93%, 38/42).
Table 1: Demographic characteristics of participants in survey to explore medical students' perceptions of rural clinical placement in Papua New Guinea
|
Characteristic |
n |
|
|---|---|---|
|
Gender |
||
|
Female |
22 |
|
|
Male |
19 |
|
|
Marital status |
||
|
Single |
33 |
|
|
Married |
8 |
|
|
Background |
||
|
Rural |
20 |
|
|
Urban |
21 |
|
|
Rural hospital |
||
|
R1 |
15 |
|
|
R2 |
22 |
|
|
R3 |
4 |
|
Table 2: Medical students’ perceptions of rural clinical placement exposure in Papua New Guinea
| Category | Specific aspect of rural clinical placement | Average Likert score† |
|---|---|---|
| Clinical exposure experience | ||
| Understanding rural health needs | 4.6 | |
| Communication skills | 4.3 | |
| Clerking skills | 4.2 | |
| Teamwork skills | 4.2 | |
| Learned primary care | 4.2 | |
| Help in clinical examination preparation | 4.2 | |
| Help in written exam preparation | 4.2 | |
| Relating theory to clinical skills | 4.0 | |
| Most procedures performed | 3.9 | |
| Bedside case presentations | 3.7 | |
| Total average | 4.1¶ | |
| Learning environment | ||
| Proper accommodation | 4.9 | |
| Conducive learning environment | 4.6 | |
| Access patients with wide range of illnesses | 4.5 | |
| Active participation in patient care | 4.4 | |
| Seen enough patients | 4.4 | |
| Conducive training facilities | 4.3 | |
| Suitable resources for learning | 4.0 | |
| Total average | 4.4§ | |
| Clinical supervision | ||
| Respectful supervisors | 4.7 | |
| Approachable supervisor | 4.6 | |
| Learning environment facilitated | 4.6 | |
| Enthusiastic supervisors | 4.6 | |
| Assistance in identifying learning needs | 4.5 | |
| Sufficient autonomy | 4.5 | |
| Continuity of patient care provision | 4.5 | |
| Excellent role models | 4.5 | |
| Adequate help and advice | 4.4 | |
| Useful feedback | 4.4 | |
| Appropriate clinical responsibilities provision | 4.4 | |
| Overall clinical education provision | 4.4 | |
| Decision-making in patient management | 4.3 | |
| Supervision of clinical decisions | 4.2 | |
| Total average | 4.5‡ | |
† Based on a five-point Likert scale: strongly disagree (1), disagree (2), neutral (3), agree (4), strongly agree (5).
¶ For clinical exposure experience questions, an average of 3% disagreed (2) and 21% were neutral (3).
§ For learning environment questions, an average of 2% disagreed (2) and 10% were neutral (3).
‡ For clinical supervision questions, an average of 1% disagreed (2) and 6% were neutral (3).
Qualitative strand
Throughout the discussions, there was a sense of first-time exposure to the rural area with the same expression of enjoyment in all groups. However, a comparison of the four groups indicated differences in the quality of supervision and the basic equipment in different rural facilities, which likely influenced their perception of the rural placement.
Positive factors influencing students’ perceptions of rural placements
The positive factors influencing students’ perceptions about rural placement were the exposure and positive staff approach. Students expressed that rural placement is all about the exposure to rural areas and how it shapes their clinical training, especially in a low-resource setting. One of the participants stated:
I think rural placement is good for us students because it helps us put what we've learned in theory to practice. And, also, we get to do a lot of hands-on because, in rural hospitals, there are not plenty of workers.
Participants also expressed that the staff at rural hospitals was helpful and very approachable:
The staff … were very friendly and they were eager to teach us … I think that’s the only way I learn a lot.
Challenging factors that influence the perceptions of rural placement
The challenging factors influencing students’ perceptions were communication barriers, inadequate supervisor guidance and poor diagnostic equipment.
Inadequate supervision affected training:
Sometimes the nurses approached us and asked us to do something. Some tasks we were able to do, but others we needed someone to guide us.
The students expressed the need for a faculty clinical tutor or supervisor during the rural placement. Students indicated language barriers, with a low understanding of patients and some staff interactions.
Another challenge was the diagnostic process caused by the lack of elementary diagnostic equipment in rural hospitals. Most rural hospitals do not have basic diagnostic equipment for X-ray, ECG or ultrasound:
In class, we learnt the investigations and tests that you would do to find a diagnosis; out there, in the rural [areas], there is not much of this equipment to use. Sometimes, you will have to improvise, and many of the diagnoses that you will do will rely on your clinical knowledge.
Preference for a rural career path
Many students indicated they would consider choosing a rural path based on experience, environmental factors and background.
Furthermore, the students commented that they would go to the rural path only when they had enough experience and the acquired skills. They would not go there after graduation because rural hospitals lack proper diagnostic equipment, which requires a rural doctor with in-depth clinical skills and knowledge. Another participant expressed that ‘maybe after residency … when I go through all the blocks and acquire all the knowledge and skills, then I can go’ to work in rural.
In relation to environmental factors, more females than males wanted to go to the rural areas because they were so peaceful and welcoming, and because life was cheap. A female student said:
For me, yes, I want to live in the rural area because life is cheaper, peaceful, and quiet compared to town, where it's noisy. I love the rural environment, plus the people there are very friendly.
It was noticed that students from rural backgrounds wanted to return to rural areas because of the struggles they observed in their rural communities.
Students from urban areas expressed awakening and agreed that rural placement changed their minds. They wanted to go to the rural areas because they saw the needs of the rural people:
Before, I hadn’t really experienced that scene because I grew up in town and most of my life was in the town area. In town, they got their own hospital and I haven’t been to rural hospitals too and so I haven’t really noticed things happening there. Being there, I saw the things and struggles, and it changed my mind.
Another student from an urban background stated:
I choose to be in the rural area not for my own good or my family, but for the good of the people there and because there is a need, and I saw that need.
Recommendation for rural placement program improvement
The majority of students expressed the opinion that the rural placement program needs improvement in terms of better student preparation for the placement and improved supervision during the placement.
The MBBS program should prolong the duration of the rural placement for better exposure and experience, as expressed by this participant:
… if the Medical Department can prolong the period there, then the students can have more exposure.
Some participants expressed that a faculty clinical tutor should follow the students to the rural areas to supervise and guide them.
Students also suggested that the medical program should commit to the rural training program by building dormitories in the rural training hospitals.
For policymakers, the students stated that to attract doctors to rural areas the following conditions should be met: providing basic needs for doctors and their families, increasing rural doctor salaries (incentives for remoteness) and upgrading the existing rural hospital facilities to accommodate more doctors.
The students would like to see more government support for the development and upgrading of rural facilities as well as creating career development opportunities in rural medicine. They also pointed out that improving internet coverage in rural areas would alleviate their isolation from family and friends during rural placement.
Discussion
Decentralising tendency in clinical training
The current tendency in undergraduate medical education swings towards decentralisation of clinical training by moving it from training in large specialised urban hospitals towards supervised general practice10-12. Although there is growing evidence that decentralised training produces comparable or, in some areas, superior results to centralised training13, traditionalists view training outside large urban hospitals as a waste of time and far away from ‘real medicine’ in big urban hospitals14. Traditional medical curricula employing clinical clerkships in specialised urban centres emphasise short block rotations through narrow disciplines. The model of the longitudinal integrated clerkship strengthening generalist training is gathering sizable support internationally and being increasingly implemented in medical schools10-12,14. Along with adopting a decentralised model of clinical training, some medical schools emphasise community-based education by training students in primary healthcare facilities1,15.
Value of rural clinical placement in education programs
This research explored medical students' perceptions of longitudinal rural placement and showed that rural placement enhances students’ perception of confidence and competence level in clinical skills. These views were based on the opportunity to practice several procedures, hands-on diagnosing and managing patients, a wide variety of cases and taking more responsibility for patients’ care. These findings align with a study showing that students’ perceptions after rural clerkship improved regarding work demand, medical expertise and understanding of primary care service16.
Numerous studies have confirmed that rural groups showed a comparable or higher level of performance on standard exams compared to corresponding urban groups trained in centralised hospitals17,18.
Similarly, a study by Halaas et al recorded positive results of longitudinal rural placement on students, including comparable to centralised training academic results, higher clinical skills, well-developed communication skills and confidence to undertake more responsibility for patient care14. The literature suggests that students who underwent training at rural and remote sites were not disadvantaged academically, and they believed they had a more meaningful learning experience than they would expect in urban centralised hospitals17,19.
Students' experiences in Africa20 and India15 highlighted that, during generalist rural practice, students were exposed to a wider range of patients than in highly specialised units of central hospitals, which agreed with our students' perception.
Role of rural placement in choosing a career path
In our study, many students pointed out that rural placement influenced them to think about rural career paths in the future. In line with our findings, many studies have pointed out that longitudinal rural placement increases the likelihood of students practising rural medicine in the future2,13,20-27. The study by Putri et al, analysing the factors associated with working in rural Indonesia, concluded that building the rural workforce would require a multimodal strategy, including selecting students with rural backgrounds, organising rural clerkships and internships, and providing financial incentives28. Furthermore, a study in Australia on the career path of graduates has shown that rural-based training graduates were 19 times more likely to choose a rural career path compared to students whose training was based on urban specialised hospitals (p<0.001)29. However, practices in countries that achieved some success in reducing the discrepancy in doctors’ allocation between rural and urban settings implemented more complex strategies, including proven interventions. Strasser pointed out that three factors are strongly associated with attracting and retaining doctors in rural practice: a rural upbringing, positive experience from rural exposure during undergraduate training and organised post-vocational rural training22. Implementing these strategies may lead to a long-term solution for recruitment and retaining doctors in rural facilities22. In 2000, Australia was among the first countries to implement a national policy offering more extended rural programs to undergraduate medical students. This policy is one of many tactics aiming to increase the number of rural doctors30.
Challenges of rural placement
While our findings showed that most students (76%, n=31) were satisfied (agreed or strongly agreed) with rural placement, with the highest evaluation of rural supervisors, they pointed out numerous challenges and areas that need improvement, including a shortage of supervisors and a lack of diagnostic equipment. Likewise, another study in developing countries indicated that, despite positive rural experiences, students faced several challenges, such as a shortage of diagnostic equipment, medication and supervising staff2. It was postulated that moving a part of clinical training from the central university hospital requires visionary leadership from management and staff at the medical school to upscale decentralised training11. Others pointed out that placing students at rural sites is a complex logistic task that requires additional effort in preparing students, supervisors and sites and resources on the medical school site19.
Limitations
This study's limitations included a small sample size and context specificity; therefore, the results cannot be automatically generalised to other settings. However, several approaches were used to validate the results: triangulation between quantitative and qualitative data, discussion of the results and comparison to other studies.
Conclusion
This study enhances our understanding of the factors affecting medical students' opinions on rural clinical placement and how this experience is likely to influence medical students’ future career choices. Most participants find the experience interesting and helpful, which may encourage students to work in rural settings. The medical school realised that more preparation needs to be done for the rural placement to improve the students’ experience. A further study should be conducted to assess the association between rural placement and choosing a rural career path.
Effective strategies encouraging medical students to choose rural practice require multi-stage coordinated action adopted in the undergraduate medical programs by medical schools and supported by the government's rural policy. While following the rural placement, many students considered a future working in a rural area; the final decision on the rural career path also depends on suitable conditions created by the government for rural doctors.
Conflicts of interest
The authors declare no conflict of interest.
Data availability
The data that support this study are available in the article and accompanying online supplementary material. Survey dataset: 10.6084/m9.figshare.26531083



