Context
Hervey Bay is in the Fraser Coast, part of the Wide Bay region of southeast Queensland, Australia (Fig1). Hunting for Scylla serrata mud crabs, otherwise known as ‘crabbing’ is an extremely popular activity in the local river systems (Fig2). The Wide Bay region and surrounding areas are subject to regular patterned wet and dry seasons. However, La Niña typically increases the chances of above-average rainfall, with the spring–summer–autumn of 2021–2022 progressing to flooding rains1.
During this period, there was an increased presentation of critically unwell patients with necrotising fasciitis admitted to the Hervey Bay Hospital intensive care unit (ICU). All patients had environmental exposure to saltwater estuary rivers that had recently been inundated by the 2021–2022 summer floods. Four patients had a non-cholera Vibrio species cultured, and one patient had multiple organisms as the agents of infection, which correlates positively in the literature with salty water exposure2.
Necrotising fasciitis is a surgical diagnosis characterised by friability of the superficial fascia and absence of pus in infected soft tissue. Necrotising fasciitis caused by Vibrio species carries a high morbidity and mortality, and often progresses rapidly into a life-threatening soft tissue infection, multi-organ failure and fatal sepsis. Immunocompromised patients are especially at higher risk of developing this disease. Early diagnosis and emergency fasciotomy or amputation with aggressive antibiotic treatment are therefore crucial in reducing mortality in patients, which can reach as high as 25–100%2,3.
Vibrio vulnificus is part of the normal marine microbiota and is found in warm coastal waters (typically exceeding 20°C), which provides ideal growth conditions for this microorganism4 and reaches sufficient concentrations to cause clinical illness generally in the warmer months of the year2. The typical history of Vibrio species-induced necrotising fasciitis is the infection of wounds by direct invasion or contact with contaminated seawater or raw seafood such as crustaceans3.
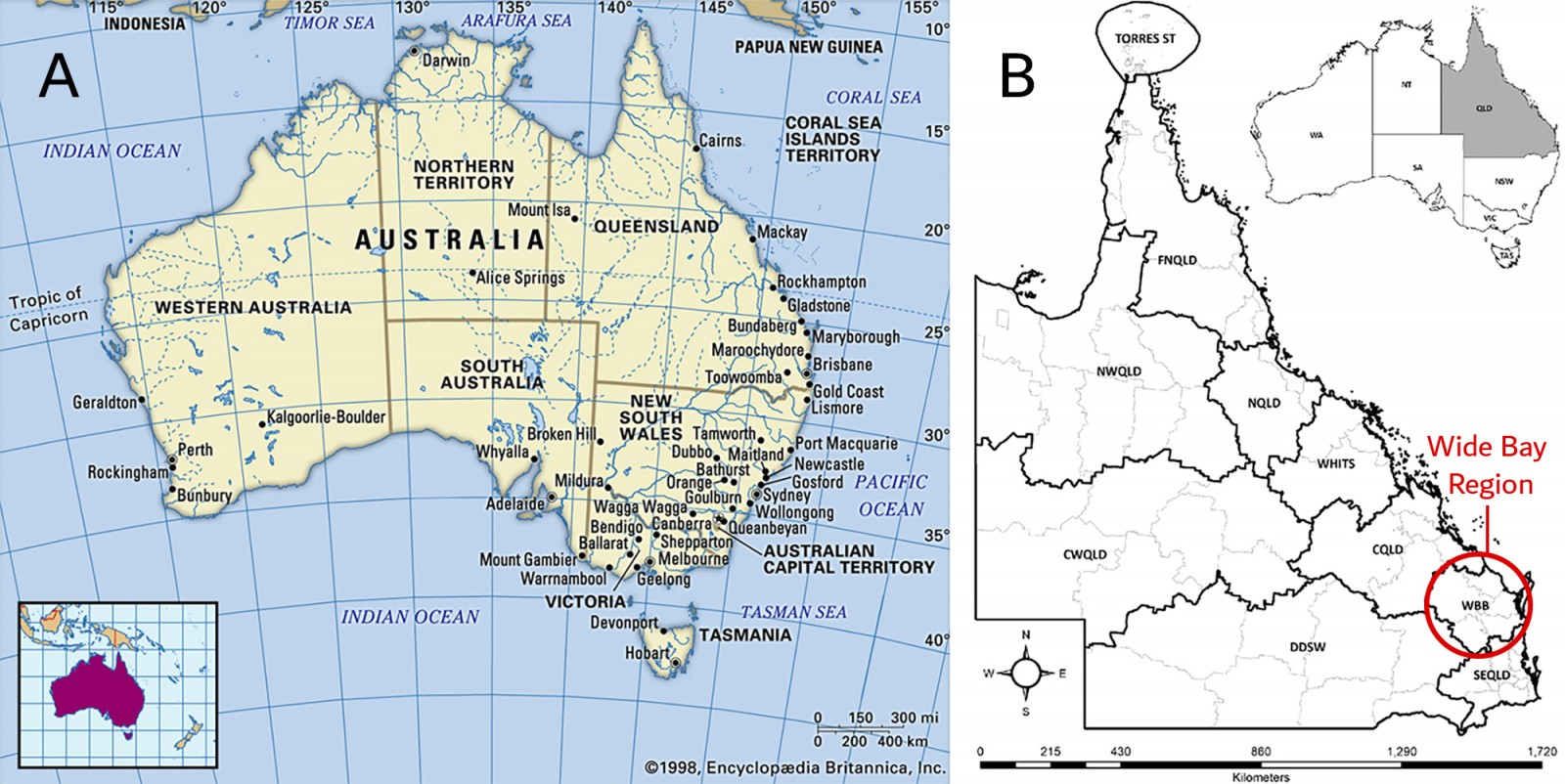 Figure 1: Maps showing the location of the Wide Bay region in Queensland, Australia. (A) Map of Australia showing detailed breakdown of regions within Queensland. Source: Regional Organisations of Council across the state of Queensland. (B) Map of Queensland showing Wide Bay and other regions. Source: Regional Organisations of Council across the state of Queensland.
Figure 1: Maps showing the location of the Wide Bay region in Queensland, Australia. (A) Map of Australia showing detailed breakdown of regions within Queensland. Source: Regional Organisations of Council across the state of Queensland. (B) Map of Queensland showing Wide Bay and other regions. Source: Regional Organisations of Council across the state of Queensland.
 Figure 2: Mary River catchment area in the Wide Bay region. Source: Mary-area-map, Mary River Catchment Coordinating Committee.
Figure 2: Mary River catchment area in the Wide Bay region. Source: Mary-area-map, Mary River Catchment Coordinating Committee.
Issue
This case series presents a review of the clinical documents for each patient with necrotising fasciitis between the months of March and October 2022.
Five male patients aged between 59 and 86 years presented with necrotising fasciitis wounds associated with injuries obtained from their hunting equipment or from crustaceans. Each exposure site was in saltwater rivers post-flooding events. All five presented to the Emergency Department in septic shock with multi-organ failure and required inotropic cardiovascular support, mechanical ventilation and aggressive antibiotic therapy. All five patients had either an emergency surgical debridement with or without an emergency fasciotomy and prolonged ICU stays. Details are displayed in Table 1.
Table 1: Patient demographics, risk factors, environment exposure and in-patient outcome.
| Attributes | Patient 1 | Patient 2 | Patient 3 | Patient 4 |
Patient 5 |
|---|---|---|---|---|---|
|
Admission date 2022 |
20 March |
22 March |
14 April |
30 May |
05 October |
|
Sex |
Male |
Male |
Male |
Male |
Male |
|
Age (years) |
79 |
82 |
59 |
86 |
81 |
|
Diagnosis |
Necrotising fasciitis, Left leg and upper foot with septic shock. |
Necrotising fasciitis to the right upper calf and lower leg and septic shock. |
Necrotising fasciitis to the left hand and forearm and septic shock. |
Necrotising fasciitis to the right lower leg. |
Soft tissue infection Rt lower leg, necrotising cellulitis, septic shock and multi-organ failure. |
|
LRINEC score |
9 |
11 |
5 |
7 |
13 |
|
APACHE II |
23 |
19 |
17 |
24 |
22 |
|
APACHE III |
75 |
74 |
36 |
72 |
103 |
|
Risk of death % |
31.10 |
23.46 |
3.98 |
22.43 |
66.11 |
|
Presenting complaint |
79yo male travelling to Hervey Bay for fishing trip, 1 day prior to admission, standing in brackish water crabbing with crab pot. Developed left foot pain gradually worsening. On presentation to hospital febrile and foot pain disproportionate to clinical signs. Subsequently became hypotensive requiring vasopressors. |
82yo male, 3 days prior to admission, scratched right leg on the crab pot, presented with fever, feeling generally unwell, poor appetite and worsening cellulitis pain, swelling and redness, hypotensive and tachycardic. |
59yo male cut his left hand lifting the crab pot out of the water 2 days prior to the presentation to ED with swollen left hand + tender on exam, no crepitation. Admitted to the ICU intubated and ventilated post debridement of necrotising fasciitis of the left forearm/hand. |
86yo male presented with 2 days history of progressive right lower leg pain and swelling, with associated fevers, hypotensive and shocked with a right leg necrotising fasciitis post-operative admission to ICU. Patient was cleaning barnacles and marine growth from the bottom of his yacht in the Mary River in knee-deep water. Nil chills/rigors. |
81yo male minor skin tear on the right shin from crab pot near Eli waters creek 4 days before presentation. PO antibiotics and minor debridement done by GP but then developed rigors, vomiting and worsening wound pain and presented to ED. On presentation, septic shock, severe pain, requiring vasopressor support. |
|
Potential source |
Crabbing/crab pot wound to left foot in the Isis River. |
Crabbing/crab pot wound to right leg in the Mary River. |
Crabbing/crab pot wound lifting the pot out of the water to his left hand/forearm in the Poona creek. |
Barnacles scratch to the lower leg in brackish water descaling his yacht in the Mary River. |
Crab pot wound on the right lower shin in Eli Creek. |
|
Organism cultured |
Vibrio parahaemolyticus (site) |
Vibrio vulnificus (BC, histopath and site) Aspergillus flavus (aspirate) Candida glabrata complex scant (site) |
Candida parapsilosis (histopath), Trichosporon Asahii (histopath and bone) Staphylococcus epidermidis (BC) Enterococcus faecalis (bone) Streptococcus pyogenes (site) |
Vibrio vulnificus (BC) |
Vibrio vulnificus (BC) |
|
Avg water temperature on day of exposure† |
26.3°C |
26.3°C |
25.4°C |
22.2°C |
22.3°C |
|
Medical background |
COPD, IHD/CABG, HTN, peripheral vascular disease CKD stage IV, IDDM |
HTN, dyslipidaemia, osteoarthritis. |
Mechanical AV replacement 2020, IHD, EF 55%, AF on warfarin, COPD, Current smoker 50 a day, HTN OSA – Intolerant of home CPAP, BMI 47, T2DM, peripheral neuropathy |
CCF LV failure EF 51%, IHD CABG 1999, CODP, AF, BPH, OA of the knee, spondylosis of the lumbosacral spine, hyperlipidaemia, GORD, gout, neuropathic pain right leg |
AF, CABG, T2DM, HTN, |
|
Radiological findings |
CT LL: Diffuse subcutaneous oedema of LL compatible with inflammation or infection with intramuscular oedema. No subcutaneous gas locules. Necrotising fasciitis cannot be ruled out. Doppler USS in ED, negative for arterial insufficiency or DVT |
X-ray left tibia/fibular ankle and foot. No gas collections are seen, diffuse soft tissue swelling at foot and calf. No focal bony lesions. Left US leg veins, No DVT identified. |
USS done ? possible collection but difficult to determine given inflammation. X-ray no fractures, gas or foreign body present. |
CT head/chest/abdomen: 1. No intracranial haemorrhage. 2. Very small volume pleural effusions and minor dependent atelectasis noted in the lungs. 3. No intra-abdominal fluid collection or definitive focal source of intra-abdominal sepsis. |
Diffuse soft tissue inflammation of the leg suggesting cellulitis with minor thickening of the fascia. No abscess formation. No extension to the intermuscular fat planes. No gas formation |
|
ICU Course |
Four days of ICU requiring mechanical ventilation, high dose vasopressor support and CRRT. Transfer to tertiary centre for ongoing care under the vascular team. |
Fifteen days of ICU with septic shock complicated with multi-organ failure including anuric renal failure requiring mechanical ventilation, vasopressor support and CRRT. Multiple blood cultures positive for Vibrio vulnificus in 1 to 2 hours. Required multiple debridements to left leg. Transferred to tertiary burns centre for further plastic surgery input. |
Six days of ICU with septic shock, requiring mechanical ventilation and vasopressors and then transferred to tertiary centre for further ICU and plastic surgery management. |
Eight days of ICU with mixed shock (septic and cardiogenic), requiring triple inotropes and vasopressors and mechanical ventilation. Blood cultures grew Vibrio vulnificus in 4.4 hour. Non oliguric renal failure not requiring dialysis. Transfer to tertiary centre for further plastic surgery management and rehabilitation. |
Seven days of ICU, presented in shock state and renal failure. Intubated for potential debridement and started on renal replacement therapy for severe lactic acidosis and refractory shock. Bedside incision of the wound by surgeons did not reveal necrotising fasciitis so was continued on medical management. Blood cultures grew Vibrio vulnificus in 4 hours, Ciprofloxacin added on day 2. Hemodynamic and metabolic abnormalities improved gradually, and he was taken off dialysis and extubated. ECHO – Likely septic cardiomyopathy in known heart failure. |
|
Surgical findings/ intervention |
Debridement dorsum of foot until viable tissue found. |
Multiple debridement ×5. Findings: multiple areas of necrotic skin wound edges left lower limb popliteal fossa and right lower limb lateral knee. |
‘Dish washer fluid’ on dorsum of left hand and index finger with necrotic tissue. Necrotising fasciitis noted to radial and posterior side of elbow. Fasciotomy done on flexor surface of forearm with minimal necrotic tissue noted. Vac dressing placed on forearm extensor surface. |
Multiple surgical debridement of extensive necrotic soft tissue right lateral lower leg from above malleolus to below knee. Approximately 1.5h procedures, with source control achieved. |
Bedside diagnostic incision that did not reveal necrotising fasciitis. Did not require debridement. |
|
Antimicrobial treatment |
Doxycycline, meropenem, vancomycin, clindamycin, ciprofloxacin and gentamycin |
Meropenem, vancomycin, clindamycin and ciprofloxacin |
Meropenem, vancomycin, clindamycin, ciprofloxacin, voriconazole and fluconazole |
Meropenem, vancomycin, clindamycin and ciprofloxacin |
Meropenem, vancomycin, clindamycin and ciprofloxacin |
|
Patient status (Three months post-ICU admission) |
Alive – in-patient in private hospital. |
Alive – in-patient rehabilitation unit. Bilateral debridement and allograft placed with STSG. Complete graft with ongoing dressing changes. |
Alive – left below elbow/hand amputation with SGST post development of osteomyelitis and multiple surgeries at tertiary unit. |
Alive – returned from tertiary hospital with multiple debridements and graft. Currently in-patient local surgical unit. |
Alive – rehabilitation at private hospital. |
†Water temperatures as recorded in Urangan boat harbour, Hervey Bay, Qld, Australia. AF, Atrial fibrillation; APACHE, Acute Physiology and Chronic Health Evaluation; AV, atrioventricular; BC, blood culture; BCC, basal cell carcinoma; BMI, body mass index; BPH, benign prostatic hypertrophy; CABG, coronary artery bypass grafting; CCF, congestive cardiac failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CPAP, continuous positive airway pressure; CRRT, Continuous Renal Replacement Therapy; CT, computed tomography; DVT, deep vein thrombosis; ECHO, echocardiogram; ED, emergency department; EF, ejection fraction; GORD, gastro-oesophageal reflux disease; GP, general practitioner; HTN, hypertension; ICU, intensive care unit; IDDM, insulin dependent diabetes mellitus; IHD, ischemic heart disease; LL, lower lobe; LRINEC, The Laboratory Risk Indicator for Necrotising Fasciitis score; Lt, left; LV, left ventricle; OA, osteoarthritis; OSA, obstructive sleep apnoea; PO, per-oral; Rt, right; STSG, split-thickness skin graft; T2DM, type 2 diabetes mellitus; USA, United States of America; USS, ultrasound scan.
 Figure 3: (A) Patient 1, upper foot on Day 5 of admission. (B) Patient 2, post debridement lateral leg on Day 2 of admission. (C) Patient 3, palmer view of hand and inner forearm, Day 5 of admission. (D) Patient 4, medial leg prior to debridement. (E) Patient 5, anterior leg prior to debridement.
Figure 3: (A) Patient 1, upper foot on Day 5 of admission. (B) Patient 2, post debridement lateral leg on Day 2 of admission. (C) Patient 3, palmer view of hand and inner forearm, Day 5 of admission. (D) Patient 4, medial leg prior to debridement. (E) Patient 5, anterior leg prior to debridement.
Data
Data obtained from Pathology Queensland show 86 Vibrio vulnificus blood cultures identified over the past 25 years (i.e. an average of 4.16 infections in Queensland per year). Although it is not known if these blood cultures were in patients presenting with necrotising fasciitis, there are several commonalities to the cases we observed. Of the 86 infections, the majority of Vibrio vulnificus infections occurred in males (91.9%) with an average age of 68.3 (±14.7) years old. We also observed a seasonal trend in the incidence of infections, with the highest number of cases occurring during summer (i.e. December to February; n=46; 53.5%) and autumn (i.e. March to May; n=30; 34.9%), which are typically the wetter seasons.
Incidence
We further investigated whether climate drivers had any influence on these infections. Our results (Fig4) showed that the rise in the number of infections coincided with La Niña, which is typically associated with increased rainfall5. The incidence rate of Vibrio vulnificus infection in Queensland was highest during La Niña events (2.9 per million population years), with an incidence rate ratio (IRR) of 4.7 (95% CI 1.3 to 6.6) when compared with the incidence rates during the neutral phase (i.e. non-La Niña nor El Niño events; 0.6 per million population years).
In contrast, during El Niño, which is typically associated with warmer temperature and less rainfall6, there were only 9 cases of infection over a period of 6.4 years, with an incidence rate of 0.3 per 1,000,000 population years at risk and an IRR of 0.5 (95% CI 0.6 to 1.3) compared with the neutral phase.
Table 2 indicates higher infection rates during La Niña are consistent with a previous study that showed the influence of climate drivers, such as El Niño, on abundance of Vibrio vulnificus in a tropical region7.
A search of the literature for Australian cases recovered a limited number of cases, with the majority of infections in tropical regions of Queensland and, importantly, in years of significant flooding rain1,8. Ralph et al documented a case series of Vibrio vulnificus and V. parahaemolyticus necrotising fasciitis infections in three fishermen in the tropical waters of the western Gulf of Carpentaria (16°S), a location that is characterised by sedimentary stratiform of lead, zinc and silver mining operations9. The water temperatures were recorded as 23–30°C. Although Vibrio is most commonly found in tropical and warm coastal waters8, the Fraser Coast area (25–26°S), is below the Tropic of Capricorn (23°S), making Fraser Coast sub-tropical.
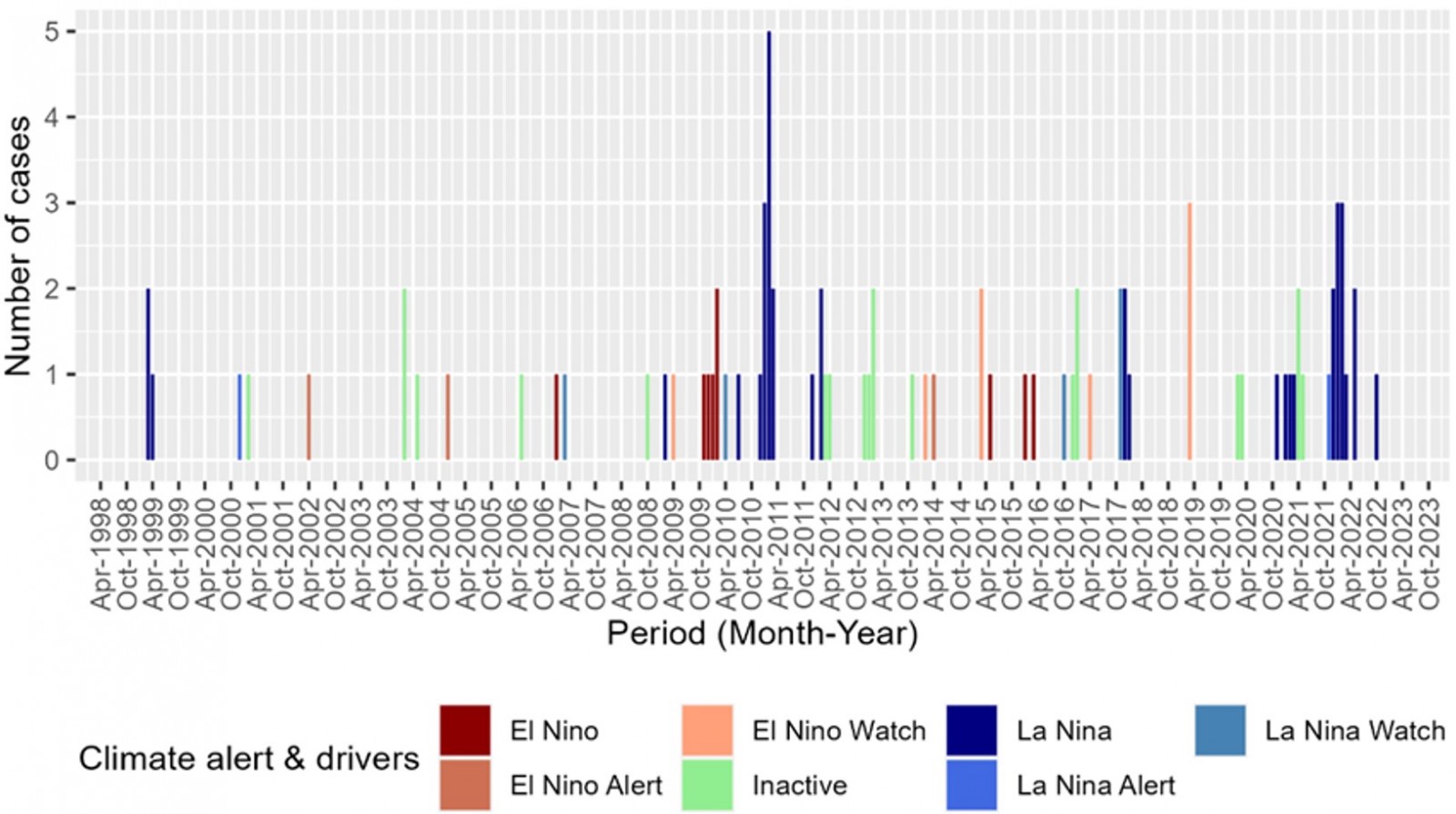 Figure 4: Vibrio vulnificus blood culture identified in Queensland April 1998 to October 2023. The graph demonstrates the monthly incidence of Vibrio vulnificus infection in Queensland by climate driver phase (1999–2022). Most of the spikes (rise in number of cases) in the calendar year correlate positively with the period of La Niña within Australia. Note: climate alert drivers information was collected from the Australian Government Bureau of Meteorology website.
Figure 4: Vibrio vulnificus blood culture identified in Queensland April 1998 to October 2023. The graph demonstrates the monthly incidence of Vibrio vulnificus infection in Queensland by climate driver phase (1999–2022). Most of the spikes (rise in number of cases) in the calendar year correlate positively with the period of La Niña within Australia. Note: climate alert drivers information was collected from the Australian Government Bureau of Meteorology website.
Table 2: Incidence of Vibrio vulnificus and climate events from April 1998 to October 2023.
Table 2 shows the number, incidence rates and incidence rate ratio of infection during different climate phases. Note: Queensland population numbers were collected from the Australian Bureau of Statistics website.
| Event | Time exposed (years) | No. of cases (N=86) | Average population at risk | Population*years exposed | Incidence rates per 1,000,000 population years (at risk) | Incident rate ratio in the event when compared with neutral phase (95% CI) |
|---|---|---|---|---|---|---|
| La Niña | 3 | 38 | 4,421,053 | 13,263,159 | 2.9 | 4.7 (1.3–6.6) |
| El Niño | 6.4 | 9 | 4,301,200 | 27,599,367 | 0.3 | 0.5 (0.6–1.3) |
| Neutral phase | 14.6 | 39 | 4,402,591 | 64,204,452 | 0.6 | Ref |
Discussion
The authors’ anecdotal evidence suggests mud crabs are in high activity during major moon/tidal events and during periods of significant water flow, such as flooding events, feeding on the biological matter that was washed out to the rivers and sea. Local fishing people contend that ‘when the flooding rains come, so do the filter feeders and scavengers’. This knowledge predisposes the at-risk individuals in seeking high-risk activities, such as crabbing in post-flooded rivers. Quoting Patient number two, his ‘greatest regret was not the life-threatening infection, but the number of fresh crabs going to waste in the fridge’.
Climate change and its impacts have been previously well documented as a factor that increases necrotising infections presentations10. Table 2 also supports this theory because it shows an increasing case load over the last two decades in Queensland, Australia. After Hurricane Ian in Florida, USA in 2021, a sudden spike in documented cases of flesh-eating bacterial infections was identified. The Florida Department of Health in Lee County published a public health warning of a sudden spike in sewage-spill-related Vibrio infections11. In 2023, the Centre of Disease Control had warned of increasing V. vulnificus infection due to rising water temperatures and climate change12.
In contrast to the literature, we observed a far better outcome from severe necrotising fasciitis in our patients, despite all of them being part of the same demographic profile (elderly men with clinical comorbidities). All five patients had high post-operative mortality scores with APACHE III scores ranging between 36 and 103, giving an average mortality rate of 29.46%. All cases survived with variable significant limb loss and eventually were discharged home.
We believe that the outcome was related to the high index of suspicion of V. vulnificus infection in our local community and the awareness of the surgical team and intensive care staff that led to early aggressive surgical treatment and adequate antibiotic therapy2,12,13.
It is important to note that four of the five male patients were injured and subsequently infected while handling their own crab pots. Previously in Japan, Morimoto et al documented a case of a male patient being infected with Vibrio vulnificus while handling contaminated fishing gear14. It is reasonable to expect that a crab pot that has been submerged in a saltwater mangrove will not be sterile. By law, the Australian Maritime Safety Authority requires all domestic and commercial boats carry a first aid kit onboard. It is best practice to provide and seek first aid when injured on a boat15.
Conclusion
With a strong possibility of future floods due to climate change and the cyclic return of the La Niña in the near future1, this article highlights a potential public health issue. This case series demonstrates the importance of increased vigilance for necrotising fasciitis by frontline healthcare staff post-flooding waters. Future referral to environmental health and identification and escalation of a potential public health warning may need to be assessed for future flooding events.
Postscript
While completing this manuscript, a 94-year-old male was admitted to Hervey Bay Hospital ICU with necrotising fasciitis with a pus and blood-culture-positive Vibrio vulnificus infection. This male presented in February 2023 with sepsis from a crab-inflicted left lower leg cellulitis complicated by anaemia, kidney failure and myocardial infarction. He required debridement, dialysis, inotropes and ventilation and was subsequently transferred to a tertiary Brisbane hospital for cardiac interventions.
Funding
All authors were employees of Wide Bay Hospital and Health Service at the time of manuscript construction. In-kind support by Wide Bay Hospital and Health Services was provided for the development of this manuscript. No financial incentives were provided.
Conflicts of interest
The authors declare no conflicts of interest.
Consent and ethics approval
All patients or their next of kins provided a signed patient informed consent form for the use of their medical records in this case report. Ethics review of the manuscript for the publication of this case report was obtained from MetroSouth HREC (EX/2022/QMS/91616). The authors continue to enjoy crabbing and eating mud crabs as they are delicious.




