Introduction
Uninterrupted access to care remains a concern for 67% of Bangladeshis living in rural areas in 20131-3, who face access disparities compared to urban residents4,5. Availability of providers and affordability of care are key factors influencing access in rural areas6. In Bangladesh, government healthcare expenditures have continued to decrease over the years, and 34% of public sector posts remain vacant, most of which are in rural areas7. In 2014, the Bangladesh government recruited more than 6000 physicians to improve access for rural residents8. With around 70% of its 160 million population living in rural areas, it is critical to determine whether previously underserved individuals in Bangladesh's rural areas have improved access to health care because of the geographic and economic benefits. This article aims to assess the impact of the physician recruitment policy on access to care and the health status of rural residents of Bangladesh.
Many countries adopt the strategy of increasing provider supply to address the increasing healthcare needs of underserved communities. Researchers have examined how deploying mid-level non-physician providers in rural India impacts healthcare service utilization and health outcomes9. Brazil's Mais Médicos (More Physicians) program increased the supply of physicians and had mixed results regarding healthcare utilization and infant health metrics10,11. One study used a natural experiment in Norway to explore the impact of physician density on perinatal health outcomes12. A study of a Turkish policy presented insights into the broader effects of increasing hospital beds and health workers on resource utilization13. Another study evaluated the impact of assigning trained physicians versus non-physician providers on mortality rates in Nigeria, finding that improved access to physicians significantly reduced mortality14. Bangladesh is the most recent country to implement a provider recruitment policy to improve rural access.
One of the primary barriers to access to care in Bangladesh is the acute shortage of physicians in rural areas15. In 2011, there were only 21 doctors per 100,000 population in rural areas compared to 249 per 100,000 in urban areas16. Despite the vast number of rural primary care facilities, these are more likely to have only one provider and less likely to have multiple providers17. In the public healthcare sector, vacancies remain despite regular recruitment. From 2007 to 2013, compared to the total number of sanctioned posts, an average of 34% of physician posts were empty in Bangladesh's public healthcare system18. With the recruitment of 6368 physicians in 2014, the percentage of vacant positions came down to single digits (7%) for the first time in Bangladesh's history (Fig1).
Adding to the challenge is that 75–80% of the rural population, including those with low income, prefer non-physician providers over trained physicians4,19. There are more non-physician providers, including unqualified village doctors and pharmacy salespeople, than trained physicians or nurses in Bangladesh16. However, there are concerns about rural non-physicians providing medical care20, as they have only superficial knowledge of the conditions they treat21. Some rural non-physician providers receive no training at all, while others have varied levels of basic training: polli chikitshok (3–6 months of training from unregistered private organisations), local medical assistant and family planning, and medical assistant training20,22. Patients also prefer alternative treatment options such as religious or spiritual, self- and family treatment, homeopathy, and ayurvedic medicine23.
Low utilization of public healthcare facilities is observed for many reasons, including that, over the years, physical accessibility to public healthcare facilities has improved, but economic accessibility remains a barrier24. Patients prefer treatment at tertiary facilities to treatment at rural primary facilities17. In Bangladesh, the poorest households spend 10% of their monthly income on medicines as out-of-pocket expenditure25. They are less likely to report receiving prescribed medicines from public facilities26 as only 48% of primary facilities have essential medicines27. Primary care facilities also struggle to offer diagnostic services, and 66% of their patients have their diagnostic tests done outside the facility28.
Significant disparities exist between rural and urban households regarding catastrophic health expenditure, with this increasing steadily in rural households from 2005 to 201629. Bangladesh also has a growing income disparity between rural and urban areas. In 2010, the average monthly income per household in rural areas was 9468 Bangladeshi taka (BDT) (approximately A$162); in urban areas, it was BDT16,475 (approximately A$282)30. Any reduction in out-of-pocket healthcare costs would help reduce rural residents' high levels of income disparity.
Bangladesh has made significant progress in controlling infectious diseases31,32, but the primary care system faces challenges in meeting the needs of patients with non-communicable diseases33. Rural residents are burdened with 63% of NCDs34, with high prevalences of disease such as hypertension, cardiovascular disease, and chronic obstructive pulmonary disease34,35. The poorest rural households have more NCDs and comorbidities than households with higher socioeconomic conditions36,37, but are 8–10% less likely to consult primary healthcare services38.
To meet the challenges faced by primary care facilities serving the rural population, the Bangladesh government made a policy intervention in 2014 by hiring more than 6000 physicians. Although the number of physicians increased, whether beneficiaries utilized the newly available services has yet to be studied. The impact on the health status of rural beneficiaries is also unknown. This is one of the first studies to assess the impacts of physician recruitment on access to care and the health status of rural beneficiaries in Bangladesh.
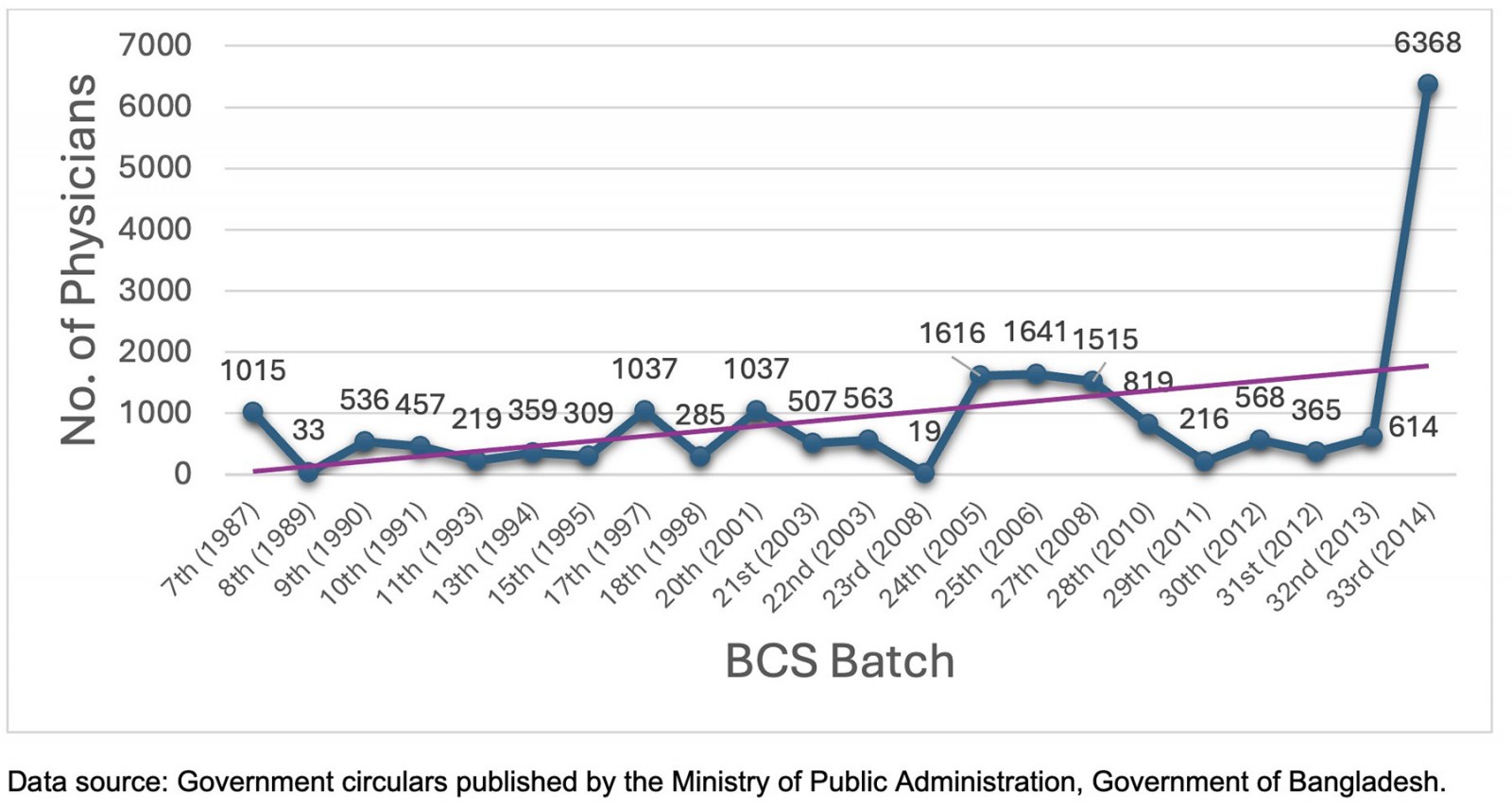 Figure 1: Trend of physician recruitment by Bangladesh Civil Service batch.
Figure 1: Trend of physician recruitment by Bangladesh Civil Service batch.
Methods
Data
This study uses data from the Household Income and Expenditure Survey (HIES) for 2005–201639. HIES is a nationally representative dataset that includes modules on topics such as household income, expenditure, consumption, savings, housing conditions, health and sanitation, and disability. The Bangladesh Bureau of Statistics began conducting the HIES survey in 1973–74 through a multi-stage stratified random sampling of households across Bangladesh. The Bangladesh government uses the HIES data to make policy decisions on several important public programs40. In our study, we analyze individual-level data by pooling three waves of HIES data – from 2005, 2010, and 2016 – with a study sample of more than 275,000 individuals from 68,400 households.
Study variables
Supplementary table 1 provides descriptive statistics for key study variables. To study access, we utilize five measures for access to providers. These are binary indicators for having consulted for illness: government health worker, government physician, private physician, pharmacy salesperson, and family or self-treatment. The supplementary analysis analyzes outcomes for the following providers: NGO health workers, homeopaths, ayurved, kabiraji or hekim, and other traditional or spiritual healers.
We analyze five measures of access to medicine, including government facility, NGO health facility, private facility, pharmacy or dispensary, and others.
We include five indicators for the cost of care: cost of visit, of medicine, of tests, of conveyance, and total cost. Data on the cost of care are adjusted for inflation using the Consumer Price Index for Bangladesh41 and is converted to the 2016 BDT value.
For health status outcomes (Supplementary table 2), we analyze binary indicators for reporting the following conditions: chronic heart disease, cancer, blood pressure, arthritis or rheumatism, eczema, diabetes (types 1 and 2), and paralysis. In the supplementary analysis, we also analyze outcomes for chronic fever, injuries or disability, chronic dysentery, gastric ulcer, leprosy, paralysis, hysteria or mental health conditions, and others.
Additionally, to understand the time spent on outpatient care, we analyze three outcomes: number of days from symptoms to visit, time spent reaching the provider, and time spent waiting for the provider (where time is measured in minutes).
Policy exposure
From 1987, the Public Service Commission of Bangladesh recruited physicians (medical officer/assistant surgeon) and dentists (assistant dental surgeon) for the public healthcare system. This includes physicians (not barefoot or village doctors) who obtained licensing certification from the Bangladesh Medical and Dental Council after completing their Bachelor of Medicine and Bachelor of Surgery or Bachelor of Dental Surgery. The age cap for public physician recruitment is 32 years, meaning most newly recruited physicians are fresh graduates or just a few years out of medical school. Supplementary figure 1 shows trends in the number of newly recruited physicians and the percentage of vacant posts in the public healthcare system.
Bangladesh has several administrative units, and the public healthcare sector is organized into primary (upazila, union, and village/ward), secondary (district), and tertiary (medical college and specialized institute) levels42. The newly recruited government physicians must complete a mandatory rural posting at the primary level, which has been compulsory since the 1980s and was reinforced again in 200843-45. A physician can pursue post-graduation training only after completing the mandatory 2-year period46. However, because of geographical hardships, there is an exception for three rural districts: Rangamati, Bandarban, and Khagrachhari, where the mandatory period is 1 year44.
Following the Bangladesh government policy decision to increase provider supply, the Public Service Commission recruited 6000 or more physicians, who formally joined the service on 7 August 201447. We use this natural experiment to assess access and health status impacts. Given that the physician recruitment policy of 2014 is determined exogenously to the local population, access and health outcomes should be causally impacted at intensive and extensive margins. Once the local population characteristics are controlled for, the backdoor source of the confounding effect is ruled out from the effect of the underlying treatment. The policy impacts outcomes on the extensive margins (ie whether getting access or not) and the intensive margins (how recruitment impacted other outcomes beyond access, such as health status).
Study design and estimation
The research design is a generalized difference-in-differences (DD) model comparing outcome changes within treatment or rural areas before and after the policy change to outcome changes within control or urban areas. DD is a commonly used method to study the impact of policies on access and health outcomes48-50. Following previous literature51,52, rural areas are considered the treatment group, as the physician recruitment policy's impacts are isolated to rural areas for the first 2 years, with few exceptions, as the physicians served in rural areas as stipulated by law. As the newly recruited physicians were not posted in secondary- or tertiary-level hospitals, urban areas are in the control group because they did not benefit from the new policy. In the study sample, data for 2005 and 2010 serve as the pre-period, and data for 2016 serve as the post-period. In this setting, the DD model helps to estimate the average treatment effects of the physician recruitment policy.
The DD regression is specified as follows:

In this model, Yiut is one of the access outcomes mentioned above for an individual i in an upazila u in a year t. RURALu is equal to 1 for rural areas and 0 for urban areas. POSTt is equal to 1 for the post-treatment period of 2016, when they received new providers under the government policy, and 0 for the pre-treatment period of 2005 and 2010.
Xiut includes the following individual-level covariates: age, sex, religion, marital status, employment status, and education. θd represents district fixed effects (0/1 indicators), which capture time-invariant differences between districts. γt is for time-fixed effects. Hence, β1 is the DD estimate of the provider recruitment policy effect on outcome Y. The interaction between RURALu and POSTt captures the causal impact of provider recruitment effects for rural areas compared to urban areas before and after the treatment policy was implemented in 2014.
Pre-trend check
The DD design assumes that outcomes would have changed similarly between the treatment and control areas in 2016 had the policy change or recruitment not happened in 2014. To test this assumption, we compare outcome trends between rural and urban areas before policy implementation using a regression model like that in the previous model equation by interacting the rural–urban indicator (RURALu) with one binary indicator for 2005 and another for 2010. We then test these interactions, which, if significant, would indicate differential pre-trends that might bias the DD estimates.
We estimate the regression models using weighted least squares with the HIES individual sampling weights. Standard errors are clustered at the rural level. All analyses are conducted using Stata v17 (StataCorp; https://www.stata.com).
Ethics approval
The Office of Research Protections and Integrity, University of North Carolina, reviewed this submission and determined that it does not constitute research on human subjects as defined under federal regulations 45 CFR 46.102(e) and 21 CFR 56.102(e).
Results
Provider recruitment effect on access to providers
Table 1 reports the estimated effects of provider recruitment on provider access from the model equation. Relative to urban respondents, rural respondents had an increase in the probability of visiting a government physician by 14 percentage points (p<0.01) and government health workers by one percentage point (p<0.05). The likelihood of visiting a private physician decreased by 15 percentage points (p<0.05). The provider recruitment significantly reduced the probability of getting treatment from a pharmacy salesperson by seven percentage points (p<0.10). The likelihood of receiving treatment from family or self-treatment decreased by two percentage points (p<0.05).
Supplementary table 3 presents results for additional provider outcomes. Provider recruitment increased the probability of receiving treatment from an ayurved, kabiraj, or hekim by one percentage point (p<0.10). The probability of receiving treatment from other traditional or spiritual healers decreased by one percentage point (p<0.05). There were suggestive or no changes in the likelihood of receiving treatment from an NGO health worker or homeopath.
Table 1: Difference-in-differences estimates of effects of provider recruitment on healthcare access for rural residents of Bangladesh, Household Income and Expenditure Survey 2005–2016†
|
Government health worker |
Government physician | Private physician | Pharmacy salesperson | Family or self-treatment |
|---|---|---|---|---|
|
0.01** |
0.14*** (0.00) |
–0.15** (0.00) |
–0.07* (0.01) |
–0.02** (0.00) |
*p<0.10, **p<0.05, ***p<0.01.
† Models adjust for age, sex, religion, marital status, employment status, and education, and include fixed effects for districts. Standard errors are clustered by rurality and are presented in parentheses. Sample size ranges between 31,195 and 42,711, depending on the outcome. Household Income and Expenditure Survey person-level sampling weights are used.
Provider recruitment effect on access to medicine
Table 2 estimates the effects of provider recruitment on access to medicine. The probability of receiving medicine from the government facilities increased by one percentage point (p<0.05) for rural residents compared to urban residents in the period following the recruitment of providers, relative to the prior years. There was a significant decline in getting medicines from pharmacies or dispensaries, by seven percentage points (p<0.10).
Table 2: Difference-in-differences estimates of effects of provider recruitment on access to medicines for rural residents of Bangladesh, Household Income and Expenditure Survey 2005–2016†
|
Government facility |
NGO health facility | Private facility | Pharmacy or dispensary | Others |
|---|---|---|---|---|
|
0.01** (0.00) |
–0.00 (0.00) | 0.00 (0.00) | –0.07* (0.01) | 0.01 (0.00) |
*p<0.10, **p<0.05, ***p<0.01.
† Models adjust for age, sex, religion, marital status, employment status, and education, and include fixed effects for districts. Standard errors are clustered by rurality and are presented in parentheses. Sample size ranges between 31,195 and 42,711, depending on the outcome. Household Income and Expenditure Survey person-level sampling weights are used.
Provider recruitment effect on outpatient care cost
For cost-of-care outcomes (Table 3), the policy intervention decreased the total cost of care in the previous 30 days for rural residents by BDT569.18 (A$9.74; p<0.10). The cost of diagnostic tests or experiments and visits decreased significantly for rural residents, by BDT179.90 (A$3.08; p<0.05) and BDT29.59 (A$0.51; p<0.05), respectively. However, the cost of conveyance increased by BDT33.91 (A$0.58; p<0.01), while the cost of medicine increased by BDT103.39 (A$1.77; p<0.05).
Table 3: Difference-in-differences estimates of effects of provider recruitment on cost of care (BDT)† for rural residents of Bangladesh, Household Income and Expenditure Survey 2005–2016¶
|
Cost of visit |
Cost of medicine | Cost of test | Cost of conveyance | Total cost of visit |
|---|---|---|---|---|
|
–29.59** |
103.39** (2.99) |
–179.90** (13.78) |
33.91*** (0.29) |
–569.18* (53.77) |
*p<0.10, **p<0.05, ***p<0.01.
†BDT1 = AUD0.017
¶Models adjust for age, sex, religion, marital status, employment status, and education, and include fixed effects for districts. Standard errors are clustered by rurality and are presented in parentheses. Sample size ranges between 31,195 and 42,711, depending on the outcome. Household Income and Expenditure Survey person-level sampling weights are used.
Provider recruitment effect on health status
Table 4 shows that, following the policy intervention, the probability of reporting NCDs increased by two percentage points (p<0.05) for chronic heart disease and four percentage points (p<0.10) for arthritis or rheumatism, with suggestive increases in reporting paralysis. However, there were no significant effects on the likelihood of reporting blood pressure, eczema, or diabetes. The probability of reporting cancer decreased by one percentage point (p<0.10).
Supplementary table 4 presents results for additional health condition indicators. Following the policy implementation, the probability of reporting gastric ulcer decreased by five percentage points (p<0.05), chronic fever and leprosy decreased by less than one percentage point (p<0.10), chronic dysentery by one percentage point (p<0.05), and mental health conditions by one percentage point (p<0.05). There were no discernible changes in reporting injuries or disabilities and asthma. Provider recruitment significantly increased the probability of reporting other diseases, by one percentage point (p<0.10).
Table 4: Difference-in-differences estimates of effects of provider recruitment on health status of rural residents of Bangladesh, Household Income and Expenditure Survey 2005–2016†
|
Chronic heart disease |
Cancer | Blood pressure | Arthritis or rheumatism | Eczema | Diabetes | Paralysis¶ |
|---|---|---|---|---|---|---|
|
0.02** |
–0.01* (0.00) |
0.01 (0.00) |
0.04* (0.00) |
0.00 (0.00) |
0.01 (0.00) |
0.00*** (0.00) |
*p<0.10, **p<0.05, ***p<0.01.
† Models adjust for age, sex, religion, marital status, employment status, and education, and include fixed effects for districts. Standard errors are clustered by rurality and are presented in parentheses. Sample size ranges between 31,195 and 42,711, depending on the outcome. Household Income and Expenditure Survey person-level sampling weights are used.
¶ The coefficient value for the paralysis outcome is 0.004*** to three decimal places.
Provider recruitment effect on time spent on outpatient care
Supplementary table 5 reports the effects of provider recruitment on the time spent accessing outpatient care. There was a significant decrease in the time spent reaching the provider, by 2 minutes (p<0.05). No change or effect was observed regarding the time spent waiting for the provider. Also, there were no significant changes in the number of days spent from the first appearance of a symptom to visiting a provider.
Robustness checks
To test the robustness of our results, we analyze models without the study sampling weights (Supplementary tables 6–9). The results from these analyses are generally similar to the main results for access to providers, medicine, cost of care, and health outcomes. The results of the robustness models confirm the validity of our study estimates.
Pre-trend checks
Supplementary table 10 reports the estimates of pre-recruitment trends for access to providers. There are no statistically significant differences between access to provider outcomes between rural and urban areas. Supplementary tables 11–13 report the pre-trends of access to medicines, cost of care, and health status by rurality, where no statistically significant differences were observed between rural and urban states in pre-trends (based on joint year tests or individual year differences). Overall, these results support the robustness of the estimated effects of provider recruitment on all outcomes.
Discussion
The 2014 physician recruitment was a landmark policy intervention to increase provider supply in Bangladesh. Our study finds that the policy improved rural residents' access to care and health status on various indicators. Before the policy implementation, there were several barriers to accessing health services at rural public facilities53,54. Despite these shortcomings, we find significant increases in the probability of visiting government physicians for rural residents compared to urban residents. In contrast, the likelihood of consulting a private physician or pharmacist decreased significantly. Similar evidence is found in other countries, like Brazil, where the More Physicians program increased physician visits across all age groups in underserved regions10. However, a study from Turkey shows that the increase in healthcare providers does not have a significant effect due to a potential mismatch in resource allocation13.
Previous studies have shown that most rural non-physician providers practice at their pharmacies20. There are various reasons for preferring non-physicians over physicians, especially among those in low socioeconomic circumstances23,55,56. The decline in treatment received from pharmacy salespeople in this study indicates that, post-2014, physicians were substituting the care previously provided by non-physician providers. Our findings align with studies that have seen trends of a shift from unqualified personnel to qualified physicians in rural areas57.
Our study demonstrates that, along with increased access to physicians, access to medicines at public facilities increased significantly post-intervention. Patient satisfaction increases with receipt of the complete course of medicine and prescribed diagnostic services at primary-level facilities58. Our findings indicate that the rural population utilized primary care facilities more than before. A study conducted in India revealed a 68% increase in monthly patient visits at public primary healthcare facilities following the introduction of mid-level providers9.
Affordability significantly predicts care-seeking behavior among patients with comorbidities6. Physicians working in rural private facilities face challenges such as tremendous resource constraints, and quality and safety concerns. Rural public facilities offer comprehensive healthcare services focusing on preventive public health initiatives and function as safety nets for the vulnerable rural population. Public healthcare services are provided at minimal cost, whereas private facilities have no regulation or monitoring on healthcare charges. Without expanding public services, the rural population remains vulnerable to excessive healthcare costs in private facilities. Therefore, our findings of increased public physician utilization and decreased private physician utilization indicate a potential substitution effect resulting from the recruitment policy, which will have significant spillover effects. Our results show that several cost indicators, including physician visit costs, decreased significantly for rural respondents. At public facilities, there is only a nominal fee for physician visits. The physician recruitment policy improved the availability of physicians in rural areas, who could be seen at minimal out-of-pocket cost. The diagnostic test fee schedule is also much lower in public than in private facilities. With the influx of physicians, diagnostic testing was conducted with renewed enthusiasm at the primary-level facilities. This significantly decreased diagnostic test costs for rural residents observed in this study. However, most primary care facilities do not have the provisions to offer a wide range of diagnostic services27. Despite the decrease in total cost of care, medicine costs increased significantly for rural patients. Circumstances such as diagnosis of previously undetected conditions, modification of previous prescriptions, and higher utilization of the newly available providers may explain the significant increase in out-of-pocket medicine costs observed in this study. Efforts must be made to increase the availability of medicines and diagnostic testing services at primary care facilities.
NCDs significantly predict household out-of-pocket expenditure59 and contribute to rural–urban gaps in catastrophic health expenditure29. Early diagnosis and treatment of NCDs improve rural beneficiaries’ quality of life and ability to contribute to the nation's economy, reduce costs and mortality rates60, and prevent comorbidities. We find that rural residents are reporting more NCDs, such as chronic heart disease and arthritis, which is important because mortality rates from cardiovascular diseases are projected to increase 21-fold by 202561. The shift from non-physicians to physicians may explain the higher probability of rural residents reporting NCDs. Previous studies have found that NCD diagnosis rates differ between physicians (60%) and untrained providers (35%)34. The physician influx has made available expertise in rural areas, indicating previous under-diagnosis of complex NCDs (ie rural residents had such conditions but remained undiagnosed). Our results also demonstrate that the likelihood of reporting cancer and mental health conditions decreased for rural residents. The coefficient decrease may signal a substitution effect as local care is being substituted with more specialized care at secondary- or tertiary-level facilities, as such providers are deficient in rural areas62,63. This also indicates a revitalization of the referral system at the primary level64.
Following the physician recruitment, we found that patients’ travel costs increased while travel time to providers decreased, and no significant impact was observed on waiting time. After policy implementation, patients accessing primary-level facilities must travel for treatment they previously received from nearby pharmacies or non-physician providers. A recent study found no impact of distance on the utilization of primary care facilities for rural women and children in Bangladesh65. Patient wait times are higher in public facilities compared to private facilities17, where physicians see an average of 40 patients daily and spend 16.17 minutes per consulting session64. Results of the present study show that, despite an increase in the number of people accessing public facilities, there was no significant impact on patient wait times. However, rural patients were unsatisfied with prolonged wait times at rural facilities before the policy implementation58,66. Efforts must be made to decrease wait times at primary-level facilities while maintaining a high quality of care.
Limitations
Our study has several limitations. Due to many missing values, we could not include important predictors such as income. The dataset did not have homogenous geocodes for study respondents across the years. The geographic boundaries of different local administrative units changed over time, and it was not possible to generate homogeneous or consistent identifiers for the local administrative units smaller than the district level. Therefore, we could only include district-level fixed effects in the study models. Health data were only collected from respondents having a recent healthcare incident and not from all study participants, limiting the sample size further. The study results suffer from power issues due to small and inconsistent sample sizes across the three waves of HIES data. As the study relies on group-level variables, there is a risk of ecological fallacy, drawing inferences about individuals based on aggregated data. For example, the probability of visiting a government physician represents group-level trends and should not be interpreted as reflecting the behavior or access of any individual. This limitation is particularly relevant in contexts like those of Bangladesh, where disparities in healthcare access may lead to unequal service utilization, even within the same geographic area.
Policy implications
The study results have several implications for developing countries like Bangladesh, which face challenges in retaining a sizeable physician workforce in rural areas. To continuously maintain low vacancy rates in rural areas, governments should hire an appropriate number of physicians and consider other policies for their retention. Without expanding public services, the rural population remains vulnerable to excessive healthcare costs in private facilities. Decreased medical costs following wider provider availability will contribute to reduced catastrophic health expenditure. The residual income from decreased out-of-pocket expenditure can be invested in other areas, such as education, nutrition, and income-generating activities. With a gradual shift in the morbidity patterns from communicable to NCDs, early detection and treatment can reduce socioeconomic disparities among rural residents. Strengthening the rural NCD treatment system by hiring specialists will ensure a healthier and more productive workforce, potentially having spillover effects on the economies of developing countries.
Conclusion
In this article, we empirically test if the increased supply of providers impacts access to providers and medicine, out-of-pocket costs, and health status among the rural population of Bangladesh. Overall, the results indicate that the policy intervention to increase physician supply in rural Bangladesh positively impacted various healthcare access and utilization aspects, including a shift towards formal healthcare services, enhanced access to medicines, reduced care costs, and increased NCD diagnoses. Developing countries should thus consider increasing the supply of physicians to improve rural residents' access to health care.
Funding
No funding was received for this research.
Conflicts of interest
The authors declare no conflicts of interest.
References
Supplementary material is available on the live site https://www.rrh.org.au/journal/article/9715/#supplementary
You might also be interested in:
2015 - Indonesian medical students' preferences associated with the intention toward rural practice
2011 - Attitudes of GPs towards Older Adults Psychology Services in the Scottish Highlands


