Introduction
Sustainable Development Goal 3 aims to reduce maternal and infant mortality. The global target is to reduce maternal mortality to fewer than 70 per 100,000 live births by 2030, with no country exceeding 140 per 100,0001. Despite its commitment, Indonesia reported a maternal mortality rate (MMR) of 189 per 100,000 in the 2020 census2, significantly higher than the Sustainable Development Goal target, and the rate of many South-East Asian countries3. Although Indonesia reduced the rate of neonatal mortality (at 0–28 days) to 18 per 1000 live births in 2022, expanding access to neonatal and intensive care, which are vital for reducing infant deaths (at 0–11 months), remains challenging4,5. Most of these maternal and infant deaths can be prevented6,7. These indicators are essential for a country's health, and have significant social and economic impacts8.
According to WHO, Indonesia's MMR was 173 deaths per 100,000 live births in 2020, approximately 1.3 times higher than the average of the South-East Asia region. This places Indonesia as the country with the fourth highest MMR, following Cambodia (218 per 100,000 live births), East Timor (204 per 100,000 live births), and Myanmar (179 per 100,000 live births). Indonesia's MMR declined by 42.8% from 2000 to 2020, which is less than the 58% decrease observed across South-East Asia during the past two decades9. Globally, the under-five mortality rate has more than halved since 2000, with 4.9 million under-five deaths in 2022, 2.3 million of which occurred in the first month of life and 2.6 million between the ages of 1 and 59 months. Indonesia's infant mortality rate (IMR) was 18 deaths per 1000 live births in 2022, nearly 1.5 times lower than the regional average in South-East Asia5.
As a way to lower MMR and IMR, the Indonesian government encourages women to give birth in medical buildings, like hospitals and health centers – these are called institutional deliveries. Article 14, Paragraph 1 of Regulation Number 97 of 2014, released by the Minister of Health of the Republic of Indonesia, says that giving birth must occur in a healthcare facility. This rule aims to lower the number of illnesses and deaths among mothers and kids10,11. However, efforts to improve the availability of trained medical staff in healthcare facilities to help with delivery are facing problems. Social, cultural, and economic conditions of communities make this difficult, and local resources aren't being used enough to help pregnant women and babies get the care they need in health centers12.
Previous research found that 39.6% of mothers in Gilgelbelles City, North West Ethiopia, 28.8% of mothers in the Benishangul Gumuz region, South West Ethiopia, 72% of mothers in Bule Hora City, and 44.82% of mothers in Bangladesh gave birth in health facilities. Some of the factors strongly linked to giving birth in a hospital are the mother's age (15–20 years), age of her first pregnancy, father's and mother's level of education (middle and high school education), the mother’s parity, her good awareness of birth preparedness and a complications readiness plan, her ability to make decisions, her ability to travel less than 30 minutes to get to the nearest health facility, her knowledge of birth preparation and what to do if something goes wrong, marriage after the age of 18 years, her having at least one problem during her pregnancy, and having fewer than two children. Institutional delivery services aren't used often because of cultural issues in the community and health centers that don't have the correct delivery equipment13-16. From this, we can see that there are still significant problems with government delivery services.
According to the 2023 Indonesian Health Survey, 89.9% of deliveries occurred in health facilities17. However, in several remote and underdeveloped provinces, the utilization of these services remains low due to unequal access to transportation and communication across the Indonesian archipelago. For instance, in Maluku Province, where most of the region is water, only 48.2% of deliveries occur in health facilities. North Maluku has a slightly higher rate of 63.6%, below the national average17. Maternal mortality in these provinces is 1.34 to 1.38 times higher than the national rate2. The Indonesian government has introduced maternity waiting homes near primary healthcare centers or hospitals to address these challenges, particularly in remote areas such as Maluku18. A maternity waiting home is a place or room located near a health facility (health center, hospital) that can be used as a temporary residence for pregnant women and their companions (husband/cadre/traditional midwife or family) for several days while waiting for labor to arrive, and for several days after giving birth13. In the maternity waiting home, mothers are observed for 14 days: 1 week before and 1 week after giving birth. While receiving services at the maternity waiting home, pregnant women who are at high risk are cared for and observed by health workers19,20.
As of May 2025, there was no official data on the exact number of maternity waiting homes in Maluku and North Maluku provinces. Available information indicates that maternity waiting homes have been implemented in several areas to increase access to maternity services, especially in remote areas and islands19-21. These facilities are providing temporary accommodation for pregnant women and their companions before and after delivery to improve the early detection and treatment of maternal and infant complications, and contribute to efforts to reduce maternal and infant mortality rates22.
In this context, this study aims to investigate the use of maternity waiting homes and their impact on increasing institutional deliveries in remote island regions of Indonesia.
Methods
Data source and study design
The study was mainly based on information from the Ministry of Health of the Republic of Indonesia's 2023 Indonesian Health Survey. Multistage and stratified random selection methods were used for interviews with household and individual instruments. The survey was conducted from May to July 2023, and 91.49% of people who answered it did so17.
In the 2023 Indonesian Health Survey, weighting ensured that the survey results accurately represent public health conditions at the national and regency/city levels. This process involves adjusting for differences in sample selection probabilities and correcting for potential bias due to non-response or imbalances in demographic distribution. Thus, indicators such as disease prevalence, nutritional status, and access to health services generated from the survey can be used to make more targeted health policies. The data used in weighting is from the population census and other administrative data, which are used to estimate population characteristics17.
Setting
The study setting is Maluku Province, one of Indonesia’s islands. Archipelagic terrain is one of the most extreme features of Maluku Province's geography. The province comprises at least 1286 islands across 11 towns and regencies23.
Participants
The study group included women who had given birth 5 years before the interview. The weighted group for the secondary analysis study comprised 1372 people.
Outcome variable
The outcome variable in our study was the use of institutional delivery (births in medical buildings like hospitals and health centers). The study divided use of an institutional service into ‘yes’ and ‘no’.
Exposure variables
The study used the utilization of maternity waiting homes as an exposure variable.
Control variables
Nine control variables were included in the study: type of residence, age group, marital status, level of education, job status, wealth status, health insurance ownership, antenatal care, and parity (number of previous births). Statistics Indonesia divides places of residence into two groups: urban and rural areas.
Age groups (years) were 19 or less, 20–24, 25–29, 30–34, 35–39, 40–45, and 45 or more. Marital status was married, divorced, or widowed. Education completed was categorized in five groups: no formal education, primary school, junior high school, senior high school, and college. The study divided job status into two groups: unemployed and working.
The wealth index in the 2023 Indonesian Health Survey is determined using a method similar to the 2018 Basic Health Survey. This method involves analyzing data related to household ownership and other indicators, such as access to clean water, sanitation, and energy sources. The poll found out how wealthy a home was by examining the items it owned. Families were surveyed on how many and what types of items they had (such as cars, TVs, and bikes), as well as how their home was kept (access to clean drinking water, toilets, and what materials were used to build the ground floor). The score was found using principal component analysis. Based on the total household scores of each person, five groups (each with 20% of the population) constituted the national wealth quintiles. These are the five levels of social status: poorest, poorer, middle class, richer, and richest24.
Exposure was measured based on the level of antenatal care. The Indonesian government continues to use an antenatal care model that is different from that of WHO’s 2016 recommendation that the minimum number of antenatal care visits be increased from four to eight. Indonesian government policy recommends antenatal care treatments at least six times for pregnancies that are considered to be uncomplicated. This includes one visit in the first trimester, two in the second, and three in the third. This includes one visit during the first trimester, two in the second and three in the third trimester10. The study divides antenatal care completeness into two groups: six or more visits and fewer than six visits.
Other categories were whether or not women had health insurance, and how many live births she had in total: primiparous (≤1), multiparous (2–4), or grand multiparous (>4).
Data analysis
First, the χ2 was used for bivariate analysis. In the second part of the investigation, the collinearity test was used to ensure that the independent factors had no significant relationships. We used the enter method for a binary logistic regression analysis for the last step. The study's adjusted odds ratios (AOR) have 95% confidence intervals (CI). The Statistical Package for the Social Sciences v26 (IBM Corp; https://www.ibm.com/products/spss-statistics) was used for statistical research.
The study used ArcGIS v10.3 (ESRI Inc.; https://www.esri.com/en-us/arcgis/products/arcgis-desktop/resources) to map the number of women in Maluku Province, Indonesia, who chose to give birth in a hospital and the number who were waiting to give birth at home. The Indonesian Statistics Service provided a shapefile with polygons showing administrative borders for the poll.
Ethics approval
The 2023 Indonesian Health Survey received authorization from the National Ethics Committee (No. LB.02.01/I/KE/L/287/2023). This secondary analysis is exempt from ethics approval. The survey utilized informed written consent, with participants or guardians providing their signed approval to ensure the voluntary and confidential character of the data-gathering process.
Results
The data show that only 6.8% of women in Indonesia's Maluku Province use maternity waiting homes; 46.1% give birth in an institution. Figure 1 presents the geographic distribution of maternity waiting home utilization rates in several regencies/cities of Maluku Province in 2023. Figure 2 shows the geographic distribution of institutional delivery rates in several regencies/towns of Maluku Province in 2023. The figures indicate the same tendency: the distribution of maternity waiting home utilization and the highest institutional delivery rate are in the same area, namely the northern part of Maluku Province. The area is the center of government of Maluku Province. This is likely because Maluku Province has more islands than North Maluku Province (not shown). This situation makes the availability of health services and public access to these health services more difficult geographically.
Table 1 shows the results of bivariate analysis. Regarding institutional delivery, women who deliver in institutional settings have a higher ratio of utilizing maternity waiting homes. According to the residence type, women in rural areas make up a higher proportion of maternity waiting home residents. Based on age group, women aged 30–34 years have the highest proportion of maternity waiting home utilization. Moreover, married women constituted the majority of maternity waiting home utilization.
Table 1 shows that women whose highest level of education was senior high school, who are unemployed and/or who were categorized as poorer are in the highest proportion in maternity waiting homes.
Table 1 also shows that the proportion of insured women in maternity waiting homes is almost three times that of uninsured women. Only women with six or more antenatal visits were at maternity waiting homes. Multiparous women made up the highest proportion in maternity waiting homes.
Table 2 presents the findings of binary logistic regression. Women who utilized maternity waiting homes were 2.756 times more likely than those without to deliver in an institutional setting (AOR 2.756; 95%CI 2.625–2.894). The result indicates that the utilization of maternity waiting homes is positively associated with institutional delivery in Maluku Province.
Furthermore, the study provides a comprehensive understanding of the factors influencing institutional delivery. It found seven control factors that play a significant role: type of residence, age group, education level, employment status, wealth status, health insurance ownership, and parity. For instance, the type of residence was a significant factor, with women in urban areas being almost twice as likely as those in rural areas to opt for institutional delivery (AOR 1.996; 95%CI 1.946–2.047).
Table 2 shows four maternal characteristics related to institutional delivery: age group, education level, employment status, and wealth status. According to health insurance ownership, insured women were 1.704 times more likely to achieve institutional delivery than uninsured women (AOR 1.704; 95%CI 1.663–1.745). Furthermore, all parity types were more likely than grand multiparous to have institutional delivery.
Table 1: Bivariate analysis results (n=1372)
| Variable | Characteristic | Maternity waiting home utilization | p-value | |
|---|---|---|---|---|
| No (%) (n=1263) | Yes (%) (n=109) | |||
| Institutional delivery | No | 55.8 | 28.3 | <0.001*** |
| Yes |
44.2 |
71.7 | ||
| Residence | Urban | 38.5 | 44.2 | <0.001*** |
| Rural |
61.5 |
55.8 | ||
| Age group (years) | ≤19 | 0.8 | 2.7 | <0.001*** |
| 20–24 |
15.1 |
10.5 | ||
| 25–29 |
26.5 |
17.7 | ||
| 30–34 |
27.0 |
28.9 | ||
| 35–39 |
19.0 |
24.8 | ||
| 40–44 |
8.7 |
12.8 | ||
| ≥45 |
2.9 |
2.6 | ||
| Marital status | Married | 95.1 | 95.8 | 0.001** |
| Divorced/widowed |
4.9 |
4.2 | ||
| Highest education level | No formal education | 1.3 | 2.1 | <0.001*** |
| Primary school |
16.8 |
12.1 | ||
| Junior high school |
17.0 |
9.3 | ||
| Senior high school |
45.9 |
50.9 | ||
| College |
19.0 |
25.6 | ||
| Employment status | Unemployed | 64.7 | 59.3 | |
| Employed |
35.3 |
40.7 | ||
| Wealth status | Poorest | 40.1 | 19.4 | <0.001*** |
| Poorer |
24.5 |
27.8 | ||
| Middle |
14.1 |
26.0 | ||
| Richer |
12.0 |
13.7 | ||
| Richest |
9.4 |
13.1 | ||
| Health insurance | Uninsured | 43.5 | 25.1 | <0.001*** |
| Insured |
56.5 |
74.9 | ||
| Antenatal care visits | <6 | 0.3 | 0.0 | <0.001*** |
| ≥6 |
99.7 |
100.0 | ||
| Parity | Primiparous (≤1 birth) | 27.0 | 28.7 | <0.001*** |
| Multiparous (2–4 births) |
62.0 |
61.9 | ||
| Grand multiparous (>4 births) |
11.0 |
9.4 | ||
*p<0.05, **p<0.01, ***p<0.001.
Table 2: Results of binary logistic regression (n=1372)
| Variable | Institutional delivery | |||
|---|---|---|---|---|
| p-value | Adjusted odds ratio | 95% confidence interval | ||
| Lower bound | Upper bound | |||
| Maternity waiting home: No (reference) | – | – | – | – |
| Maternity waiting home: Yes | <0.001*** | 2.756 | 2.625 | 2.894 |
| Residence: Urban | <0.001*** | 1.996 | 1.946 | 2.047 |
| Residence: Rural (reference) | – | – | – | – |
| Age group (years): ≤19 | <0.001*** | 1.783 | 1.559 | 2.039 |
| Age group: 20–24 | <0.001*** | 1.600 | 1.482 | 1.728 |
| Age group: 25–29 | 0.270 | 1.042 | 0.968 | 1.122 |
| Age group: 30–34 | 0.579 | 0.980 | 0.911 | 1.054 |
| Age group: 35–39 | 0.001** | 0.878 | 0.816 | 0.946 |
| Age group: 40–44 | <0.001*** | 2.145 | 1.982 | 2.321 |
| Age group: ≥45 (reference) | – | – | – | – |
| Marital status: Married | 0.618 | 1.014 | 0.961 | 1.070 |
| Marital status: Divorced/widowed (reference) | – | – | – | – |
| Education: No formal education (reference) | – | – | – | – |
| Education: Primary school | <0.001*** | 1.470 | 1.307 | 1.653 |
| Education: Junior high school | <0.001*** | 1.921 | 1.709 | 2.159 |
| Education: Senior high school | <0.001*** | 1.867 | 1.664 | 2.096 |
| Education: College | <0.001*** | 2.277 | 2.022 | 2.564 |
| Employment: Unemployed (reference) | – | – | – | – |
| Employment: Employed | <0.001*** | 1.549 | 1.512 | 1.588 |
| Wealth: Poorest (reference) | – | – | – | – |
| Wealth: Poorer | <0.001*** | 1.151 | 1.117 | 1.186 |
| Wealth: Middle | <0.001*** | 2.036 | 1.965 | 2.109 |
| Wealth: Richer | <0.001*** | 2.917 | 2.802 | 3.036 |
| Wealth: Richest | <0.001*** | 3.305 | 3.147 | 3.470 |
| Health insurance: Uninsured (reference) | – | – | – | – |
| Health insurance: Insured | <0.001*** | 1.704 | 1.663 | 1.745 |
| Parity: Primiparous (≤1 birth) | <0.001*** | 2.013 | 1.914 | 2.118 |
| Parity: Multiparous (2–4 births) | <0.001*** | 1.510 | 1.447 | 1.576 |
| Parity: Grand multiparous (reference) (>4 births) | – | – | – | – |
*p<0.05, **p<0.01, ***p<0.001.
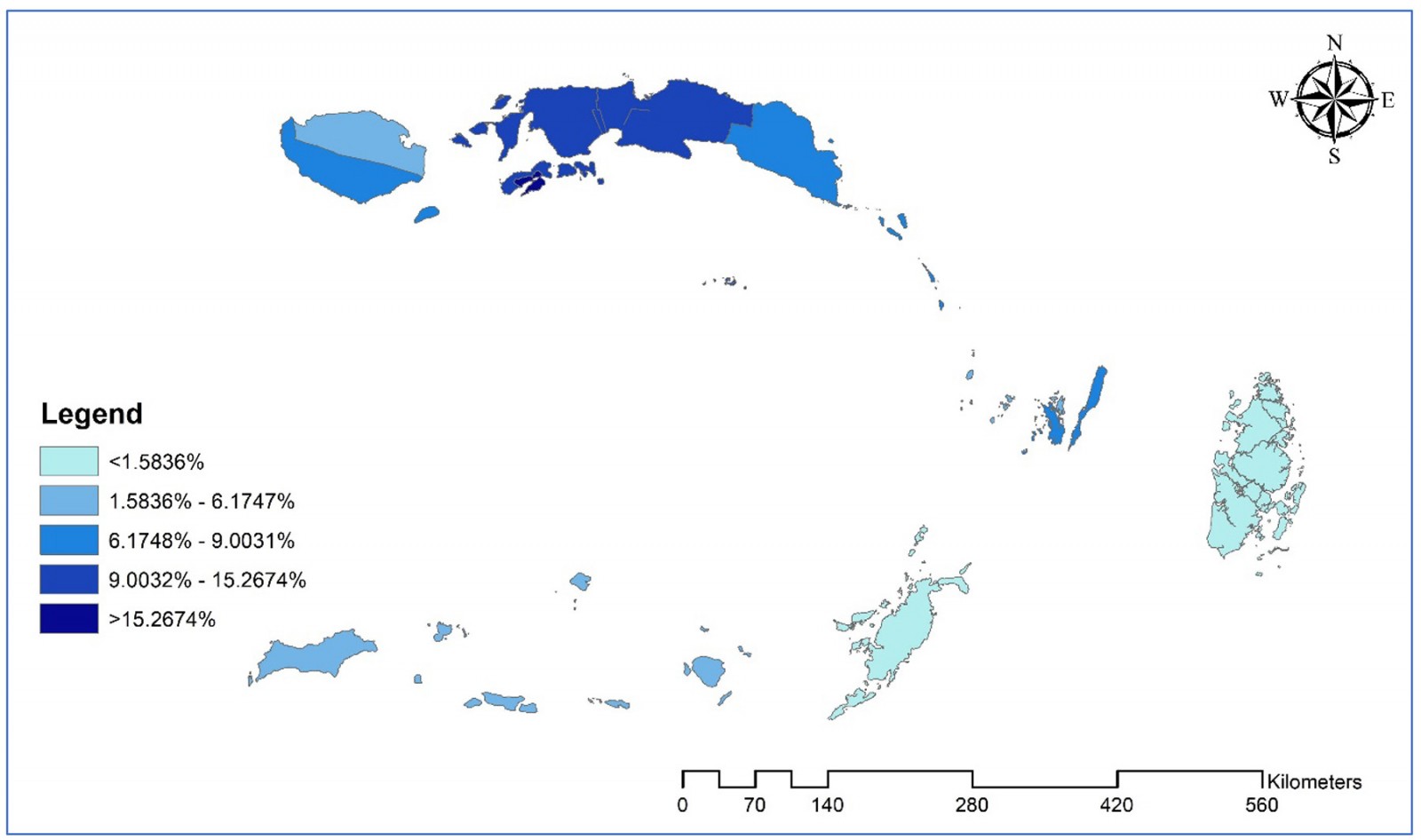 Figure 1: Geographic distribution of maternity waiting home utilization in several regencies/cities of Maluku Province, Indonesia, 2023.
Figure 1: Geographic distribution of maternity waiting home utilization in several regencies/cities of Maluku Province, Indonesia, 2023.
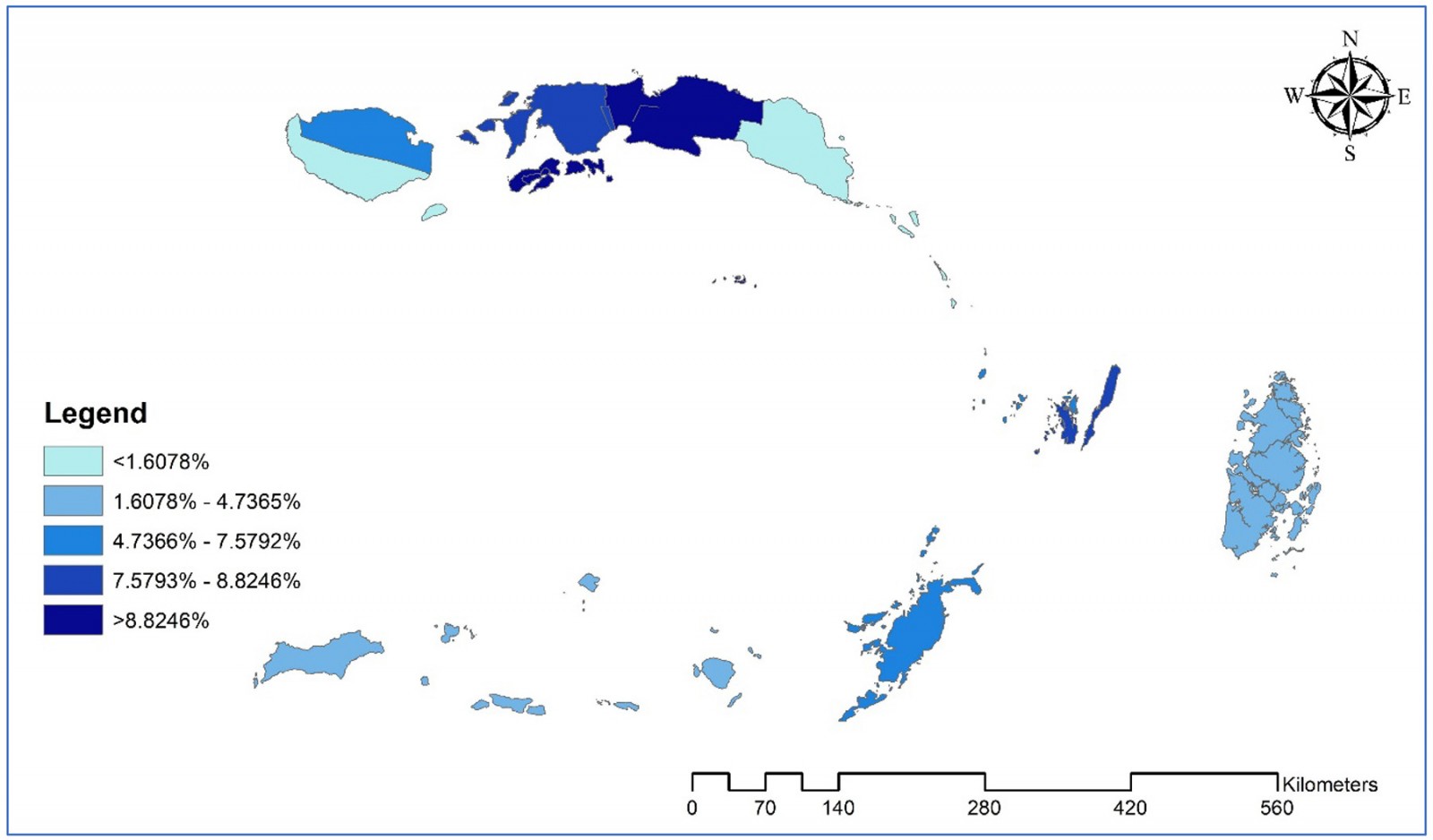 Figure 2: Geographic distribution of institutional delivery rate in several regencies/cities of Maluku Province, Indonesia, 2023.
Figure 2: Geographic distribution of institutional delivery rate in several regencies/cities of Maluku Province, Indonesia, 2023.
Discussion
Maternity waiting home utilization was related to institutional delivery in Indonesia’s Maluku Province. Thus, using maternity waiting homes could increase the possibility of institutional delivery. Maternity waiting home use was linked to institutional delivery in Indonesia's Maluku Province based on how often these homes were used. In the last few weeks of their pregnancy, pregnant women can stay at maternity waiting homes that are close to hospitals or other healthcare facilities. These homes are beneficial for women who live in remote or rural areas. The goal is to make sure that they can get medical help quickly when they go into labor25,26.
Thus, using maternity waiting homes could mean that a baby is more likely to be born in a hospital. Therefore, using maternity waiting homes could increase the likelihood of the baby being born in an institutional delivery. These results show that women are more likely to give birth in a hospital or clinic when these facilities are available and used25,27. The conclusion is that encouraging women to use maternity waiting homes might lead to more women choosing to give birth in a hospital. This is important because giving birth in a hospital or clinic usually gives better access to medical care, lowers the risks of giving birth, and improves overall outcomes and conditions for mothers and children. The statement stresses how important maternity waiting homes are in Maluku Province to boost institutional deliveries, making childbirth safer for women, especially those living in remote places25,28.
Numerous factors affect the utilization of maternity waiting homes in Maluku Province, especially among expectant women in isolated and rural regions. Geographic accessibility is crucial, as challenging terrain and restricted transit alternatives frequently impede prompt access to healthcare institutions, rendering waiting homes an essential alternative. Socioeconomic status influences utilization: women from low-income homes may have financial limitations that hinder their ability to remain in these facilities. Cultural views and familial support significantly influence decision-making, with certain women opting for home births due to traditional customs or insufficient encouragement from relatives. Moreover, awareness and understanding of the advantages of maternity waiting homes and institutional delivery are essential. Women who obtain adequate antenatal education are more inclined to utilize these services. Ultimately, the quality and comfort of the facilities, encompassing the provision of essential amenities and the courteous treatment by healthcare professionals, can either promote or deter their utilization19-21.
The results showed a stark contrast: women in urban areas were almost twice as likely as those in rural areas to opt for institutional delivery, highlighting the urgent need to address this disparity. Women who live in urban areas are more likely to be able to access healthcare facilities and services. In contrast, women who live in rural areas may have trouble because of distance, cost, or a lack of facilities. This is important because giving birth in a hospital or clinic provides better access to medical care, reduces the risks associated with childbirth, and improves outcomes for both mothers and babies29,30. Studies in China, Indonesia, and Iran found that facilities and transportation are easier to use in cities than rural areas. This makes the case for institutional delivery in urban places even stronger31-33.
The results showed four maternal characteristics related to institutional delivery: age group, education level, employment status, and wealth status. The age of the mother can affect her choice to give birth in a hospital. For instance, younger mothers may need to learn more about health issues or have better access to health care than older mothers, which can affect where they choose to give birth34. The amount of schooling completed by a mother was shown to affect her health decisions. Women with more education may know more about the benefits of giving birth in a hospital, have better access to healthcare information, and be more likely to choose a hospital-based delivery for safety reasons34,35.
Whether or not a mother is employed can affect her ability to access resources like health care and be financially independent. Some women who have jobs might be able to afford to give birth in a hospital, or their jobs might offer health insurance or other benefits, encouraging them to use hospitals29. The mother's income is a critical factor. Women with more money are more likely to be able to pay for the costs of giving birth in a hospital, such as getting there and back, as well as any medical care that may be needed. Less wealthy women, on the other hand, may have trouble accessing institutions because of financial issues36.
Insured women were significantly more likely to achieve institutional delivery than uninsured women. This underscores the crucial role of health insurance in providing access to health care, thereby increasing the likelihood of safe deliveries. The message stresses how vital health insurance is to ensure women can get medical care. Health insurance can make deliveries much safer by making it easier for women to give birth in a hospital. This lowers the risks of childbirth for both the mother and the baby37-39. When a woman gives birth in a hospital, having health insurance can lower the costs she has to pay. She also feels protected and safe, which makes her more likely to use birth services. The situation is also shown by a study that was done in Indonesia37. Furthermore, in Nepal, a study has shown that women who have health insurance are more likely to go to the hospital than women who don't38.
All parity types were more likely than grand multiparous to have institutional delivery. Since these women have already given birth more than once, they may feel more comfortable giving birth at home or think they don't need to go to an institution as much. But this can be dangerous because the chances of problems may increase with more babies. In a 2018 study in Nepal, about 74.4% of first-time mothers gave birth in health facilities40. A 2024 study in Ghana, where birth rates are high, showed that most mothers with four or more children decided to have non-health (traditional) help at home during their births41.
Strengths and limitations
This study examines many different datasets, which gives us helpful information about Indonesia's Maluku Province. Because it uses secondary data, the survey only considers essential factors.
Conclusion
Based on its findings, the study concluded that maternity waiting home utilization was related to institutional delivery in Indonesia’s Maluku Province. Thus, using maternity waiting homes could increase the possibility of institutional delivery.
The findings regarding maternity waiting for home utilization are in line with the government's efforts to reduce MMR and IMR. The government needs to build more maternity waiting homes in places that don't have easy access to medical care, such as remote or rural areas, with partnerships with non-government or international organizations to fund maternity waiting home expansion. This will make it easier for women who live far from healthcare centers to give birth in a hospital. Also, we need to ensure that maternity waiting homes have all the medical services and amenities that would make them more attractive and comfortable for pregnant women. This includes having enough places to stay, clean bathrooms, food, and trained medical staff available.
Acknowledgements
The authors are grateful to the Indonesian Ministry of Health for allowing them to examine the 2023 Indonesian Health Survey data.
Funding
The authors received no specific funding for this work.
Conflicts of interest
The authors declare that they have no competing interests.
Availability of data and materials
Authorized researchers can obtain the 2023 Indonesian Health Survey information at https://layanandata.kemkes.go.id.
References
You might also be interested in:
2020 - Organophosphate exposure and the chronic effects on farmers: a narrative review
2016 - Supporting nurses' transition to rural healthcare environments through mentorship
2014 - Correction, article no. 2907: Non-physician communities in Japan: are they still disadvantaged?



