Introduction
Rural communities have specific health needs because of their isolation, socioeconomic demographics and patient population1. New Zealand has traditionally used a model of care for rural health based on a medical general practitioner (GP) providing 24-hour care in the rural community2. However, this model is becoming less viable as GPs search for a better work–life balance3 and smaller rural populations decrease financial feasibility for GPs3, limiting patient access to rural health services3.
The rural nurse specialist (RNS) role has evolved to provide many healthcare services traditionally provided by GPs2,4. The RNS is a registered nurse (RN) with advanced nursing skills, enabling independent and autonomous practice. As the RNS role has been developed according to specific local community needs2, information regarding the RNS role is fragmented, creating a need for a descriptor of the RNS role in New Zealand.
Describing the RNS role is also hampered by a lack of formal definition for the term ‘rural’ within the literature. A lack of definition for the term ‘rural’ creates difficulties understanding the context in which the RNS operates. With no definition for ‘rural’, it then becomes difficult to define a RNS because they are specialising in an undefined area. Within New Zealand a rural community is defined by the distance to commute to an urban centre for employment5. However, there is no specific definition for rural health services. An RN may independently provide advanced assessments and treatments under the descriptor of ‘practice nurse’ or ‘district nurse’. Other terms such as ‘community nurse’ may also be used. There can also be confusion as clinical nurse specialists caring for a specific population within the rural area may consider themselves an RNS.
The purpose of this study was to provide a description of the RNS role in New Zealand. A clear descriptor of this role may provide further information for workforce planners, professional organisations, employers, and both current and future RNSs. The study was undertaken as part of the requirements of a Master of Nursing program. JB was the lead researcher, supported by two academic supervisors (RC, KH), who guided the research process.
Methods
A descriptive exploratory approach was used to conduct the research, which was completed in two phases in order to answer the following question: what are the core descriptors of the rural nurse specialist role in New Zealand? Data were collected in 2014–15.
Phase 1
Phase 1 consisted of document content analysis of five position descriptions of a rural nurse specialist or similar.
Sample: Five New Zealand District Health Boards (DHBs) were contacted and a request was made for a position description for an RNS role or similar. The request for a similar role was to allow for roles that may not have the title RNS to be included. The five DHBs were chosen based on the New Zealand Institute of Rural Health report Comparison of five District Health Boards6, because it provided a broad overview of the New Zealand health population. Initial contact with the DHBs was made by phone or email. Two position descriptions were found on the search engine Google.
Document content analysis: Document content analysis was undertaken. An inductive approach was used and data were categorised according to the Modified Strong Model of Advanced Practice7. This model provides five domains: direct comprehensive care, support of systems, education, research and professional development. Any data that did not fit into these domains were placed in a separate category. All raw data and analysis were reviewed by the academic supervisors (RC, KH). The results of the document content analysis were used to inform the interview questions for phase 2.
Phase 2
Phase 2 entailed interviews with four RNSs who were practising or had practised as an RNS in New Zealand within the previous year.
Sample: The sample for phase 2 was found using the snowball technique. A notice with the researcher’s contact details was placed in the national New Zealand College of Primary Nurses newsletter. An email describing the study was sent to the New Zealand Institute of Rural Health with the request for the study information to be passed on to potential participants. Criteria for participation in this study included RNs employed as RNSs with a broad range of patients practising in a rural area. Five potential participants responded, with one consequently excluded because the role only included a specific patient group in a rural area. After four interviews, data saturation was reached.
Interviews: Semi-structured interviews were conducted by telephone. The interviews were conducted in a private setting and recorded on a secure digital recorder. Interviews took an average of 45 minutes and were conducted by the researcher (JB). Raw data were reviewed by academic supervisors (RC, KH) after all identifying data had been removed.
Data analysis: Thematic analysis was used to categorise raw data. Data were categorised according to the Modified Strong Model of Advanced Practice6 to provide unity between phase 1 and phase 2 and allow comparisons. Initial data analysis was returned to the four participants for member checking8.
Ethics approval
Approval for this study was gained from the Eastern Institute of Technology Research and Ethics Approval Committee on 11 September 2014, Reference 39/14. Potential participants were invited to participate, and they were provided with information about the study. Participant consent was gained in writing, then verbally prior to the interview.
Results
A wide variety of position descriptions was obtained in phase 1, as seen in Table 1.
During phase 2, four participants were interviewed. Figure 1 shows the characteristics of the participants.
The findings of both phases are presented within the domains suggested by the Modified Strong Model of Advanced Practice7.
Table 1: Position descriptions of a rural nurse specialist or similar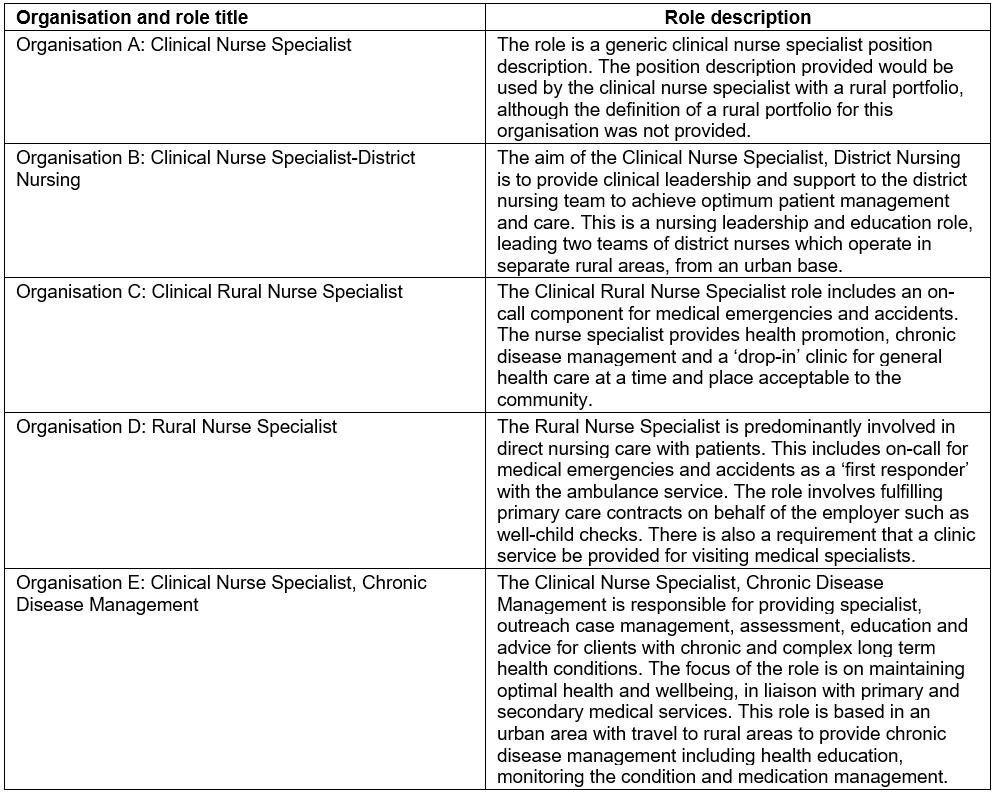
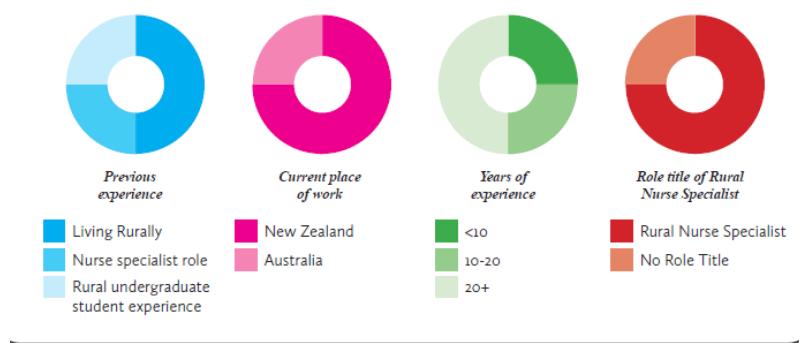 Figure 1: Characteristics of participants in phase 2.
Figure 1: Characteristics of participants in phase 2.
Domain 1: direct comprehensive care
‘Direct comprehensive care’ refers to all direct patient care including dissemination and assessment of investigative results7. Analysis of job descriptions in phase 1 revealed that all but one organisation required the RNS to provide advanced patient management to the population. Two organisations additionally required on-call skills to provide emergency health care.
Participants in phase 2 considered direct patient care to be the most important aspect of their role. Patient care utilised advanced assessment skills such as physical assessment, diagnosis and treatment in a variety of settings. Participants typically worked from a community clinic providing a ‘walk-in’ service, assessing and treating acute presentations.
Nurse D stated, ‘I see children with infections, sick children, I diagnose and treat [urinary tract infections]. I do a bit of upper respiratory tract infections, throat infections, skin infections and mastitis. I see essentially anything that walks through the door realistically.’
Two participants provided on-call emergency care where acute assessment skills were utilised after hours in conjunction with the ambulance service. On-call services were considered a challenge because the RNS was often the sole health professional at the scene. The hours of work required were considered a potential stressor, demonstrated by one participant who would complete 64 hours of work for one weekend on call (Friday night until Monday morning).
Patient care was provided independently, with comprehensive assessment, diagnosis and treatment skills considered essential. At the time of data collection, treatment with medication was based on the standing order system. However, all participants felt that the ability to prescribe would allow them to maximise the services they were able to provide to the community.
Domain 2: support of systems
Support of systems focuses on nursing care that is innovative and facilitates patient movement through the health system with a focus on role advocacy7.
During phase 1, effective communication skills were considered crucial in all position descriptions. Communication was important both within the immediate healthcare team and throughout the wider, regional healthcare team to safely facilitate patient care. Quality assurance activities were also included in this category. Health and safety was a key focus of all five position descriptions.
Participants in phase 2 demonstrated different ways of facilitating patient movement through the health system. Nurse A was developing health technology to assist patient access to health services. Nurse D was involved in practice management as no-one else was available to fill the role.
Collaboration with medical staff, pre-hospital carers and other health professionals providing secondary care was considered a critical tool to assist a smooth transition of care for the patient.
Nurse C stated, ‘it’s important to work in collaboration as well with the doctors and the rest of the healthcare team’.
Close collaboration within the immediate healthcare team especially the GP allowed the RNS to upskill practice to take on responsibilities traditionally provided by the GP. Participants developed advanced assessment and treatment skills to respond to acute presentations and thus enable the GP to see more complex patients.
Domain 3: education
Education in this context is related to the use of the RNSs’ advanced knowledge to educate both colleagues and patients7. In this study, education required to maintain an advanced knowledge base was included in this domain.
Position descriptions were noted to have a high expectation of the RNS using their advanced knowledge base to provide education to other healthcare professionals. Three position descriptions had a patient-centred approach to education, with specific requirements for their communities. The expectation from these organisations centred around the RNS providing education to promote self-management of health and wellbeing to the community.
Formal educational expectations amongst the organisations differed. Two organisations required a postgraduate certificate and three required a Masters degree relevant to the RNS’s area of practice. Each position description had specific local certification such as IV cannulation, cervical smears, PRIME (primary response in medical emergency) and vaccination.
Within phase 2, three key concepts emerged in relation to this domain: health promotion, the specialist generalist role and upskilling the RNS.
Health promotion: ‘Health promotion’ refers to patient education and promoting health and wellbeing within the community. RNSs believed in developing strong community relationships to understand local health needs. Nurse D noted the connection with the local community is important, allowing the RNS to provide relevant healthcare services.
Effective communication was also considered important because the participants worked with a wide range of patients across the lifespan.
Nurse A stated, ‘you have got to know how to have the conversation with the kids but then you can also have a conversation that shows respect to someone that’s dealing with an elder passing’.
Specialist generalist: ‘Specialist generalist’ is a term used by participants to describe their advanced practice with a wide range of patients across the lifespan. Being a specialist generalist was considered by participants to be unique to the RNS role because they provided advanced and autonomous assessment and treatment to a wide range of patients with a broad range of presentations. The specialist generalist nature of the role was considered a motivator for the RNSs when pursuing further education.
Upskilling: Upskilling is required to ensure the RNS maintains an advanced knowledge base to respond appropriately to a broad range of clinical situations. This was considered very important by participants and as one of the biggest challenges within the RNS role, because the wide range of conditions presented in the rural environment meant that participants were concerned they may not be up to date with best practice.
Nurse A stated, ‘I also had to learn lots about everything else and be really generalist and I was a bit fearful of how much I know, as to how much I’ve, you know, the capacity that I had to upskill’.
Upskilling was undertaken both formally and informally. All participants were engaged in postgraduate study. Postgraduate study was considered an important part of the RNS identity, setting them apart from other registered nurses.
Nurse C described, ‘I guess the difference between myself … and a practice nurse was having that postgraduate study’.
Upskilling also occurred within collegial relationships at work. A working environment that provided a positive learning opportunities was considered essential to upskilling.
Nurse B stated, ‘You need to have a good supporting GP so you advance in it [advanced practice] at that level. If you just get thrown into it and you work there and don’t get any more support from there on then I kind of think you can actually start to learn bad things because you’re not actually really getting the medical supervision’.
Domain 4: research
‘Research’ refers to the ability to generate knowledge and integrate research into practice and pass this on, to promote a culture of change within the work environment7.
During phase 1, each organisation had research requirements specific to the role; however, there was a wide variance in requirements for research participation. These ranged from maintaining nursing standards to maintaining an up-to-date pharmaceutical formulary.
Within phase 2 participants identified policy development as an aspect to their role that required research. Each participant would assess a clinical need and develop a best-practice policy in response to that need.
Nurse A gave this example: ‘'This is the evidence that we have on gout, can we have a standing order please?' and this is what developed and we have monthly meetings that give us the opportunity to talk about there’s a need for a new standing order’.
Domain 5: professional development
Publication and professional leadership refers to the RNSs’ dissemination of knowledge outside the work environment and participation in supporting organisations7. Within phase 1, there was no requirement for professional leadership outside the work environment.
During phase 2, one participant indicated she was active in a group of rural nurses from the community who met for education and support. Another participant believed professional leadership, while important, was a potential stressor that may lead to burnout.
Additional themes arising from the data included stress management and lack of recognition role. Both themes were cited as important to the participants.
Stress management: Stress management was initially recognised in phase 1, as organisations required the RNS to demonstrate an ability to deal with stressful situations and have an effective debriefing strategy.
Within phase 2, participants identified several different aspects of stress management including recognising triggers, professional boundaries and having a strong support network. All participants recognised the importance of identifying stress triggers and developing individual coping mechanisms.
Nurse A chose an RNS role with no on-call requirement because the long hours were considered a stress trigger.
The rural community itself was recognised as a stress trigger, due to the small community creating blurred lines between social and professional boundaries. Nurse D developed friendships within their community, but stipulated within the friendships that health matters were to be discussed at work within their professional capacity.
All participants utilised family members as a support network, with one participant taking her husband to any ambulance callouts where she felt unsafe alone. Two participants had professional counselling or clinical supervision as a method of stress management.
Lack of recognition: Lack of recognition of the advanced practice role motivated participants to take part in this study. Participants felt that other health professionals did not recognise their role or their RNS skills.
Lack of recognition led to an adverse effect on patient care: lack of recognition or acceptance, by other health professionals, of an RNS assessment prevented smooth transition of patients through the health system. Participants also believed that lack of recognition and poor understanding of the RNS role meant their assessments and treatments of patients were at times questioned by other health professionals or repeated unnecessarily.
The inconsistent use of a title and position description was considered a major influence on interprofessional relationships. Each participant in this study had a different position description and title, ranging from a specific RNS title to no title.
Nurse B gave an example of lack of tailoring a position description to a local community when moving into a new role: ‘I gave them my position description from town B and they looked at it and said, '… that’s good you’ll just work like that', because it was new, they hadn’t had them [RNSs], but of course that puts me at a barrier anyways, because some of the practice nurses were unaware of it [RNS role] and half the GPs were unaware of it’.
Participants believed a lack of recognition led to isolation from the health team as well as professional development because they were excluded from both GP education and nurse education. Advanced postgraduate studies and the difference education made to the participants’ practice were not recognised by other health professionals, particularly other nurses.
Nurse C stated, ‘helping your colleagues to understand why you actually go on and develop your postgraduate education ‘cos that is often I mean; you know I had nurses saying to me 'well what is it that you do that is different?' They don’t understand that your knowledge is different and it actually makes their practice different. That’s been a real challenge, yeah like I mean I’ve had comments from staff of 'what makes you think you can call yourself a rural nurse specialist, we don’t have those here'’.
A conceptual model of findings is provided in Figure 2.
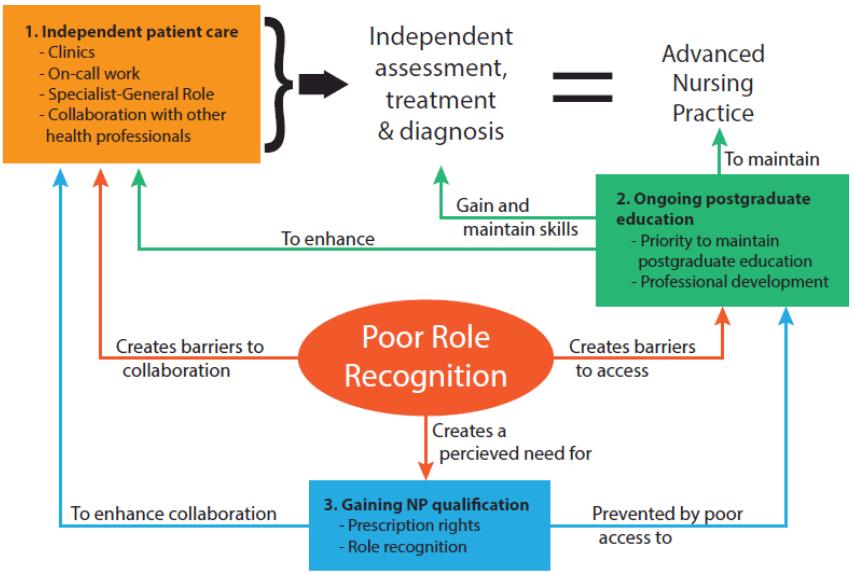 Figure 2: Core components of the rural nurse specialist role in New Zealand.
Figure 2: Core components of the rural nurse specialist role in New Zealand.
Discussion
This study was conducted using a descriptive exploratory approach to explore the core descriptors of the RNS role in New Zealand. Useful descriptors include independent patient care utilising advanced assessment, treatment and diagnostic skills. These skills were gained through postgraduate study. The isolation in which an RNS practices creates a need for these skills because there is a lack of health professionals. However, isolation also creates a barrier to accessing postgraduate education. The RNS role is relationship-centred and focuses on community needs. Role recognition is essential to provide collaborative care within the interprofessional healthcare team. These findings will be discussed based on the framework provided by the Modified Strong Model of Advanced Practice7. The themes discussed here are based on and emerged within the framework categories during phase 2 of the study.
‘Rural’ and the context of direct comprehensive care
Direct comprehensive care was identified as an important part of the RNS role by participants. An understanding of the term ‘rural’ is required to understand the context in which direct comprehensive care is provided.
Despite the lack of consistent definition, common characteristics of a rural population include a small population with geographical isolation between health providers9, which creates a generalist role4,10-15.
The term ‘generalist’ is used to describe the broad range of presentations the RNS treats across all stages of life12,15-18. Patients present with various conditions infrequently and at different stages of acuity10-13,15,17. ‘Generalist’ can create confusion within the literature because, in some literature, a generalist is the equivalent of a registered nurse19.
The term ‘specialist generalist’ was used by participants to describe their practice. While ‘generalist’ refers to the broad range of patients treated by the RNS (ie the specialty area of practice), ‘specialist’ refers to the advanced practice skills the RNS uses within their scope of practice1,10,15. The use of advanced practice skills can be termed specialist, because the RNS is practising at an advanced level within their scope of practice20. Therefore, the term ‘specialist generalist’ can be used to describe the RNS providing care using advanced skills (specialist) within a wide range of settings (generalist).
Advanced practice in rural settings
Advanced practice is utilised by RNSs in response to the geographical isolation between health providers within the rural setting. International literature also describes this trend in both Greenland and the USA10,16. The USA has formally recognised advanced practice with specific titles and prescribing rights10.
Advanced practice was evidenced by participants in nurse-led clinics and when undertaking emergency after-hours call, with GP support.
At the time of this study, standing orders were utilised to provide treatment. Standing orders provide criteria for prescribing medication and are designed to be provided by the GP or dentist working with the nurse21. However, these were difficult to use in the rural setting due to a lack of GPs to write the standing order22. All participants in this study were pursuing NP status in order to gain prescribing rights. In 2017, nurse prescribing for registered nurses was introduced in New Zealand, creating another avenue for the rural population to access healthcare services.
Role clarity and collaborative practice
In order to facilitate effective patient movement through the health system, the RNS requires role clarity18. The ability to work more autonomously would also facilitate effective patient care.
Role clarity occurs between health professionals when there are clear expectations of behaviours within that setting18. Role clarity enables role recognition, creating effective collaboration and enabling improved access to healthcare for rural populations18,23,24. Within this study, lack of role clarity led to poor communication and poor understanding of the RNS role, creating ineffective collaboration with other health professionals. Collaborative practice can provide the support needed to promote autonomous role development18. The collaborative relationship with GPs during ‘normal’ working hours led to improved advanced, autonomous skill development for after-hours care provision.
Geographical isolation and autonomous role development
Autonomous role development can also be a result of large geographical distances between healthcare providers9. Coordinating the care of an acutely unwell patient in an isolated area is a skill unique to rural healthcare provision10,25-27. Geographical isolation creates challenges for transport provision as weather may isolate areas and prevent air or road travel. Transport services are different in each community according to the local needs1,10,11,16,25. Autonomous role development occurred in this study as participants took on after-hours responsibilities, managing their own clinics and answering emergency calls with the ambulance teams. RNS sharing after-hours work with GPs helps retain GPs in the local area, in response to a decrease in rural GPs in New Zealand4,21.
Relationship-centred practice
Relationship-centred practice is essential to the RNS role. Building relationships within the community can be challenging because rural communities can be based on a network of ‘who knows who’11,26. This network means that initially there is minimal trust in the RNS role27,28 Once trust is gained there can be challenges in setting professional and personal boundaries1,27,28. Participants had different views regarding boundary setting, with some feeling they were constantly at work. Due to the nature of the rural community the social behaviour of an RNS can affect the community’s perception of their professional ability and vice-versa1,11,28.
Community relationships are pivotal to the RNS role as services are provided based on a community’s identified health needs12,17,26. During phase 1, only one position description identified community education as a priority. Within phase 2, relationships with the community were identified as important by participants as a large portion of their time was spent in health promotion.
A positive interprofessional relationship with the healthcare team encourages interprofessional education, enhances professional development and lessens professional isolation18,29. This ultimately benefits the patient by enhancing the collaborative relationship, allowing for better healthcare provision30.
Negative interprofessional relationships are seen to increase professional isolation and decrease professional development for the RNS18,29. Negative interprofessional relationships can also lead to a patient experiencing delay in receiving care or a lack of interim care such as verbal orders of analgesia.
The wider healthcare team may include allied health staff, mental health staff and emergency services (fire, police, ambulance)13,18, and specialists in a secondary healthcare facility29. The wider healthcare team comes from a variety of backgrounds, requiring the RNS to have adaptable communication29. Due to geographical isolation, much of this communication is carried out by phone rather than face to face 4,18,28,29. Having face-to-face contact has been shown to enhance interprofessional relationships and collaboration18.
In phase 1, emphasis was placed on the ability to communicate well and work within a healthcare team. These requirements varied according to each position description – some position descriptions required the RNS to work with specific team members. Interprofessional education and postgraduate education are two strategies that may encourage effective collaboration18.During phase 2, positive relationships with the interprofessional team allowed all participants to develop the skills and resources to provide the services needed by the community. Participants’ discussion around collaborative care focused on relationships with the medical team.
Education
Postgraduate education emerged as an essential component of the role within phase 1 and phase 2, which is supported by international literature1,10,31. Postgraduate study enhanced collaborative care by providing the RNS with the language to clearly communicate with other health professionals4,32. Postgraduate education can be hampered by geographical isolation. Barriers to completing postgraduate education include travel away from home and education aimed at health professionals in urban centres12,33,34.
Geographical isolation requires an RNS to provide expanded services in a wide range of environments9,12,13,35. This generalist role is beginning to fall into the realm of RNSs due to a lack of wider health professionals3,4,30,35-37. Participants believed postgraduate study gave them the skills and confidence to provide specialist generalist care.
Postgraduate educationwas considered an essential element of the RNS role during both phase 1 and phase 2. There was inconsistency during phase 1 regarding the level of educational requirements. This variation reflects an overall lack of consistency in postgraduate education for nurse specialists in New Zealand30. During phase 2, postgraduate education was identified as important due to the specialist generalist nature of the role.
Participants in this study found that in-service professional development was often targeted at registered nurses, below the level of education of the participants, or at GPs33. Participants perceived themselves as excluded from in-house professional development.
NP registration was considered preferable as it provided greater role clarity – the NP role is already clearly delineated and recognised in New Zealand, whereas the RNS role is not30. Therefore NP registration was considered by all participants as a more effective way to provide advanced care in the rural environment. All participants had completed postgraduate study to a Masters level and were pursing NP qualifications. One participant was unable to obtain NP registration due to lack of support for an NP role.
Professional leadership may increase role visibility of the RNS35. Professional leadership was notably omitted from all position descriptions in phase 1. During phase 2, there were limited discussions regarding professional development. There were no specific questions regarding professional leadership so participants may not have discussed this if they did not think it was important.
Limitations
This study was conducted within New Zealand, with the samples for both phase 1 and 2 coming from the North Island and South Island. While the wide geographical range makes this study transferable within New Zealand, the information may not be internationally transferable due to differences in rural community needs and regulatory body requirements. Within phase 2 there were only four participants; however, the rich data collected tells the story of the lived experience of the RNS role.
Recommendations
Recommendations from this study include improving role clarity of the RNS role within the wider health team, thus enhancing collaborative care and improving patient care. RNS professional leadership would increase visibility in the healthcare sector. Professional organisations should including an RNS-specific group. Access to postgraduate education for RNSs is essential, thus increasing access to online resources is recommended. In-service education will be enhanced by role clarity.
Further research into the efficiency and use of the RNS role and the effect of the role on rural health is required. The perception of both GPs and the community of the RNS role would also be worthy of further investigation.
Recommendations include interprofessional education, considering an expanded role for the RNS in New Zealand and dissolving barriers to nursing education. The use of prescribing rights in the rural setting and its effect on accessible healthcare needs to be investigated as well as the effect of the RNS role on rural health outcomes.
Conclusion
The aim of this research was to provide a description of the RNS role within New Zealand. This study demonstrated a wide variance in the understanding of the term ‘RNS’. Phase 2 demonstrated that the role is centred around the community and their needs. Direct patient care is a priority and includes assessment, treatment and diagnosis of a wide range of presentations across the lifespan. The term ‘specialist generalist’ refers to the concept that the RNS utilises advanced nursing skills to care for a wide range of presentations.
The advanced assessment and treatment skills utilised by the RNS are gained through postgraduate study. Postgraduate study is also considered essential as it enhances the collaborative relationship between the RNS and the healthcare team. However, geographical isolation and lack of relevant postgraduate study can be barriers to accessing further education.
Lack of role clarity can create barriers to clear communication with other health professionals, and potentially affect patient care and movement through the health system. The NP role was considered more desirable because it carried more role clarity and role recognition.
Acknowledgements
The authors thank the participants in the study and the Eastern Institute of Technology for the support to complete this study. No financial support was received.

