Introduction
A health visitor’s ability to assess and analyse aspects of family resilience in daily practice is essential to enable practitioners to support families and facilitate positive lifestyle choices and improve child health and developmental outcomes. The Welsh Government in 2012 published A vision for health visiting in Wales and within it acknowledged that continual assessment was critical for health visitors to ensure that families were able to get the right support at the right time1. The purpose of the present study was to understand how health visitors perceived ‘family resilience’ and how they constructed it. This article presents the findings of an in-depth exploration of the concept of family resilience (as opposed to individual or community resilience) as understood and agreed by health visitors in Wales, using online integrated software. This was the first stage of a two-part research study that developed the Family Resilience Assessment Instrument Tool (FRAIT; www.frait.wales). This is a standardised form of assessment, measuring instrument, guidance, aide memoire, training package and community of practice for health visitors to use in their daily practice. It has the potential to identify whether family resilience differs across rural and urban communities in Wales. This work has supported the notion of an all-Wales universal provision of health visitor intervention as described within the Welsh Government (2016) Healthy Child Wales Programme2. The present article presents the first stage of the FRAIT research study, that of identifying the clusters (or constructs) within the concept of what health visitors in Wales perceive as ‘family resilience’.
Health visiting
‘Health visiting’ is the term used to describe a UK specialist community public health nursing service. As registered specialist community public health nurses, health visitors are regulated by the UK Nursing and Midwifery Council3. The Institute of Health Visiting in 2018 defines health visitors as:
… registered nurses/midwives who have additional training in community public health nursing. They provide a professional public health service based on best evidence of what works for individuals, families, groups and communities; enhancing health and reducing health inequalities through a proactive, universal service for all children 0-5 years and for vulnerable population targeted according to need. Health visiting is a proactive, universal service that provides a platform from which to reach out to individuals and vulnerable groups, taking into account their different dynamics and needs, and reducing in equalities in health. Pre-school children and their families are a key focus4.
The professional practice of health visiting is unique, as it includes the responsibility to work with both individuals and a population, which may mean taking decisions on behalf of a community or population without having direct contact with every individual in that community. Luker et al (p. 13) acknowledge the role of the Institute of Health Visiting as having ‘a core purpose of raising professional standards in health visiting practice’. They agree that health visitors have a key role in their work with families with children aged 0–5 years and contribute to public health outcomes through key performative skills such as talking, the home visit and the health visitor–client relationship. However, they also argue that in the context of devolution and a changing world of public policy and services integration, it means that health visitors will work far more closely with other professional groups and services such as social workers and education. They also recognise that health visiting needs to focus on understanding outcome measures that could evaluate health visiting and influence professional and services changes in the future5.
Health visiting provision across the UK is devolved to its respective governments, which have responsibility for workforce development, delivery and policy context2,6-9. Wales had an estimated population of 3.1 million in June 201610. It has pockets of high relative deprivation in the South Wales valleys and large cities, some North Wales coastal and border towns, with historically industrial Blaenau Gwent local authority (its most deprived) just 14.5 km from rural Monmouthshire, its area of least deprivation11. The National Health Service Wales in 2016 employed 870 whole time equivalent (WTE) health visitors, a rise of 111 WTE since 200912. In its most deprived areas, the Welsh Government has funded the Flying Start initiative, which delivers intensive multidisciplinary and interprofessional support to children and families in order to make a difference to their life chances, and health visitors are an integral element of Flying Start provision13. The health visitors working in Flying Start are employed by the health boards but commissioned to provide the health visiting component of Flying Start by the local authority.
In 2012, the Welsh Government published A vision for health visiting in Wales. It identifies the role of the health visitor as empowering as well as supporting ‘children, individuals, families and communities to reach and achieve their fullest health and wellbeing potential’1. It acknowledges that, although challenging, continual assessment using a common assessment tool was critical for health visitors. In October 2016, the Welsh Government launched the Healthy Child Wales Programme2 to provide an integrated universal service with targeted interventions for those at greatest need. It listed a minimum set of key interventions, irrespective of need within three key areas: screening, immunisation, and monitoring and supporting child development (surveillance). One of the goals of the Healthy Child Wales programme is ‘to promote positive maternal and family emotional health and resilience’. It states that a family resilience assessment tool and acuity instrument will follow in 2017 to support health visitors in their professional judgement and decision making.
The Royal College of Paediatric and Child Health (RCPCH)14 in 2016 published its child health manifesto for Wales, within which it states that health visitors have a key role to play in tackling child health inequalities. Some families in Wales face immediate challenges to physical and emotional health due to poverty and unemployment. However, some families also face life course challenges because of adverse childhood experiences such as neglect, abuse, domestic violence, growing up with adults who have mental health problems, drugs and alcohol misuse, and incarceration due to crime15. In a country such as Wales, where the worst rates of childhood obesity and smoking during pregnancy in the UK are found, health professionals such as health visitors are challenged to develop and use evidence based measures that identify need and aid a positive use of appropriate interventions14.
The relationship between health visiting and parents has grown to become a process of social action as professionals support parents in their social context and focus on identifying interventions to support them16. The relationship is one of practical advice and guidance on family management. It promotes learning to reduce inequalities, safeguard against any risks identified, and promote strong, stable families17. Health visitors sometimes use assessment tools and scales to assess children’s development as well as the whole family environment setting, to decide whether further support is needed to address areas of concern about the family’s resilience2. Health visitors work closely with multi-agency professionals from health, social work and education sectors to provide this important service and maintain transparency and accurate sharing of information1. This work is especially important as a parent transitions into their new parenting role and affects their child’s future outcomes.
Literature review: Family resilience – what is it?
Family resilience is a multidimensional concept. Simon et al. define family resilience as ‘the ability of a family to respond positively to an adverse situation and emerge from the situation feeling strengthened, more resourceful and more confident than its prior state18’. Bryar (2017) recognises it as a key concept alongside community resilience but acknowledge that health visitors need to pay more attention to their community engagement skills to ensure that they can better connect with families and improve health outcomes for them and their children19.
Striepe (2017) cites Novak and Cañas (2008) and Åhlberg (2004), who state that a concept needs to demonstrate an event or object and can be represented as a word, a symbol, or a short statement20. It is a mental representation that cannot be seen or touched but evolves from experience and reflects the theorist’s educational background21. It may be influenced by a professional’s view of normality that is shaped by cultural norms, professional values and individual experience. One view of family resilience perceives family characteristics as a unit, although it recognises that individuals also have resilient characteristics that interact with each other and the family unit as a whole18. Conflict, challenges, crises and change are very much part of normal family life22. However, there are three key components to family resilience: the length of the family crisis, the life stage within which the crisis is encountered, and the strength and type of external family relationships18. These are especially important when families face developmental (normal transitions) or situational (unexpected) crisis or stress23,24.
Family resilience literature has evolved over three waves25. The first wave explored and developed a number of models set within family stress theory; this led family therapists to conceptualise family resilience, and develop an understanding that resilience was a family characteristic. Werner and Smith’s work is often described as foundational. They started their longitudinal research into child developmental outcomes and vulnerability in 1955, and found that vulnerable children found positive responses from outside of their family relationships if they were lacking within them26. McCubbin and Patterson first introduced the concept of family resilience in 1981 when discussing the family and how it managed stress27.
The second wave defined family resilience as having protective factors (eg adequate housing) and processes at individual, family and community levels, all underpinned by a family system28-30. McCubbin and McCubbin (1996) included a positive outcome by referring to an individual or family system successful adaptation or ‘bounce back’ from stressful situations having experienced growth31. This followed on from work by Patterson (2002) who developed the Family Adjustment and Adaptation Response model which proposed three ways in which a family in crisis would adapt: first, by reducing demands; second, by learning new coping mechanisms; and third, by reinterpreting what was most important to the family28. Walsh (2002) developed a conceptual model with three overarching constructs and subconstructs of ‘family beliefs systems’, ‘organisational patterns’ and ‘communication processes’29. Based on this model, Sixbey developed the Family Resilience Assessment Scale, which has six subscales – ‘family communication and problem solving’, ‘utilizing social and economic resources’, ‘maintaining a positive outlook’, ‘family connectedness’, ‘family spirituality’ and ‘ability to make meaning of adversity’23.
The third wave describes family resilience as a multidisciplinary framework. It acknowledges that a family is an adaptive system that can change when faced with a crisis or risk through multilevel protective factors available to it within its subsystems and interconnected ecosystems25. Resilient families draw on their social resources from other individuals and community support during these times. For example, effective use of networks and healthcare services appears to strengthen a family’s resilience29. Henry, Morris and Harrist (2015) developed the Family Resilience Model and the Family Adaptive System. These include a structure of individual and family relationship patterns and functions that the family fulfils (eg health, education and socioeconomics) and emerging behavioural patterns with rules and social expectations varying from family to family25.
Professionals such as family therapists and certified family life educators25 have led the development of the family resilience literature with input by others from various backgrounds32, but not health visitors. Consequently, the development of the topic’s definitions, models and practical application supports therapist professional practice. Only when professionals understand the concept of family resilience and how it is constructed are they able to use it to assess and prescribe appropriate interventions within their daily practice21. This has implications for choosing the right tool or scale for health visitors to use across Wales. Therefore, consideration was needed of the population who were to use it, and their belief (in this instance) that existing family resilience assessment tools and scales were inadequate for health visiting use in Wales. Previous work by Windle, Bennett and Noyes (2011) had demonstrated that conceptually sound measures of resilience were available for use with adults and youths but not with children under 12 years. Furthermore they should be able to reflect multiple levels of resilience such as individual, family and community33. The purpose of the study reported here was to understand how health visitors perceived ‘family resilience’ and how they constructed it. This would enable them to develop an assessment tool and scale that would support their practice and meet Welsh Government requirements2. Using an appropriate assessment tool and scale would give them the necessary information on which to base their professional judgement when assessing and prescribing interventions and resources to reduce health inequalities, and promote child and family wellbeing.
Methods
GCM offers an integrated participatory mixed methods approach to enable groups of participants to organise and represent their ideas32,34. The study was guided by the need to identify what the health visitors across Wales perceived family resilience to be. Clearly defining the concept is the essential first step in instrument development and is linked to content validity35.
A structured GCM methodology34 using Concept Systems’ Global Max online software was used to complete brainstorming, idea synthesis, idea sorting, idea rating and group analysis36. The online software allowed the researchers to gather information from busy practitioners who were geographically widespread. It gave them an equal opportunity to participate at times and places convenient to them, in short bursts of 20–30 minute activity, and as directed by the research facilitator via email and easy-to-read instructions.
Group Concept Mapping
Trochim (1989) and later Kane and Trochim (2007) described six steps in the GCM process32,34. The first four steps are considered here. They are ‘preparing for concept mapping’, ‘generating ideas’, ‘structuring the statements’ and ‘concept mapping analysis’. Steps 5 and 6, ‘interpreting the maps’ and ‘utilization’, are considered in the results section.
Step 1 – preparing for concept mapping: It was agreed at an All-Wales health visitor meeting in 2014, that family resilience was to be the focus of a universal health visitor assessment tool and scale, and the study team were instructed to conduct this GCM. This study took place between November 2014 and February 2015.
The collaborative and equal relationship between the higher education and practice study team members was a key feature to delivering the study outcomes. The study team had expertise in generic health visitor practice as well as Flying Start provision, health visitor management, All-Wales strategic leadership, higher education specialist community public health provision, and research. Care was given to include diversity in health visitor geographical location and lay membership. A retired health visitor was recruited as the lay member of the study team, to work with the researchers and practitioners to plan, analyse and interpret the research. Health and Care Research Wales believes that this approach makes research more relevant and more likely to impact on practice37. The whole study team met monthly and had responsibility for identifying key participants, content interpretation and utilisation of the concept maps. The trained GCM facilitator (an academic) managed the beginning of the process to clarify expectations. She analysed the data, not offering interpretation but ensuring that the research process was completed appropriately for concept development32,34.
The GCM facilitator worked with the study team to develop and agree the single focus prompt, ‘When assessing a family’s resilience, a specific aspect to look for is …’, and the two rating scales of ‘importance’ and ‘essentialness’. These two rating scales were thought to be most useful 32,34. Sixty two health visitors (representing all of the National Health Service administrative units in Wales) practising in Wales volunteered to participate in this study. In GCM there is no strict limit to the numbers of participants, and groups can range from small (8–15) face-to-face groups to large, web-based networks32,34. The participants in this study used their experiences of working with families when identifying the statements in response to the single focus prompt and the two rating scales from which family resilience was constructed. Once informed consent to participate had been received, each participant was emailed a username and unique password. The participants were also asked to answer four multiple-choice demographic questions (Table 1) to ensure that the study had captured a diverse group of health visitors across Wales. On three separate occasions the GCM study facilitator emailed participants with step-by-step written and visual print-screen instructions on how to navigate the online software while generating, sorting and rating ideas during the research study.
For the 62 unduplicated count of health visitors who enrolled in the study, not all participants completed every step of the brainstorming, sorting and rating. For example, 44 (71%) health visitors completed step 1 (‘brainstorming’), which generated 171 original statements; 41 (66%) health visitors started the sorting and 30 (48%) finished it; 26 (42%) completed rating 1 (importance) and 28 (44%) completed rating 2 (essentialness). Rosas and Kane’s findings demonstrated that 54% of web-based participants completed the sorting, while 68.7% and 48% on average completed ratings 1 and 2 respectively38. Explanation for the differences in completion between this study and those found by Rosas and Kane were thought to be due to this study being conducted over the Christmas and New Year period when staff were trying to juggle both work and holiday time.
Forty eight health visitors completed the study demographic questions. They included health visitor team leaders/managers (30%), practice teachers (33%) and health visitors (37%). They were generally very experienced health visitors, with 70% having practised for 11 years or more. Only 13% worked in the city while the remainder worked in towns and in the country. Sixty three per cent (63%) described their work area as an area of high deprivation (Table 1). The study used a modified version of the Office for National Statistics’ Rural Urban Classification to construct the categories in discussion with the stakeholder group. Health visitors were then asked to self-identify their practice location39. The 2011 rural–urban classification provides a rural/urban view of datasets at output area, super output area and ward level (Fig1).
Table 1: Participant online questions and results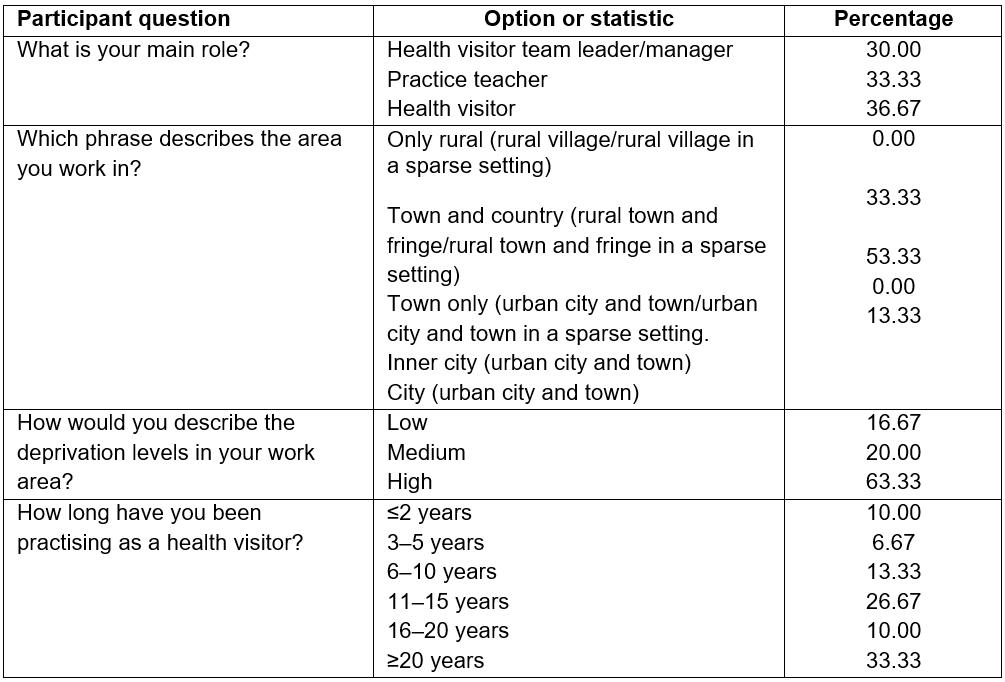
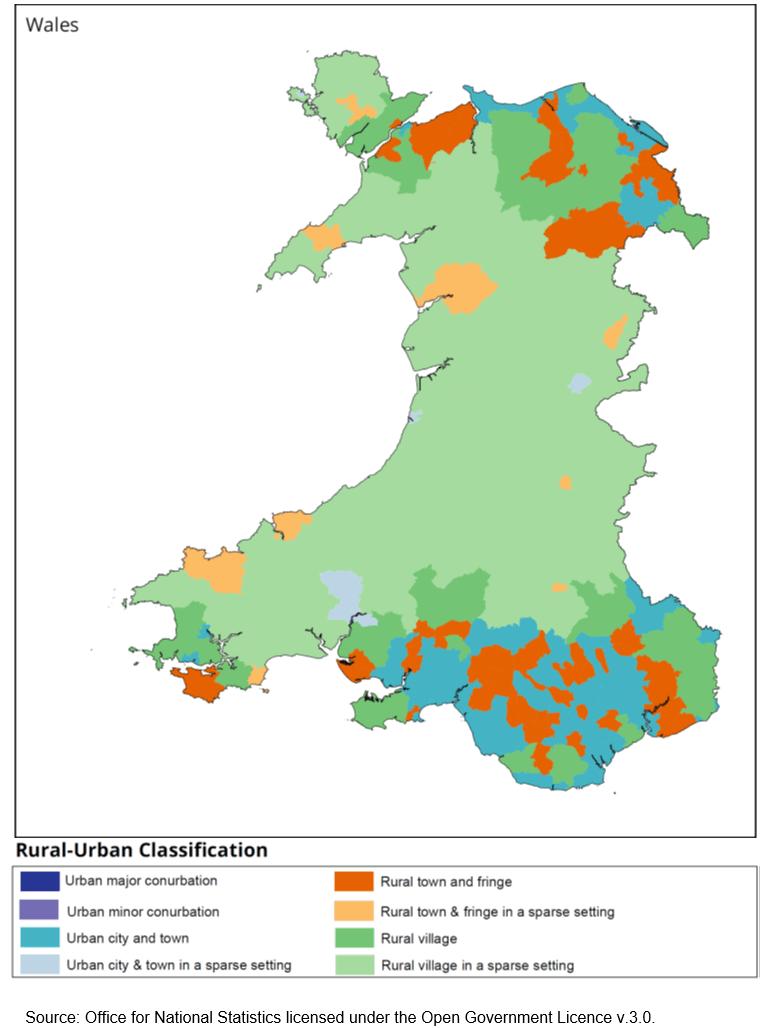 Figure 1: Map of Wales demonstrating rural-urban classification for Middle Layer Super Output Areas, 2011.
Figure 1: Map of Wales demonstrating rural-urban classification for Middle Layer Super Output Areas, 2011.
Step 2 – generating ideas: During this step the participants were asked (via emailed instructions and using the online software) to generate a set of statements using the single focus prompt. Participants were encouraged to generate as many statements as they felt appropriate, and to return to the list as often as needed. Once every participant had completed this step, the study facilitator considered the list of 171 statements. Through a process of content analysis and discussion with the study team members40, replications were removed and similar statements edited to reduce the list to 117 statements without losing content. Although using the online software is likely to yield over 100 statements, it is suggested that the number of statements be reduced to a maximum of 100 to avoid overburdening participants32,34. Rosas and Kane found that the number of statements across studies ranged between 45 and 13238. However, this study team were of the opinion that any further reduction would not be representative of the statement topics developed by the health visitor participants.
Step 3 – structuring statements: First, the participants were asked to undertake two structuring tasks32,34,36. Firstly, they were asked to sort the statements into groups (or piles) using the software’s tabletop sorting screen and then label each of their groups of selected statements. Second, they were asked to rate each statement using the two agreed computer generated scales – one to rate importance, and the other to rate essentialness. For example, rating relatively unimportant (1) to extremely important (5) participants were asked ‘to select whether a statement is considered important or not and should be included within a tool assessing family resilience’. Likewise, using the second rating scale, participants were asked ‘to select whether a statement is considered essential or not, and should be included within a tool assessing family resilience’.
Step 4 – concept mapping analysis: There were four steps to the data analysis, which was completed by using the online software36. First, descriptive statistics were used to analyse the participant responses to some demographic questions about their role, the area where they worked, perceived level of deprivation in work area and length of time participants had practised as a health visitor. This data was used to address questions regarding the geographical location of participants and experience in the profession (Table 1). Second, a similarity matrix was created from the sorted statements and demonstrated the number of health visitors who sorted the statements together. Third, a multidimensional scaling analysis of the similarity matrix created a point map, generating a point for each statement created by the participants on a two-dimension (XY) axis. Fourth, a hierarchical cluster analysis created clusters or groupings of the statements in the form of a cluster map using Ward’s algorithm. This process also included analysing the cluster labels (giving them names) and anchoring analysis, which identified the statement in each cluster that reflected best its actual content32,34,36. Further analysis using cluster rating and pattern matching maps were developed and explored to see if there were any differences between rural town and urban town/city participants, and health visitor and team leader/manager perception of family resilience.
Ethics approval
Ethics approval was given by the University of South Wales, Faculty of Life Science and Education Ethics Panel 31/10/2014, ethics approval number LSE1505E0CW.
Results
Step 5 – interpreting the maps
Following data analysis, a collection of demographic data, lists and maps were collated for a whole study team meeting to consider, interpret and make comment. These included the cleaned list of 117 statements, lists of statements grouped into their computer-generated point map (Fig2), five computer-generated individual cluster maps portraying 10 to 5 clusters only (Figs3,4), a cluster rating map for importance (Fig5), and pattern matches for importance and essentialness between health visitor practitioners and team leader managers (Fig6), and between those who worked in ‘town and country’ or ‘town only and city’ (Fig7) .
The aim of the meeting was to gain a consensus on the number of visual clusters health visitors in Wales would find useful when assessing family resilience. The group process started with a general discussion on the point map and the location of its statements. The point map is a relational map that shows the relationship of each statement to each other when placed on an XY axis (Fig2). Statements most often sorted together are seen closer together on the map, while those sorted less frequently together by the participants are further apart40. The point map (Fig2) demonstrates a stress value of 0.28. The acceptable range is 0.205–0.365 and is considered similar to reliability34. This stress value implies that there is a good relationship between the data input, the matrix of similarities developed from the grouping task and the distance represented on the map34.
The group then discussed how the statements were grouped in clusters together. Although all data are used within the final cluster map, the number of visual clusters decided in the final generated map depended on the visible detail required for the development of the FRAIT and a discussion on the ability of individuals to comfortably memorise chunks of information41. After reviewing a range of five cluster maps starting with 10 clusters (Fig3), the group agreed on a map of five clusters with a range of statements from 13 to 36 (Fig4). The cluster labels were computer generated from the labels given by the participants during step 3. The software generated a list for each cluster for discussion and agreement34,40. The study team agreed on all cluster names with exception of the ‘physical health’ cluster; this was renamed ‘family health’ after reviewing all the statements included within this cluster. Having viewed pattern matching, the study team could see that there were some differences between the health visitor practitioners and their managers’ perception of the importance and essentialness of the five clusters within the family resilience concept (Fig6a,b). Engagement was perceived by health visitor practitioners as more important and essential than team leaders/managers. When the team viewed the pattern matching for importance between those who worked in ‘town and country’ or ‘town only and city’ (Table 1) they observed no relative difference between rural town and country versus urban city and town for the constructs of ‘responsive parenting’, ‘family health’ and ‘family support’. Figure 7a demonstrates in both rank order and slope of the line that there is a relative difference perceived in the importance of socioeconomic factors between the two groups, although in Figure 7b socioeconomic factors are seen as almost equally as essential. The standard Pearson product-moment correlation (r) displayed at the bottom of each pattern matching map shows that the strength of association between the variables in each of the maps is very high42.
Therefore, family resilience was agreed by health visitors in Wales to comprise five clusters: ‘family health’, ‘responsive parenting’, ‘engagement’, ‘family support’ and ‘socioeconomic factors’. Each cluster has an identified number of underpinning statements (Table 2 - example of statements). The cluster ‘responsive parenting’ was rated most important (Table 2, Fig5) and the most essential of all five clusters. Although this latter rating scale does not appear to have been understood by health visitors as well as the importance rating scale, and so little value should be given to its interpretation.
Table 2: Example of family resilience cluster statements as defined by health visitors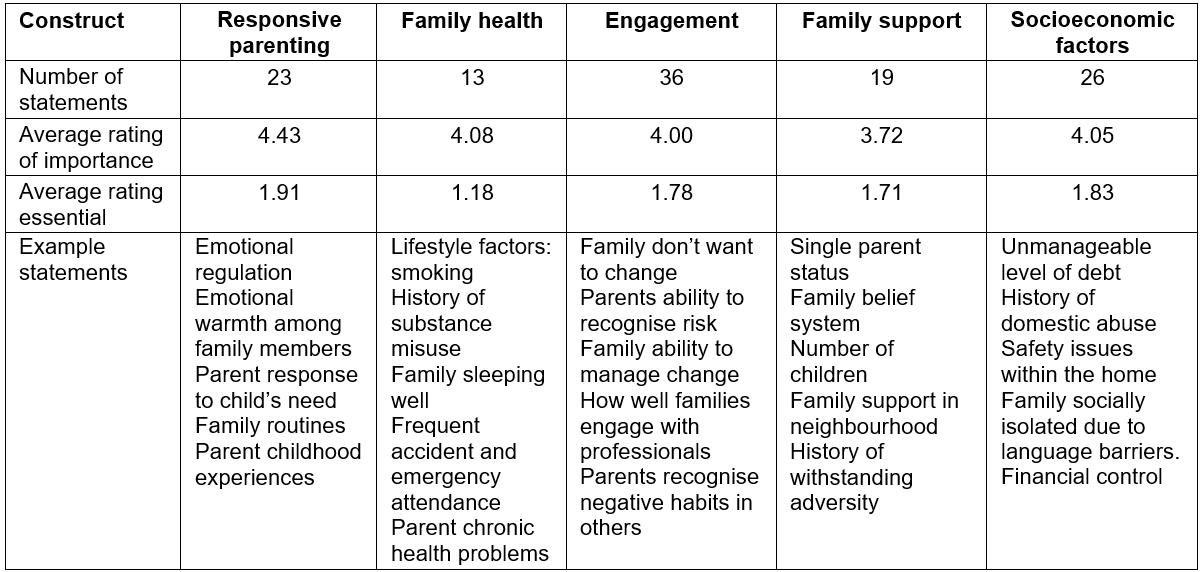
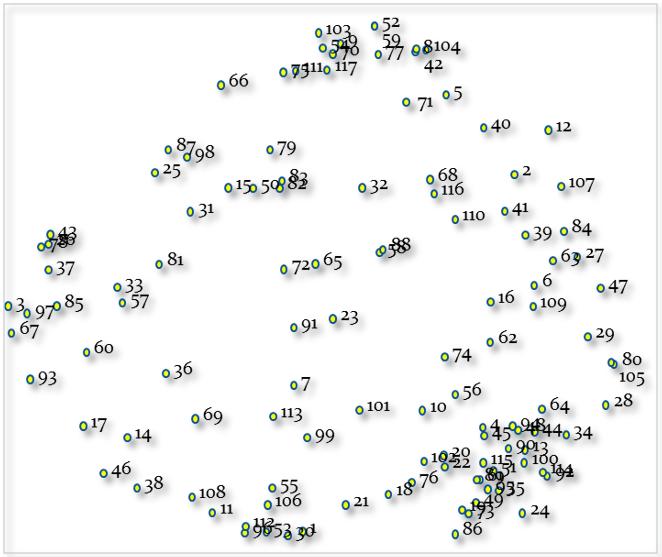 Figure 2: Computer-generated point map of 117 statements with stress value of 0.28.
Figure 2: Computer-generated point map of 117 statements with stress value of 0.28.
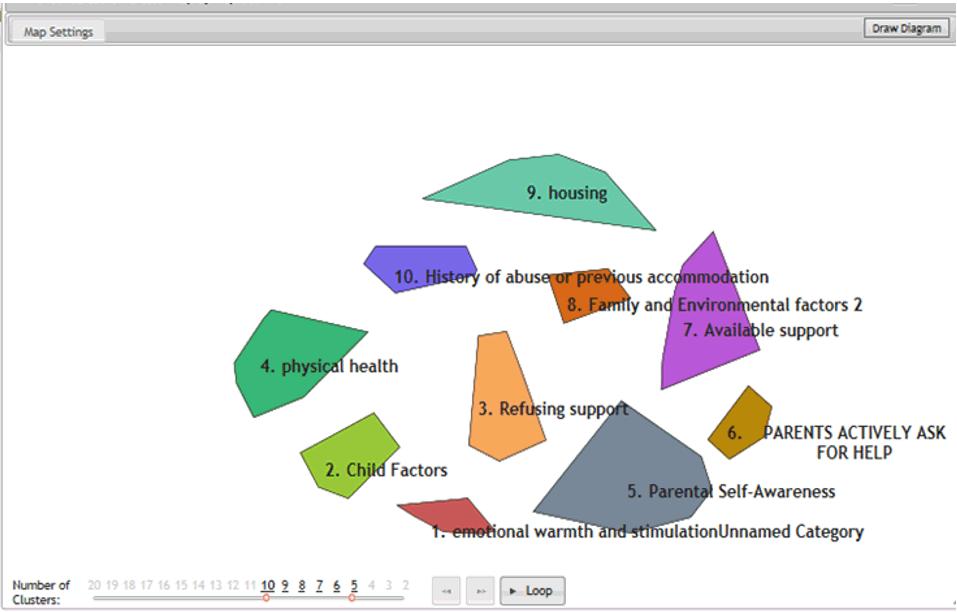 Figure 3: Example of an early map of 10 clusters.
Figure 3: Example of an early map of 10 clusters.
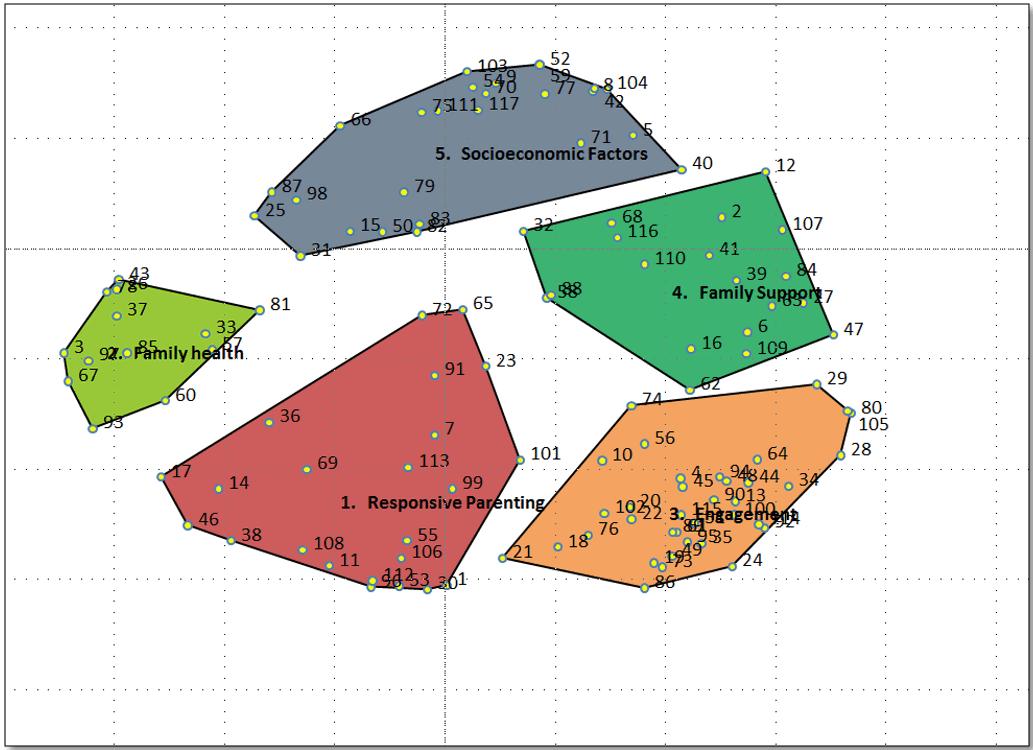 Figure 4: Family resilience cluster map. Each cluster includes their specific statement numbers. Conceptual relationship between clusters is shown by distance between one another.
Figure 4: Family resilience cluster map. Each cluster includes their specific statement numbers. Conceptual relationship between clusters is shown by distance between one another.
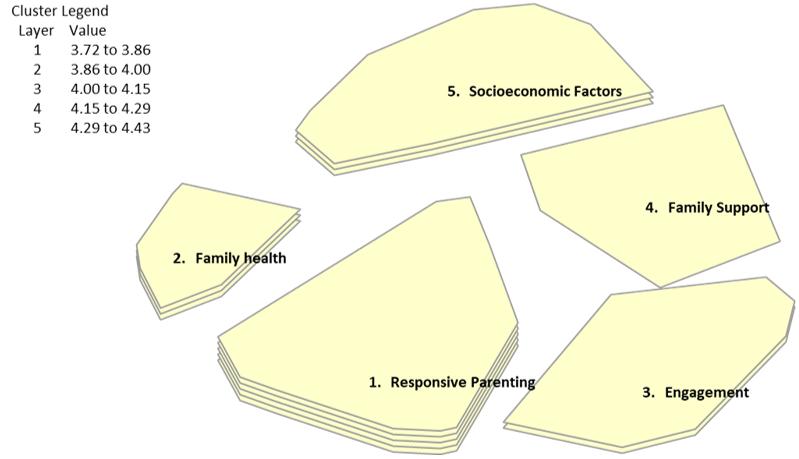 Figure 5: Cluster rating map, ‘importance’, demonstrating ‘responsive parenting’ as the most important of all five clusters.
Figure 5: Cluster rating map, ‘importance’, demonstrating ‘responsive parenting’ as the most important of all five clusters.
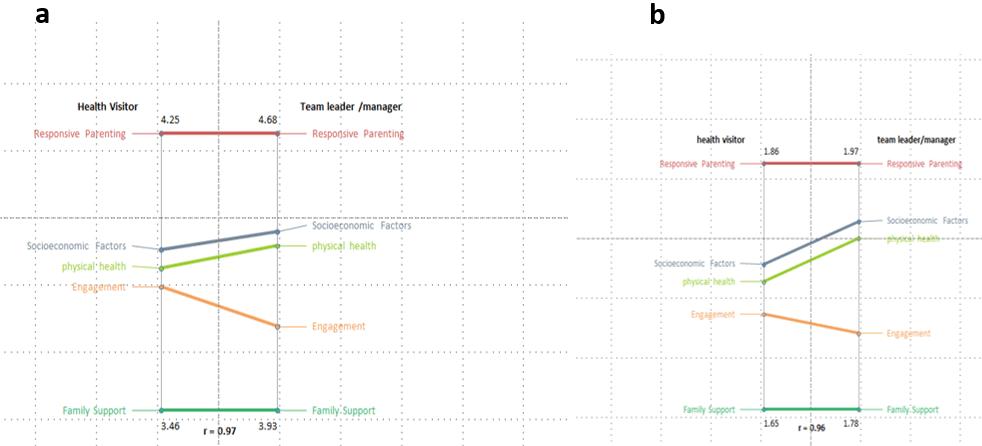 Figure 6: Pattern matching health visitor versus team leader/manager rating of the five clusters in accordance with (a) importance and (b) essentialness.
Figure 6: Pattern matching health visitor versus team leader/manager rating of the five clusters in accordance with (a) importance and (b) essentialness.
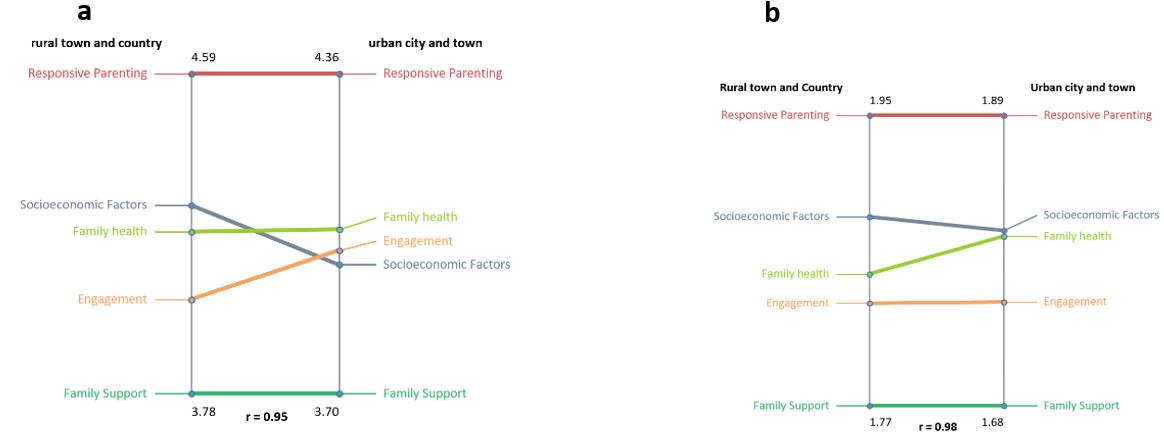 Figure 7: Pattern matching rural town and country versus urban city and town participant rating of the five clusters in accordance with (a) importance and (b) essentialness.
Figure 7: Pattern matching rural town and country versus urban city and town participant rating of the five clusters in accordance with (a) importance and (b) essentialness.
Step 6 – utilization
Kane and Trochim suggest that this stage is for group discussion on how the final concept maps will be used34. Influencing this discussion was both the new Welsh Government Wellbeing and Future Generations Act 201543, which places a wellbeing duty on public bodies to deliver ‘a resilient Wales’, and the impending Welsh Government requirements in the Healthy Child Wales Programme2. Consequently, the team agreed to develop a new family resilience assessment tool for health visitors to use in their daily practice, in addition to an instrument that would measure family resilience. Collectively these new products are known as FRAIT.
GCM is an integrated participatory method, therefore the agreed study team interpretation of the new concept map of health visitors’ perception of family resilience was emailed to all health visitor participants to ask for comments. They were asked whether or not the findings were consistent with their understanding of family resilience, and whether they would support the development of the new FRAIT in a second study. No differences in perception were identified between the study team and the participants, and the health visitors across Wales gave their support for the next stage of the study, where this concept was later tested in a high-fidelity simulation suite and in practice.
Discussion
This new concept map of family resilience offers an original contribution to the international literature as it reflects the theoretical and practice background of health visitor participants as opposed to family therapists and certified family life educators. Researchers have in the past agreed that the concept of family resilience has multidimensional constructs but they vary in their descriptions and content18,25,29. The study team takes the position that it is not only the individual resilient characteristics of the family members that are important but also the resilience of the family as a single unit because as individuals their resilience is socially interdependent (ie each individual’s resilience is affected by their own and others within the family unit) 44,45. The level of connectedness of the family members increases the resilience within the family. Health visitors can promote practices that will increase this connectedness, for example modelling communication strategies through baby massage, promoting shared meal times and shared family time.
The health visitors in this study identified five key constructs within the concept of family resilience: ‘family health’, ‘responsive parenting’, ‘engagement’, ‘family support’ and ‘socioeconomic factors’. Understanding the concept map and the statement/cluster interrelationships has enabled health visitors to underpin the development of the FRAIT. The study team (using the concept map and its data) have produced and validated a family assessment tool and an instrument to support health visitor managers and public health service planners to identify resilient cases across wide defined areas. This will help them to develop and understand geographical characteristics in this context. The underpinning statements consider both individual and family strengths, resources and concerns in a bid to acknowledge and enable productive positive behaviours. In this way it supports the four principles that underpin health visiting practice: the search for health needs, the stimulation of an awareness of health needs, the influence on policies affecting health and the facilitation of health-enhancing activities46.
The ‘family health’ cluster was the smallest identified within the health visitor concept of family resilience. It comprised 13 statements with child, parental, learning difficulties, accident and emergency attendance, lifestyle or chronic illness characteristics. The lifestyle factors include sleeping, eating, exercise, smoking, alcohol and substance misuse. Chronic ill health includes physical and mental health. However, the RCPCH report14 states that, although child health has improved in the past 10–20 years, health inequalities are severe and chronic illnesses such as asthma and lifestyle choices are linked with deprivation. For example, one in five children in their first year in primary school in England, Scotland or Wales were overweight or obese and they were most likely living in the most deprived areas.
The ‘responsive parenting’ cluster was considered by health visitors as the most important construct of family resilience with an average rating of 4.43 and the most essential rating of 1.91. It comprised 23 statements which included child or parental experiences, such as good parenting, responses to cues, family routines, coping and ability to adapt, risk factors, emotion, self-esteem and attending to needs. It acknowledged that families adapt in various ways (eg roles and function) to cope with daily challenges and family crisis22.
‘Engagement’ was the largest cluster of family resilience, with 36 statements, with an average health visitor participant importance rating of 4.0 and an essentialness rating of 1.78. It comprised parental ability to engage with others in their community, family and services, parental recognition of dysfunction in others and weakness in themselves, positive change and ability to change, problems and promptness around decision making. Parents who are able to communicate and adapt to their child’s needs tend to provide the right environment for their children to build secure relationships; this promotes emotional stability and resilience in later life47.
The ‘family support’ construct of family resilience comprised 19 characteristics and included statements about relationships, parental status and age, family belief system, family structure, family communication, accessibility, number of children and history of withstanding adversity. Health visitor participants considered this construct the least important of all five clusters, at 3.72. Educating children and families about respectful and healthy relationships is important to reduce the risk of abuse14. It is reliant upon the therapeutic working relationships and engagements with the services put in place to support families or provide these interventions.
The ‘socioeconomic factors’ construct of family resilience comprised finances including managing a stable income, debt, housing (including its quality, safety and stability), abuse, statutory care experiences, work status, deprivation, education, ethnicity, crime, isolation and cultural diversity. It comprised 26 statements, and health visitors generally rated it the second most important cluster (4.05) when assessing a family’s resilience. Although when pattern matching it against the two variables of participants working in rural town and country versus urban city and town, there was a difference in perception of importance only. Socioeconomic factors such as the level of household income are strongly related to a child’s long-term outcomes such as poor cognitive development, social-behavioural development, ill health and risk of death. The severity of such outcomes are worse the longer the child lives in poverty. In the UK, the proportion of children and young people living in relative poverty based on ‘before housing costs’ was 19% in 2014/15. Considering the ‘after housing costs’, this rose to 29% in 2014/15, which is the same figure as found in 2002/0314. These figures equate approximately to one in three children living in relative poverty due to rising essential housing costs. In Wales (as in Northern Ireland) the proportion of children living in relative poverty is greater than that in England and Scotland due to the greater levels of unemployment.
Conclusion
Family resilience as understood by health visitors is a multidimensional concept. Using an integrated participatory mixed methods approach with an online software package such as Concept Systems’ GCM enabled health visitors working across Wales to achieve a consensus, generate a concept map of family resilience and agree a way forward for future utilisation of the data. Study limitations were primarily due to the time of year that the study was conducted (December and January), a time when staff were juggling work and holiday commitments. Consequently the team relied on participant goodwill and their extensive networks to boost participation.
Family resilience was agreed by health visitors in Wales to comprise five clusters: ‘family health’, ‘responsive parenting’, ‘engagement’, ‘family support’ and ‘socioeconomic factors’. In total there were 117 statements generated and underpinning the five clusters of family resilience. This data was developed in preparation for building a family resilience assessment tool and instrument for use in health visitor daily practice as required by Welsh Government policy. The concept map was subject to further testing during tool development and validation within a high-fidelity simulation suite on two occasions and in practice with health visitors between 2015 and 2017.
Acknowledgements
Funding in costs and kind has been provided by PRIME Centre Wales, University of South Wales, Abertawe Bro Morgannwg, Aneurin Bevan and Cwm Taf University Health Boards; and the Welsh Government. Thanks to Dr Sue Thomas who was an RCBCWales (Building Research Capacity for Nursing & Allied Health Professionals and Pharmacists) funded PhD student at the time of the study and provided advice on aspects of the method.
