Introduction
The three territories in Canada’s north – Yukon, the Northwest Territories (NWT) and Nunavut – are characterized by a small population scattered over many small communities and separated by long distances over a large area (Fig1). Demographically they are very different from the rest of Canada as Indigenous people constitute a majority or significant minority of the population – 25% in Yukon, 50% in NWT and 85% in Nunavut. The healthcare system serving Canada’s north faces many challenges, despite a much higher level of per capita health expenditures1,2. In the remote communities, primary care is provided by nurses, with clinical support by physicians based in the regional centers through the transportation and communication system3. The transportation of patients to secondary and tertiary care centers – both urgent and non-urgent – is a key component of the healthcare system, which is very costly, not just economically, but also socially in terms of the separation of patients from their families and communities.
This study examines the patterns, costs and providers’ perspectives on patient transportation, with a particular focus on emergency evacuations by air (‘medevacs’) in the NWT and Nunavut.
All territorial residents are eligible to obtain medically necessary and appropriate but locally unavailable health services in another community or outside the territory, as a benefit under the territorial healthcare plans. The operating principle is that the cost of travel should not pose an economic barrier to healthcare accessibility. Some residents, such as Indigenous people, injured workers, public servants and the federal police, are covered under other benefits schemes.
The term ‘medical travel’ is used by the territorial governments to refer to the transportation of patients and their accompanying escorts, usually family members, but excluding the medical, nursing and paramedical personnel providing care en route.
Non-urgent medical travel takes a variety of forms: scheduled flights in commercial airlines; air charter to serve communities with no scheduled air or ground transport, or when a large number of people are needed to be transported; and various ground options such as land ambulance, bus, taxi and the patients’ own vehicles.
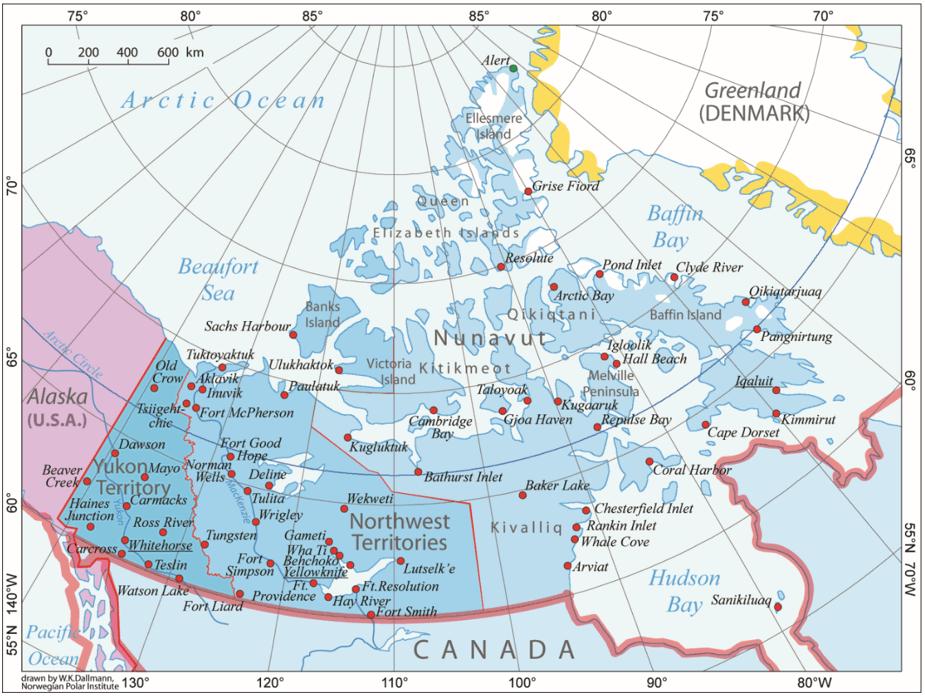 Figure 1: Map of Canada’s three northern territories.
Figure 1: Map of Canada’s three northern territories.
Methods
A variety of databases were accessed. Population data for each community in the three territories were obtained from Statistics Canada4. The mean of the 2011 and 2016 census counts constitutes the mean population for the study period. The distances by road (where available) and by air between each community and the nearest hospital were computed by the Canada Distance Calculator online5.
Medical travel data were provided by the health departments of Nunavut and NWT, covering the 5-year period from the year 2011/12 to 2015/16. The anonymized dataset included date, origin and destination of each trip, category (medevac and non-medevac), traveler’s status (patient or escort), presumptive diagnostic code and associated travel cost. Limited data on Yukon were retrieved from the Department of Finance’s annual budgetary documents6.
The number of health center visits by community for the years 2011–2015, available for Nunavut only, was obtained from the Nunavut Bureau of Statistics7.
Also conducted was an online survey of 292 nurses and 62 physicians in NWT and Nunavut in 2015 and 2016: The overall survey asked primary care providers about their views of the healthcare system, work environment, scope of practice and clinical support. Analyses of survey questions covering communications regarding patient evacuations between nurses in the communities and physicians in the regional centers are reported here. The survey was designed and implemented in collaboration with the territorial health departments, regional health authorities and the Registered Nurses Association of the Northwest Territories and Nunavut. Due to the fluidity of the healthcare workforce, especially the reliance on short-term placements, and the lack of a reliable sampling frame, the survey cannot be considered as representative of all physicians and nurses who are currently or have recently been employed in the two territories and involved in patient transportation. In total, email invitations were sent to 1246 nurses and 235 physicians, while completed or partially completed responses were received from 287 nurses and 61 physicians, yielding an overall response rate of 24%.
The study was primarily descriptive. Considering only the remote communities that are air-accessible only without road access, correlational analyses were conducted to examine potential factors associated with variation in medevac rates across these communities. It was hypothesized that communities with a larger population, a higher volume of health center visits and located further from the nearest hospital were more likely to generate higher medevac rates.
Ethics approval
This study was approved by the research ethics boards of the University of Toronto (#29362) and the University of Alberta (#53063). Research permits were issued by the territorial licensing agencies of Nunavut and NWT. The use of the medical travel data was covered by data agreements with the two health departments.
Results
Access to hospital care
Table 1 addresses the issue of accessibility to hospital services in the three territories, using distance from the nearest hospital as the measure. Where a community was accessible by both air and road, the air distance was quoted for distances over 100 km, as even where roads were available, travel conditions and the degree of urgency often necessitated the use of aircraft for distances greater than 100 km.
Small hospitals, such as those in Watson Lake (six beds) and Dawson City (six beds) in Yukon, and in Fort Smith (six beds) and Hay River (19 beds) in NWT, were excluded as they offered only limited services. For residents in these communities, distance was based on travel to the ‘next level up’ facility in Whitehorse (55 beds) and Yellowknife (80 beds), respectively. There is only one hospital in Nunavut, in Iqaluit (35 beds), serving mainly the Qikiqtaaluk region in the east. Residents of the Kitikmeot region in the west use the hospital in Yellowknife in NWT. For residents of the central Kivalliq region, the closest hospital is in Churchill, Manitoba (28 beds).
The community located furthest from a hospital in the three territories is Resolute Bay (population 200) in Nunavut, about 1570 km from the hospital in Iqaluit; Norman Wells (population 750) in NWT, 685 km from Yellowknife; and Old Crow (population 230) in Yukon, 795 km from Whitehorse.
Table 1: Distribution (%) of population by distance to nearest hospital in the three territories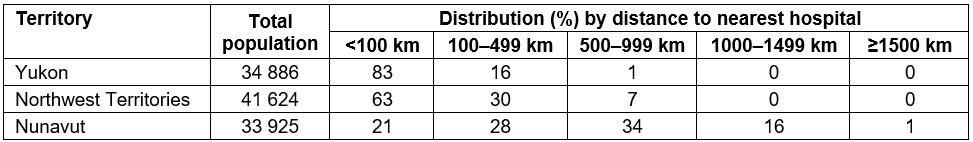
Travel flow patterns
Over the 5-year period, each year there were on average 23 012 medical travel trips in NWT and 21 578 trips in Nunavut, or 525/1000 and 610/1000 residents respectively. Of these 1395 trips in the NWT were medevacs (6%), while there were 1863 medevacs (9%) in Nunavut, at a rate of 32 medevacs per 1000 residents in NWT and 53/1000 in Nunavut. By comparison, in Yukon medevacs accounted for only 3% of all medical travel, at a rate of 0.9/1000 residents.
Figure 2 illustrates the complexity of medevacs within NWT and Nunavut, and outbound trips to higher levels of care in the larger centers in the southern provinces.
Among medevacs during this period, 51% of trips were between communities with only primary care services and regional hospitals in the two territories and the neighboring provinces of Manitoba and Alberta. About 20% of trips were from these intermediate centers to tertiary care, university teaching hospitals in large southern cities such as Ottawa, Winnipeg and Edmonton. Of note is that an equal proportion of trips (20%) were directly between the communities and the teaching hospitals, bypassing the intermediate stops.
The number of health center visits in Nunavut communities was obtained. Between 2 and 14 medevacs occurred for every 1000 patient visits to the health centers.
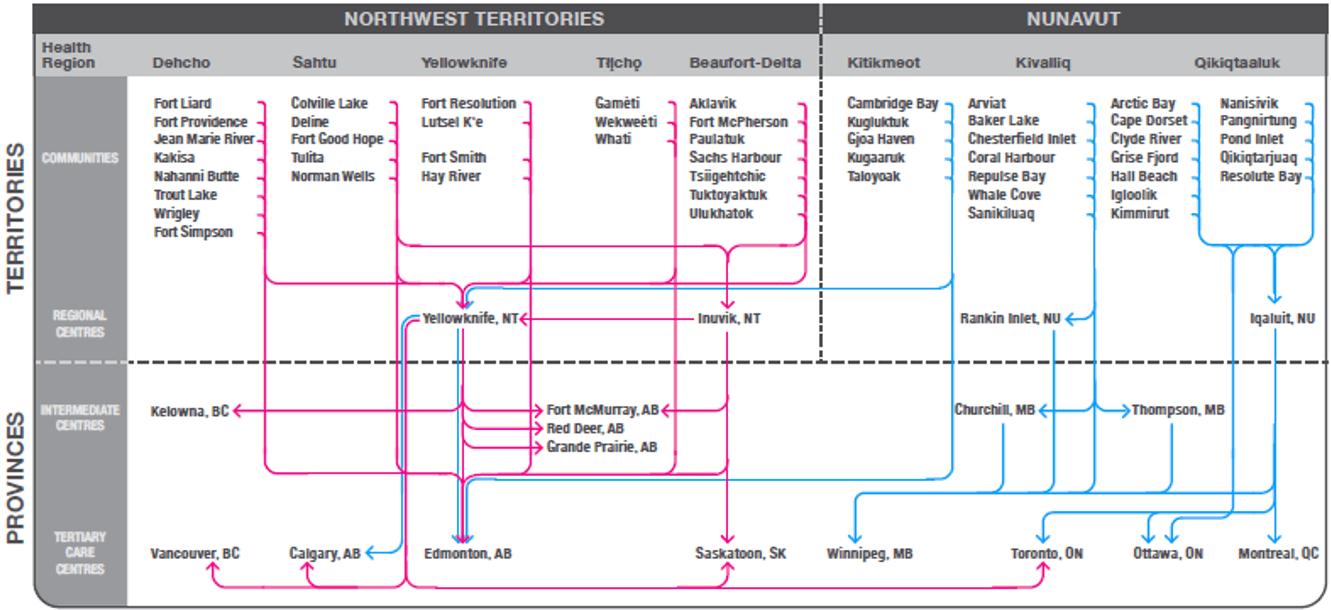 Figure 2: Pattern of patient travel within Northwest Territories and Nunavut, and outbound to southern out-of-territory destinations.
Figure 2: Pattern of patient travel within Northwest Territories and Nunavut, and outbound to southern out-of-territory destinations.
Factors associated with medevac rate
The medevac rate varies considerably among the air-accessible communities served by nurses stationed in community health centers, with some extreme outliers (Fig3).
Potential factors that may be associated with the medevac rate were examined. Distance from nearest hospital was weakly correlated with the medevac rate (r=0.28), whereas population size (r=0.12) and rate of health center visits (r=–0.13) were poorly correlated with the medevac rates.
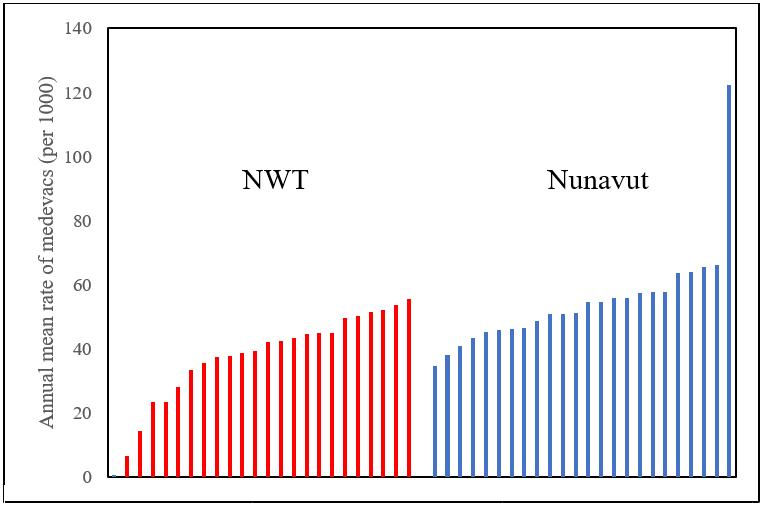 Figure 3: Variation in medevac rate across air-accessible communities in Northwest Territories and Nunavut.
Figure 3: Variation in medevac rate across air-accessible communities in Northwest Territories and Nunavut.
Travel costs
Medical travel is a substantial line item in the health department’s budget, accounting for 4–5% of NWT’s and 18–20% of Nunavut’s budget. (Note that NWT has a combined health and social services department while Nunavut’s is exclusively health.)
The costs of medevacs averaged $9.5 million in NWT and $24.8 million in Nunavut per year, or $218 and $700 per person per year (Fig3). Medevacs accounted for 49% and 35% of the medical travel costs of NWT and Nunavut, respectively. Note that cost data referred to costs directly associated with the flights (airfares or equivalent charges by carriers, meals and accommodation), but did not include program administration or the salary costs of health staff.
Providers’ perspectives
The study focused on the responses of nurses in the communities who sent patients out to regional centers in NWT and Nunavut, and physicians based in these centers who provided clinical advice and, if warranted, approved and accepted the medevacs (Table 2).
Combining those who strongly agreed or agreed with statements regarding acceptable response time, immediate access to clinical advice on patient management and understanding of the nurses’ working conditions, the proportion ranged from 56% to 66%. Fewer than 25% disagreed or strongly disagreed, with about 20% taking a neutral position. Overall the pattern of responses from nurses suggests that there was not a very strong endorsement of the timeliness and quality of clinical advice and support. In terms of acceptance of the nurses’ assessment of a patient’s condition and the need for medevac, there was a higher proportion of positive responses (77%).
At the recipient’s end, only about 50% of the physicians considered the quality of clinical information provided by the nurses during the initial consultation and accompanying the patients to be clear, when the ‘agree’ and ‘strongly agree’ responses were combined. Moreover, close to 80% of physicians regarded the pre-transfer and in-transit preparations as appropriate.
Nurses in the communities were asked to recall the last time they needed clinical advice: on average they made two calls to obtain the advice they required, spoke to two different individuals at the other end, and time from the first call to receiving the required guidance was about 36 minutes. In terms of workload relating to communications between the health centers and regional hospitals, on average nurses made six calls per week, while physicians received 11 calls from the communities.
Table 2: Providers’ perspectives on medevac-related clinical communications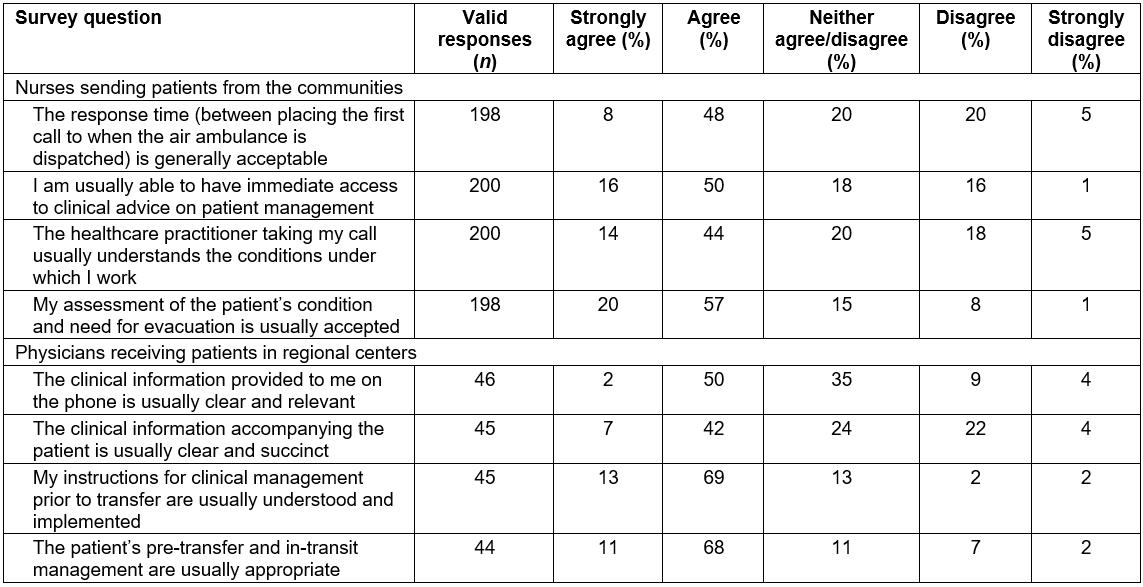
Discussion
In northern Canada, geography and demography impose an organizational structure for healthcare delivery and strongly influence the allocation of human and financial resources. It is not often recognized that a substantial proportion of northerners live in northern cities, and for them health care is not that different from much of southern Canada. Nunavut has the highest proportion of population living in remote communities with longer distances and without road access, and thus reports the highest frequency and costs associated with medevacs.
The ability to drive to a hospital in reality was only available for residents of the cities where the hospitals were located and a few nearby settlements. Over 70% of the population of Yukon resided in Whitehorse, just under 50% of NWT’s population lived in Yellowknife, and Iqaluit accounted for 20% of Nunavut’s population. Residents of Inuvik, NWT, also had local access to the territory’s second largest hospital (51 beds).
For residents of communities that are air-accessible only, distance from the nearest hospital does not fully explain community variation in medevac rates within regions. Other potential factors related to staffing, scheduling, communication, facilities, coordination, disease outbreaks, and human rather than geographical considerations, are likely involved. These factors are separately examined in a qualitative study involving interviews with providers.
Logically, medevacs should flow from the communities to small regional hospitals, and then to teaching hospitals in large urban centers, with assessment and management at each level of care before proceeding to the next level for more complex care. That 20% of medevacs bypassed the intermediate step requires further investigation. They may well be justified if the medical condition of the patient exceeds the capability of the secondary hospital, or weather conditions requires diversion to a larger airport.
Among circumpolar regions, Yukon, with its road access for all but one community, is similar to northern Scandinavia8. Medevacs in NWT and Nunavut face challenges similar to other air-dependent systems serving northern remote regions, such as those linking Greenland and the North Atlantic with northern Europe. These include limited resources, unpredictable weather conditions and long distances separating suitable landing sites9. For patients in the Greenland capital city of Nuuk, where there is a 190-bed hospital, the next level of care is in Reykjavik in Iceland (1420 km) and Copenhagen in Denmark (3530 km). By comparison, the distance between Iqaluit and Ottawa is 2090 km, and between Yellowknife and Edmonton is 990 km.
Patient transportation, especially medevacs, accounts for a substantial component of medical care costs in the north. This is evident from its share of overall territorial government health expenditures, and also in individual episodes of care. In a study of lower respiratory tract infections in infants, transportation accounted for between 18% and 55% of the total cost of hospitalizations in various northern Canadian regions. The costs include all direct healthcare costs incurred both within the north and by tertiary children’s hospitals in the south10. Economic analyses of the role of transportation in hospitalizations from other causes in northern Canada remain to be performed.
Privacy concerns did not permit linking the medical travel databases with healthcare utilization records, which would allow the assessment of patient outcomes post-evacuation, such as whether the transfer had been timely and clinically necessary and appropriate.
The technical, organizational and logistical aspects of patient transportation can be improved11,12. For example, the health department of NWT instituted a new central coordination service for clinical consultations and medevac dispatches in 2015. Ultimately, the system’s performance also depends on how health professionals interact with one another. This is particularly important in a primary care system that is nurse-based. Fostering mutual respect, understanding and trust in clinical communication between the communities and regional centers can be achieved through better staff orientation and training. In addition to ensuring that staff are fully informed of medevac protocols, the healthcare system must also ensure necessary medevacs are not missed or delayed, resulting in adverse patient outcomes.
The authors did not attempt to assess the patients’ views of the medical travel system, especially with regard to medevacs. The NWT Department of Health and Social Services conducts, biennially, a client satisfaction survey at its facilities, but there is no specific focus on medical travel. In a qualitative study involving semi-structured interviews with providers and users five NWT communities in 2014, emergency response and medevacs emerged as a consistent theme among users, with comments that the services provided were ‘challenging’, ‘far from ideal’ and even ‘unacceptable’13. The authors have not systematically searched the regional media or debates in the territorial legislative assemblies, but are aware that individual cases of delays and mismanagement often became highly publicized and politically sensitive issues. A study of the experiences of community members, similar to this study’s survey of providers, on their interactions with different aspects of the medical travel program is the next logical step to fill this important knowledge gap in northern healthcare delivery.
Conclusion
Patient transportation, especially emergency air evacuations, is an essential but costly component of the healthcare system serving Canada’s north. It is the ‘glue’ that binds an extensive network of facilities staffed by different categories of health professionals. While system design is largely dictated by geography, addressing human factors such as interprofessional communication is important for improving the system’s effectiveness. This study is primarily descriptive and it points to additional areas for improved understanding of the performance of the system.
Acknowledgements
The territorial health departments of Nunavut and NWT provided access to the medical travel databases. Both departments, and also the Registered Nurses Association of the Northwest Territories and Nunavut, collaborated in the planning and execution of the online survey of providers.
References
You might also be interested in:
2010 - Obstacles faced by general practitioners in Loreto Department, Peru in pursuing residency training


