Introduction
During recent decades, organ donation and transplantation (ODT) has become a gold standard treatment for many cases of end-stage organ failure. Acceptance of solid organ transplant programs has been improving among different countries, but it is still greatly affected by sociocultural and religious beliefs and attitudes1. Worldwide, the number of people on transplantation waiting lists continues to increase, far exceeding the number of donors and undertaken transplants, which grow at a slower pace2. Besides the direct impact on donor and recipient, ODT also affects families, relatives and society on both sides, making this decision a complex choice3,4. The mismatch between needs and availability of donated organs has increasingly led countries to shift to a presumed consent model, also known as an ‘opt-out’ system of deceased donation, in comparison to the traditional ‘opt-in’ system. There is growing evidence of support of the association between presumed consent and increased donation rates5. Countries with opt-out laws generally have 25–30% higher rates than those requiring explicit consent6.
There are two main variations in how the ‘opt-out’ system is operationalized in each country. Depending on the amount of emphasis placed on relatives’ views and decision-making involvement, a distinction is made between a ‘hard’ and ‘soft’ opt-out system. For example, in Austria, a ‘hard’ version of presumed consent is practiced; transplantation of organs after death is legal, unless there is an individual objection during a person’s lifetime7. In contrast, Spain and Greece have adopted ‘soft’ presumed consent laws, with family members making the final decision about donation, having the right to refuse organ removal8,9.
Nevertheless, transition to an ‘opt-out’ organ procurement system is not sufficient to address the critical imbalance between organ demand and supply. The need to focus on individual and system factors, exploring the impact of behavioral determinants, such as knowledge, attitudes and self-efficacy, has been underscored9-11. Based on Bandura’s social cognitive theory, a key construct that may contribute to understanding the decisions and actions in relation to deceased donation is self-efficacy12. It refers to one’s perceived competence to implement a specific behavior and it is an attribute of people who view hard tasks as something to be conquered, rather than to be avoided. Self-efficacy is regarded as influencing all aspects of behavior, including the acquisition of new behavior. It constitutes one of the most crucial determinants of one’s decision to perform or not to perform a specific behavior by regulating motivation, thought processes and behavioral standards13,14.
Self-efficacy has been examined in relation to the adoption and maintenance of a variety of health behaviors, including weight control, smoking cessation and physical exercise15-18. Emerging research among health professionals in the European Donor Hospital Education Programme (EDHEP) has demonstrated that an increase in the self-efficacy of intensive care staff is significantly related to a decrease in the perceived difficulty of requesting organ donation19. The EDHEP intervention was shown to mostly increase self-efficacy among participants with low baseline scores, while prior experience had a significant effect on both beliefs and perceived difficulty. Two randomized control studies from the Netherlands, based on social cognitive theory, have provided further insight into determinants of registration and donorship via school-based health promotion interventions. Increased self-efficacy of Dutch secondary school students was linked to their intention to register organ donation preference20, whereas a web-based program effectively encouraged lower-educated adolescents to register a well-informed choice about organ donation11. In a study of Japanese college students, the positive impact of self-efficacy on signing intention was further intensified by altruism14.
In spite of emerging interest, little is still known about the role of self-efficacy in relation to an individual’s organ donation awareness, attitudes and behaviors towards donorship within a presumed ‘soft’ opt-out consent system. Within a ‘hard’ system of presumed consent, individuals have the ability to decide whether to opt out and take the actions required. Otherwise, this system of donation in which lack of action leads to presumed consent can produce a lack of public trust21. Similarly, a ‘soft’ system of presumed consent, where relatives make the final decision, can also be problematic and stressful, if no prior discussion has taken place22. Relatives tend to err on the side of caution and are more reluctant to consent to the donation of a relative’s organs, as demonstrated in a 2008 European Union survey23. Within rural settings, primary care clinicians can play an important role as a trusted source of information and credible messenger. Ample opportunities to inform and engage with people in their communities could reinforce organ donation attitudes and actions24,25. It is hypothesized that high self-efficacy could be associated with greater awareness and intention to act – important elements for operationalizing successfully the ‘soft’ opt-out system in rural areas.
The aim of this pilot study was to examine the role of general self-efficacy in relation to knowledge and attitudes towards organ donation among rural primary care patients in Greece, in order to raise awareness and address inertia.
Methods
Setting and sample
A prospective survey within the national health system primary care unit of Alonakia-Kozani in northern Greece, serving approximately 1000 registered patients, was carried out during the year 2014. The area is characterized as semi-rural with a total population of 2000 inhabitants, located approximately 20 km from the closest urban center, with a mainly agricultural economy and a rural lifestyle. Demographic information (age, sex, education, occupation, income and diagnosis of a chronic illness) was collected for recruited primary care attendants.
Instruments
A 12-item ‘Organ donation awareness’ questionnaire was used to assess respondents’ knowledge, attitudes and awareness. It included 10 dichotomous questions from a previously developed questionnaire administered among ethnic groups in the UK26, and two questions (2 and 4) aligned with presumed consent reform from a general-practice-based study in Greece27. Responses across the 12 items showing a favorable intention towards donation (‘yes’ for questions 1, 2, 5, 9 and ‘no’ for questions 3, 4, 6, 7, 8, 10, 11, 12) determine a total score, transforming the tool into a 0–100 scale28,29. A high score suggests a positive intention towards donation. Due to 17 missing responses, there were 22 ‘empty’ cells among a total of 2436 cells. As a result of the extremely low frequency of ‘empty’ cells (0.9%), imputation was performed by alignment with the mode value (prevalent response) of each question. Reliability was estimated according to Kuder-Richardson at 0.667.
The Greek version of the General Self-Efficacy (GSE) Scale30, originally developed in German by Jerusalem and Schwarzer31, was employed. It comprises 10 items designed to assess optimistic self-beliefs to coping with a variety of life difficulties (Table 1). Each item has for responses choices, from ‘not at all true’ (which scores 1) to ‘exactly true’ (which scores 4). The scores for each of the 10 items are added to give a total score of 10–40. A higher score indicates greater self-efficacy. Reliability was estimated according to Cronbach’s α at 0.883.
Table 1: General Self-Efficacy Scale – English version 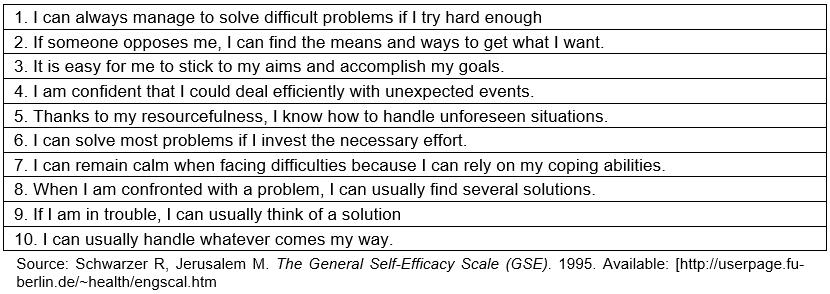
Data collection
Following the same methods as in a previous rural primary care study25, all patients with an appointment for any medical reason were invited to participate. Exclusion criteria were (i) being aged less than 18 years, (ii) seeking urgent care, (ii) having a motor, cognitive, hearing visual or speech disorder, (ii) being too sick and too elderly and (ii) having a severe organ impairment. On appointment day, and upon receiving medical services sought, eligible patients were invited by the general practitioner (GP) to take part in the survey. Once information about the study and assurance regarding confidentiality, anonymity and the voluntary nature of participation had been provided, informed consent was obtained. The GP administered the survey face to face, recorded responses to both questionnaires, and scored the GSE scale.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences software v25 (IBM; http://www.sps.com). Frequency distributions of participant descriptive characteristics were initially evaluated. Response percentages in the ‘Organ donation awareness’ scale were compared with the relevant 95% confidence intervals (95%CIs) as they were estimated, based on bootstrap techniques. Hierarchical modeling of a multiple linear regression model was adopted with GSE scale score added. Due to asymmetry, log10 transformations of the two scale scores were used.
Ethics approval
Ethics approval was obtained from the Institutional Review Board of Kozani General Hospital (#33/2014).
Results
During the 6-week study period, out of a total of 227 patients with a regular appointment, 216 were eligible, with 203 of them participating in the survey (93.9%). If there was no response to a specific item, no answer was recorded. Thus, totals may differ in tables. A respondent profile is shown in Table 2. Overall, the mean age was 54.5 years (standard deviation (SD): 15.8) with the majority being women (136/203, 67%) and 46.3% (94/203) with elementary level education.
As shown in Table 3, about half (51.7%) of respondents had thought about donating their kidneys after death and one-third (34.0%) had discussed presumed consent with a partner, family member or friend. The following positive attitudes about organ donation were reported: (i) most participants (74.9%) were confident that medical teams will try as hard to save the life of a person who had agreed to donate organs, (ii) most agreed (94.1%) that donating organs when you die is a positive act, and (iii) the high frequencies for becoming a live donor if a young child required a kidney (88.7%) or if an adult required a kidney (66.5%).
Negative attitudes about organ donation were captured as follows: (i) 36.9% expressed their opposition to a system that made it lawful to take kidneys from an adult who had just died, if the person had not forbidden it while alive, (i) about one-quarter (27.6%) intended to carry out their right to prohibit the removal of their organs upon death, (iii) 19.7% expressed worries about possible kidney removal after death; (iv) more than half (54.2%) were worried that donated organs might be used without consent for other purposes, such as medical research. Finally, 29.6% found organ donation unacceptable because of religious beliefs and verbalized the necessity of an intact body after death.
Table 4 presents descriptive measurements of the ‘Organ donation awareness’ questionnaire and the GSE scores. Their mean levels were estimated as 58.5±19.7 and 27.8±5.7, respectively, with small and negative asymmetry and questionable-to-acceptable reliability. Table 5 shows that the ‘Organ donation awareness’ score in both models was not influenced significantly by respondent characteristics such as sex, age, education, occupation, income and morbidity (p>0.05). However, it was positively significantly related to the GSE scale score (β=0.155, p=0.033).
Table 2: Participant profile (n=203)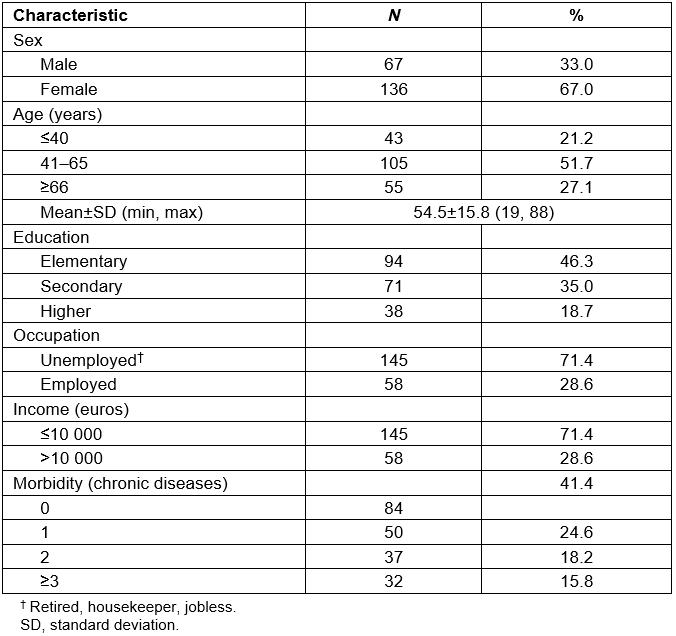
Table 3: ‘Organ donation awareness’ questionnaire responses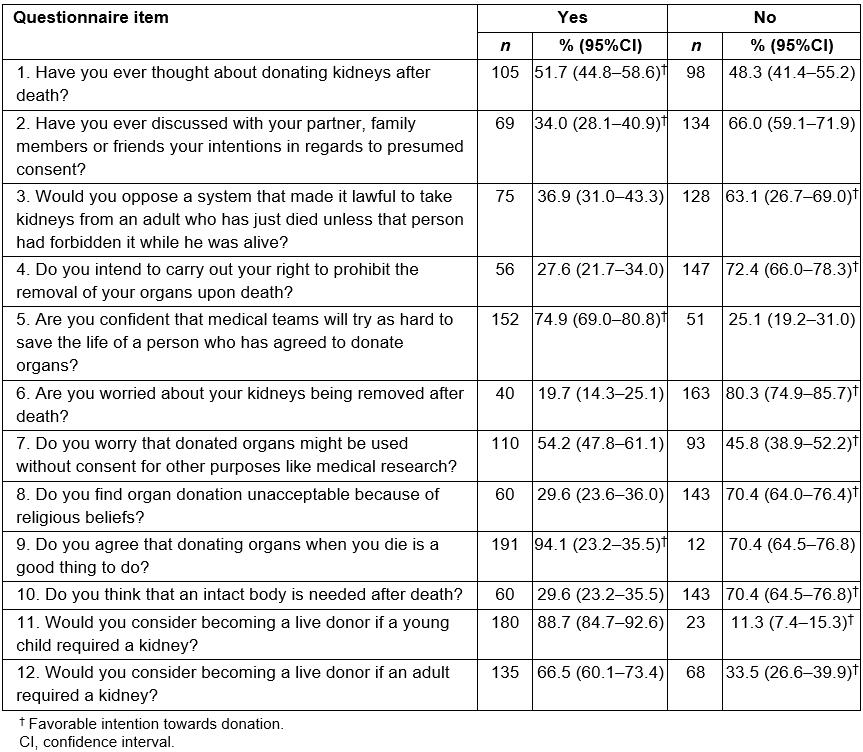
Table 4: Descriptive measurements of ‘Organ donation awareness’ questionnaire and General Self-Efficacy Scale scores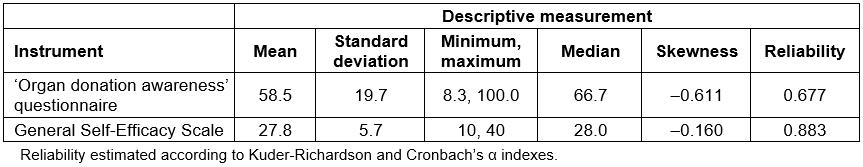
Table 5: Hierarchical multiple linear regression analysis of ‘Organ donation awareness’ score with General Self-Efficacy Scale score 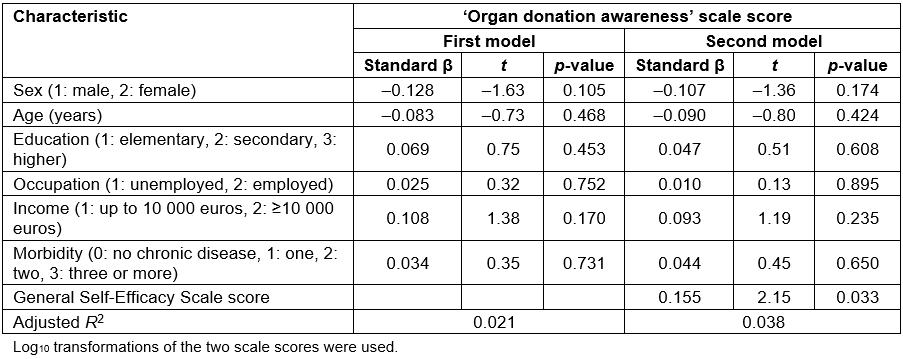
Discussion
This pilot study attempts to explain awareness and attitudes towards organ donation by exploring general self-efficacy. It is one of the few efforts, within a ‘soft’ opt-out system, to trace the donor profile among individuals who are positively predisposed to ODT. Study findings showed that about half of the respondents considered becoming organ donors but almost three-quarters had never discussed the topic with someone else, nor taken any further action. Prior studies in Greece, conducted while the informed consent system was in place, revealed inertia as one of the leading obstacles for individual opt-in25,32. Presumed consent legislation, which establishes organ donation as the default, aims to overcome this inherent inertia33. However, the fact that individuals do not register their unwillingness to donate their organs does not mean that they actually consent to be donors. Limited knowledge about organ donation and the opt-out organ procurement system was found to be a contributing factor to reduced participation in organ donation programs. This finding is in agreement with a previous general-practice-based study that showed that inertia and lack of knowledge contribute to low organ donation rates27. Regulation awareness, social interactions (reciprocity), education and age have all been found to affect an individual’s decision to donate as well as to consent for a deceased relative’s organs23.
Interestingly, the vast majority of respondents reported they trusted medical teams in making the necessary efforts to save the life of a prospective donor. Similarly, most respondents were ready to become live organ donors, particularly if the case involved assisting a child in need, and to a lesser extent an adult. Live renal transplantation, based on the voluntary donation of a healthy kidney, exemplifies an altruistic gift with no personal health benefit for the donor34. Yet, the financial impact of live renal donation for individuals living in non-metropolitan areas has affirmed a ‘rural disadvantage’ in relation to testing, hospitalization and surgery for nephrectomy34. Some evidence suggests that altruism intensi%uFB01es the positive impact of self-ef%uFB01cacy on donor signing intention14. In other words, a desire to help others can promote the strength of self-ef%uFB01cacy, which may drive a person to take action. Thus, participants with a higher self-efficacy score could potentially become altruistic organ donors if provided with the required type of support and resources. In view of the increased burden on the country’s national health system and the strained health indicators due to prolonged restrictions35,36, these findings were rather unexpected and promising.
In the present study, negative attitudes were reflected by respondents who viewed organ donation as unacceptable because of religious beliefs. They were worried about their kidneys being removed after death and had not discussed presumed consent with their loved ones. About one-third opposed kidney donation from an adult who had recently died and had not forbidden donation while alive. Self-ef%uFB01cacy has been considered a favorable correlate of donation intention14,20. As a result, people who perceive a behavior as difficult to perform become discouraged and avoid engaging in this behavior. All of this indicates that psychometrically detectable behavioral determinants can influence ODT beliefs and attitudes. As demonstrated in a study among Japanese college students, emotional response from a positively framed message can influence the recipient’s attitude towards organ donation in an accepting manner14. Similarly, altruistic messages can be used in public campaigns to induce positive emotions such as empathy and increase willingness to become a donor. Positive message framing and emotional appeal could be far more effective with targeted recipients, rather than merely rationalizing the message37. In a recent study of prosocial campaign advertising, participants exposed to conceptually matching framing-color pairs exhibited greater self-efficacy than those who were exposed to mismatched pairs38. Furthermore, the influence of the color-framing match on the intention to donate organs was mediated by self-efficacy. Consequently, promoting organ donation should consider the GSE score of a particular group or individuals as a critical driver towards a prosocial campaign. This recommendation is in addition to increasing confidence to donate, cultivating a perception of organ/blood donation, and addressing preferences to donate only to in-group members10.
Remarkably, organ donation awareness and attitude were not influenced by respondent characteristics such as sex, age, education, occupation, income and morbidity. However, both awareness and intention were significantly related to general self-efficacy. Self-efficacy is closely linked with social interactions and motivational interviewing. Social interactions affect an individual’s willingness to donate one’s organs or those of a relative23. The greater the sense of inclusion and support from neighbors, the more likely it is for an individual to reciprocate by donating their organs. A decision to accept postmortem organ donation is a single behavior that does not need to be maintained, in contrast to behaviors that require sustainability (eg dieting, exercise). Thus, self-efficacy becomes crucial at the time of decision-making39. Acceptance to become an organ donor could be further cultivated through informative interventions to raise awareness and discuss openly individual preferences with family and friends. Interventions of this nature could counteract inertia within a ‘soft’ opt-out system, viewed as a lack of making one’s end-of-life wishes known to the family and reaching a mutual understanding about organ donorship. Targeting education initiatives with a positive message framing and emotional appeal on adults with a higher self-efficacy score could motivate them in overcoming inertia40.
Subsequently, through such interventions, the percentage of those opposing because of religious beliefs or fear could be further reduced8.
Strengths and limitations
This is a novel study tracing organ donation willingness and action within the reformed presumed consent system in Greece. Self-efficacy is studied as a favorable cognitive correlate of donation intention within a ’soft’ opt-out environment that is still in its infancy. The study is based on a single rural primary care setting and one cohort of care recipients. Temporal order cannot be established given the non-experimental design and the non-longitudinal nature of data. Designed as survey technique, data collection carried out by the provider GP could have led to a higher participation rate than expected, as well as response bias due to the close relationship between GP and patients. Hence, some degree of social desirability might have affected responses. Researchers relied on participants’ reporting sincerity and recollection of a conversation or action that might have taken place some time ago, without confirming with a family member. Last, there are some inherent methodological pitfalls associated with studies of psychosocial constructs41. They are difficult to operationalize, and health behaviors need to be analyzed in the context of other relevant variables to avoid overestimating the impact of psychosocial variables.
Implications
Findings should be used for service delivery planning at the rural setting, focusing on individuals positively inclined towards ODT. For rural-based primary care physicians and nurses, planning meaningful conversations to explore concerns and intentions of patients and their families surrounding the new opt-out procurement system should build on the holistic approach and training of both groups. Interventions that increase patient awareness (knowledge) of organ donation and patient’s self-efficacy, such as the potential use of motivational interviewing and discussing with family, should be considered. Further research of the relationship between self-efficacy and organ donation intentions and actions is much needed in order to develop effective public and media campaigns tailored towards rural communities operating within a ‘soft’ opt-out system.
Conclusions
Findings from this rural primary care setting show about half of respondents considered becoming organ donors but, almost three-quarters had never discussed the topic with someone else, nor took any further action. Some evidence that the GSE score can influence beliefs and attitudes towards organ donation signals that behavioral determinants of individuals should be considered. The association of self-efficacy with raised awareness could potentially explain the gap between high intent to consent as a donor and subsequent lack of follow-up action. Further comparative research across psychosocial determinants between urban and rural populations is needed.
Acknowledgements
We thank the administrative board and personnel of the involved health care units for facilitating this study.






