Introduction
Children needing speech pathology intervention in rural and remote locations face barriers in accessing services1. The reported barriers to service delivery include transportation issues, long waiting lists and lack of clinicians2. Overall health inequities between rural/remote populations reflect these barriers and are well documented in countries with large rural geographic areas such as Australia and Canada3. Barriers to service delivery are particularly problematic for children with long-term conditions such as childhood apraxia of speech (CAS), a severe speech disorder in which children experience difficulty in forming appropriate motor plans for speech sounds and that is often difficult to treat4.
Current research into the treatment of CAS suggests that treatment is more effective if it is provided intensively5. However, in the reality of clinical practice, particularly within a rural and remote context, it may be challenging for a child with CAS to access services that provide a similar level of treatment intensity6. Furthermore, there are limited evidence based treatment options for CAS, and many clinicians often do not feel prepared enough in their training in providing services for children with CAS7.
The relationship between high levels of treatment intensity and successful motor learning is one of the tenets of the principles of motor learning8. Dynamic temporal and tactile cueing (DTTC) is one of the few evidence based and effective treatment strategies for CAS that utilises the principles9.
Within speech pathology service delivery, many speech language pathologists (SLPs) train parents to provide home-based treatment as a means of overcoming service delivery barriers such as the inability to provide adequately intensive treatment10. A survey of Canadian and Australian SLPs indicated that the majority of SLPs surveyed used parent training to overcome service delivery barriers11. In addition to using parent training to overcoming barriers, several surveys of Australian SLPs have shown that 80–96% of SLPs involve parents in intervention, mainly through the provision of homework12.
Currently there is limited research into the effectiveness in training parents to deliver a structured treatment program for CAS, particularly within the context of a rural/remote location. The only treatment study to date that has explored the effectiveness of training parents to deliver a home-based treatment program for CAS was conducted in an urban location and showed limited effectiveness in using parents to provide treatment13. In that study, parents were trained to use the Rapid Syllable Transition Treatment with their child. In addition to the limited effectiveness, parents also reported many challenges in carrying out the program in the home13. Nonetheless, with research evidence strongly supporting more intensive therapy for best intervention outcomes, documented inequities in rural and remote speech pathology service delivery, the effectiveness and feasibility of training parents to deliver therapy at home for their children with CAS in a rural/remote location needs to be further explored.
One paradigm for exploring how parent-led intervention can affect the therapeutic process is dynamic systems theory (DST)14. DST proposes that development is a result of the bilateral and non-linear interactions that exist between different developmental areas (eg speech and motor development) and between the child and their environment14,15. Various internal (eg neuronal maturation, attention) and external factors (eg parent interactions and the environment) may impact the developmental process to produce long term change. In the case of the current study, a DST lens can be used to see how an exploration of external factors such as the dynamic influence of the parent–child interactions and the child’s social environment may influence the outcome of a parent training program in a rural community.
The present study explored the effectiveness of a parent training program that used DTTC to improve the speech skills of children with CAS living in a remote location, and aimed to answer the following questions:
- Were the parents able to achieve good fidelity with the treatment and be able to complete the required number of treatment sessions?
- What were the parents’ experiences when delivering DTTC?
- Did a parent-delivered DTTC home treatment program lead to increased speech accuracy in words targeted in therapy (target words)?
Methods
The study used sequential mixed methods research design comprising a single case experimental study followed by a qualitative thematic analysis of parent interviews. These methods were selected as appropriate for early trials of new or substantially changed behavioural interventions16.
Community
The research was conducted in a remote Northern Canadian regional centre comprising three closely located communities that had a combined population of less 6000 people17. This tri-community acted as a regional centre for communities that were further north and more remote. There is only a single SLP employed by the local health region to service children of 0–5 years of age within the tri-community and the entire northern region. A single SLP is employed by the education department to service school aged children within the tri-community and the entire northern region.
Participants
Four parent–child dyads participated in the study. One of the dyads was an auntie–nephew combination but for the purposes of this study, all the adults will be referred to as ‘parent’ unless specifically discussing this dyad. (The term ‘auntie’ is used here because it is the culturally relevant term used in the community in which the participants lived. All parents participating were female, so ‘she’ and ‘her’ are used when referring to parents.)
All participants lived within the tri-community. Three of the children lived with their parents and one child, whose auntie completed the study with him, lived with his grandmother. All children had received prior speech therapy from the health SLP at some time in their lives. However, this therapy was not intensive and did not involve any prior parent training related to their speech disorder. Further demographic information is found in Table 1. All names are pseudonyms.
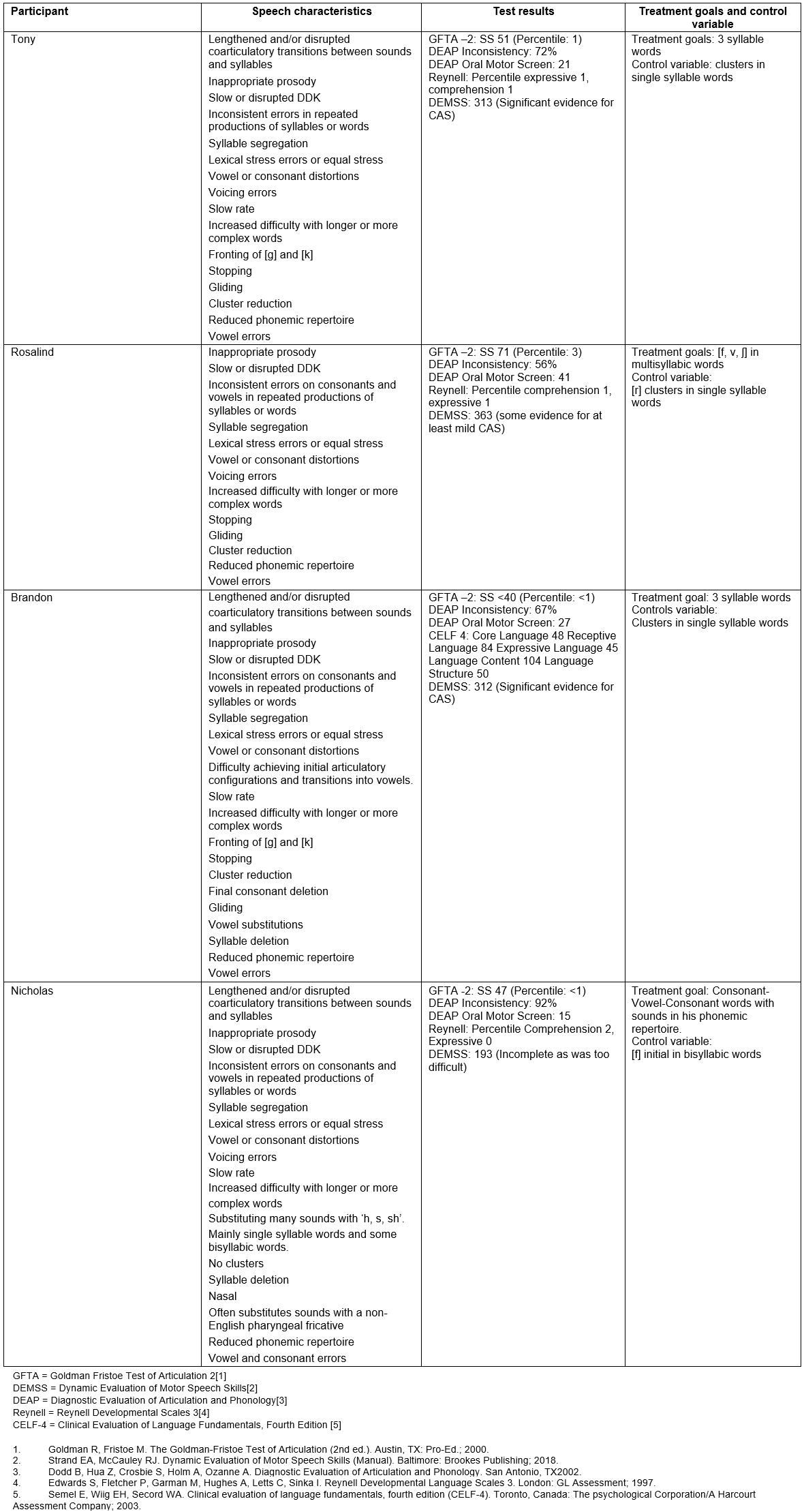
All child participants had a history of speech delay and met the study’s criteria for a diagnosis of CAS (Supplementary table 2). English was their first language and they all passed a hearing screen18 and were not diagnosed with other developmental syndromes. All parents had English as their first language, and none had noticeable speech difficulties.
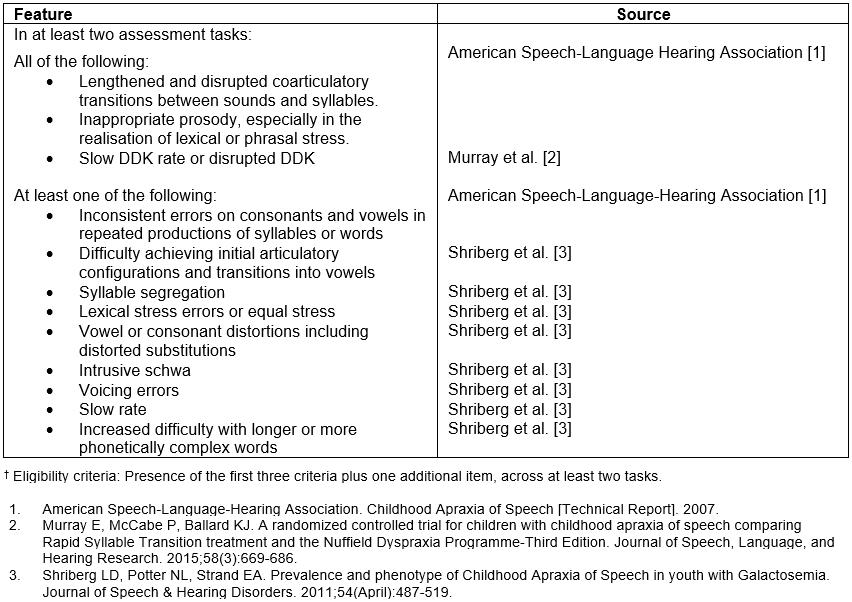
Child participants were recruited via referral from teachers or early intervention workers. There is currently no standardised test for CAS and it is usually diagnosed via the perceptual judgements of experienced clinicians based on a group of core features (Supplementary table 2)19.
Pre-study assessments were used not only to provide a comprehensive profile of participants’ speech to aid not only in diagnosis but also in determining treatment goals. There was unanimous agreement on the diagnosis of CAS and the eligibility of all the participants among all the authors. Participant performance on the pre-test assessments are shown in Supplementary table 1. Four children were tested and all were recruited. Pre-treatment assessments for all the children were conducted at the clinic or at school. Parent training was done in the clinic or at school. Probe data were collected at the clinic, at school, at day care or at home.
Table 1: Participant demographic information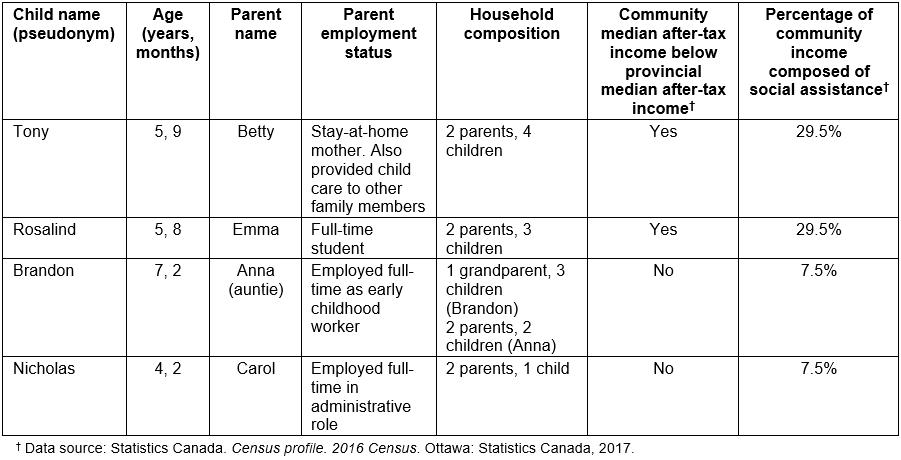
Supplementary table 1: Child pre-treatment assessment results and treatment goals
Supplementary table 2: Core features of childhood apraxia of speech used in present study†
Study design and treatment protocol
The single case experimental component comprised six different phases: baseline, parent training, treatment phase 1, break phase (ie a withdrawal phase), treatment phase 2 and a maintenance phase (Fig1). Each treatment phase targeted a different set of six target words. Individual treatment goals were selected based on the speech profile of each participant and the gaps in their skills. All target words reflected the individual treatment goals of each participant.
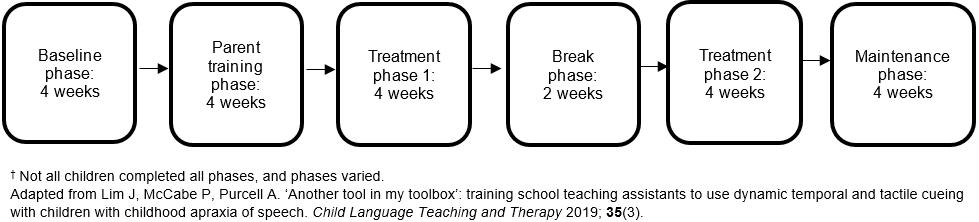 Figure 1: Planned study design from commencement to completion.†
Figure 1: Planned study design from commencement to completion.†
Probe data collection: Probe data were collected during each week of the study across all study phases. Probe words consisted of a minimum of 20 control words, six phase 1 target words, six phase 2 target words and 28 words with similar features to the target words. The control words were also reflective of gaps in skills of participants, but they were not treated in therapy. The similar words had the same features to the target words but were not used in therapy; however, change in similar words would show generalisation of the speech skills and therefore is a measure of efficiency of therapy20. The phase 1 and phase 2 target words were the actual words used in therapy during these two periods.
Due to concerns that probe data for one child (Rosalind) might not accurately represent her speech characteristics, this probe data set was expanded after the first baseline probe to include 25 control words, 33 similar words and 12 target words (six for each treatment phase). Local speakers not connected to the study were video-recorded saying the probe items. Different speakers read the probes for each child.
All probe word video-recordings were inserted into a PowerPoint presentation together with a picture of the word. Each slide consisted of one probe word. Probe words were randomly arranged for each probe session. The child had headphones on with an attached microphone (Sennheiser PC) and placed in front of a laptop. The researcher played the video-recording on each slide and the child was instructed to look at the video and copy what the speaker was saying, and then the screen was changed. The child was video- and audio-recorded throughout the probe session. At the end of the probe session, the researcher and the child played a reward game.
Parent training sessions: Four parent training sessions were spread across a period of 2–6 weeks depending on the child–parent dyad’s circumstances. The first author provided the training to the parents. Each parent training session lasted 1–1.5 hours. Parent training sessions were provided following a staged model of self-directed learning21 where the parent was first provided with information on CAS and DTTC, and then DTTC was demonstrated with increasing opportunities for the parent to practise the strategy with the first researcher (using role-play) and later with the child. Online and offline coaching through the use of video-recordings was provided by the author during practice sessions. Although a structure for the training sessions was outlined, there was some flexibility with its delivery depending on the needs of the parent learner.
At the end of the parent training phase, parents were provided with a DTTC parent manual containing information on CAS, DTTC and the treatment protocol. They were also provided with access to the videos used in the training and some of their video created during the training period, including videos of the role-playing, of the researcher working with the child, and of the parent working with their child. The manual and treatment protocol are available from the first author.
DTTC treatment protocol: DTTC relies on a hierarchy of cues that help support a child to say a targeted word with maximal success22. An outline of the cueing hierarchy used in this study is shown in Figure 2. If a child is unable to respond to the cues provided (eg to copy the parent saying the word or to say the word at the same time as the parent) and does not say the targeted word accurately, then the parent moves down the hierarchy and provides a more supportive cue (eg if the child cannot copy the word in direct imitation, the parent will then provide simultaneous cueing). If the child is able to respond to a cue with an accurate model, then the parent moves up the hierarchy and provides a less supportive cue (eg moving from tactile or gestural cues to a simultaneous and slowed rate of cueing).
A DTTC board game was designed and provided to each parent to help her follow the cueing hierarchy when working with her child. The game provided the parent with instructions of what to do based on the child’s response to the cue. Parents were also instructed to ask the child to repeat a target word three times if they gave a correct response to a cue. If a child made two consecutive errors at one level of the hierarchy, they were given another chance at saying the word with a lower level cue before the parent moved onto another target word. Each target word was written on a card with a picture of that word also on the card. The same picture was used in the probe data presentation.
At the start of each session, parents were asked to shuffle the target words. They were provided with a timer that they could set for 15 minutes and were also provided with short games that they could play with their child periodically throughout the session if their child was having difficulty complying with the tasks. During the two treatment phases, parents were asked to provide treatment at home for 15 minutes twice a day, five days a week. Parents were also provided with an audio-recorder and asked to record the treatment sessions with their child.
Parents were interviewed by the first researcher about their experiences in carrying out the treatment program. Interviews took place either at the parent’s home or at the clinic. No other person was present during the interviews. Personal bias was not able to be avoided during the interview process: the first researcher was already known to the parents because she had already been involved in training them during the study. However, this bias was mitigated during the interview as a set range of questions was asked at each interview. These included what they liked or did not like about the program and the aspects that were easy or difficult. As the interview progressed, other follow-up questions were asked to clarify points that parents made or to elicit more details from them. Parents were given the opportunity at the end of the interview to add any further comments. The semi-structured interviews were audio-recorded and later transcribed by the first researcher. The first researcher kept notes during the interview, and these were compared to the transcription of the audio-recording.
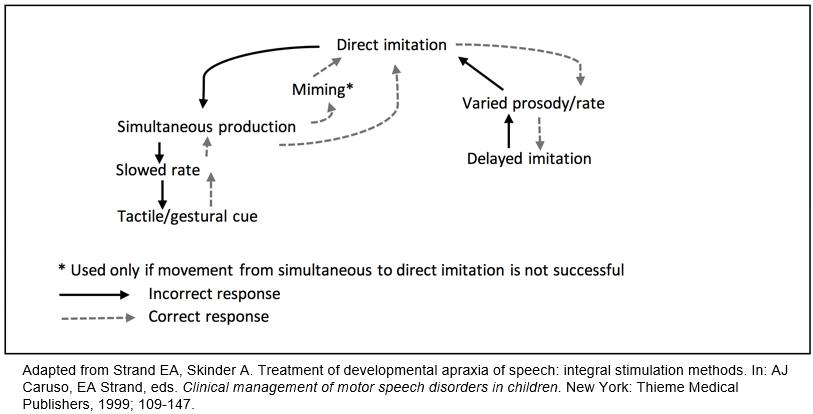 Figure 2: Dynamic temporal and tactile cueing cueing hierarchy.
Figure 2: Dynamic temporal and tactile cueing cueing hierarchy.
Outcome measures
Child measures: The number of speech sounds correct (percentage phonemes correct) was calculated for all words during each probe session. An overall percentage phonemes correct score for each group of probe words was then calculated for each probe session. Effect sizes were calculated using an improvement rate difference (IRD) score for each group of words. The IRD is the number of improved data points for intervention phases versus baseline or non-intervention phases23. An IRD of 50% and below indicates a very small and questionable effect, an IRD between 50% and 70% indicates a moderate effect size and an IRD of greater than 70% indicates a large effect size24. Visual analysis was also conducted to determine treatment effects.
Probe data were transcribed by the first researcher and two speech pathology interns who were trained by the first researcher. Inter- and intra-rater reliability were measured on 20% of the probe data for all data points. The mean intra-rater reliability was 90 (standard deviation (SD)=3.4, range 85–99) and the mean inter-rater reliability was 89 (SD=3.95, range 78–96).
Parent measures: The parent’s ability to carry out home treatment was measured by determining the total number of home treatment sessions that the parent conducted. The parent’s fidelity in using the DTTC treatment protocol was determined by the completion of a checklist by the first researcher to determine the degree of compliance with the DTTC protocol. These were based on audio-recordings of therapy sessions. Parents were rated as ‘yes’ if they were noted to perform a behaviour that was part of the DTTC protocol (eg moving up the hierarchy when the child’s response was judged correct) or ‘no’ if they were not noted to have performed a behaviour when it was appropriate. A fidelity score was obtained by dividing the number of ‘yes’ behaviours by the total number of ‘yes’ and ‘no’ behaviours. A benchmark of 85% was used to indicate a good level of fidelity because this has been used in other parent training studies13.
Qualitative content analysis was used by the first author to analyse the parent interviews25. Each idea communicated by each parent was recorded and then similar ideas were collated. Out of these collated similar ideas, emergent themes were identified and these emergent themes sorted as either representing challenges or benefits of the experience. These themes were then compared across all participants to determine any similarities or differences. The transcripts and themes were then compared by the second author to ensure there were no omissions or misinterpretations. Parents were provided with copies of the transcribed interviews and invited to make any changes. None of the parents requested any changes to the transcripts.
Ethics approval
The research was approved by the University of Sydney Human Research Ethics Committee (2014/924).
Results
Child outcomes
Data for each child are shown in Figures 3a–d and a comparison of their IRDs is shown in Figure 4.
Brandon: Brandon had a slightly altered treatment phase due to personal circumstances. His auntie provided eight sessions at variable time periods across 7 weeks followed by a 3-week break and then four more sessions over 2 weeks. Three weeks of maintenance data were collected after treatment ceased. His auntie was able to treat only one group of words (phase 1 target words). Therefore, probe data were split into target, similar and control words. For simplicity, the two treatment phases were still considered to be separate phases. Although Brandon’s auntie received the same duration of parent training, due to her work commitments, it was spread over six weeks instead of four. See Figure 3a for Brandon’s PPC scores across the study period. IRD calculations indicated that, despite this altered treatment structure, moderate effective change was noted for his target words with an IRD of 57% (Fig4). IRD of control and similar words were both less than 50%, although control words showed greater change than similar words at 49%.
Nicholas: Nicholas’ mother attempted to conduct home treatment for 4 weeks and then chose not to continue with the second 4 weeks. Only 1 week of maintenance data was collected. Consequently, only three word sets were analysed (target words, similar and control words). Although his mother had the same amount of parent training as the other parents, only three probes were collected during the parent training period.
A visual analysis of Nicholas’ probes indicated that there was no treatment effect for his target words (Fig3b). There was an improvement with his target words but at 43% this was not reflected in a treatment effect. However, both target (43%) and similar (46%) words improved to a greater extent than his control words, which only had an IRD of 16% (Fig4).
Tony: Visual analysis indicated that Tony did not show any treatment effect across the study (Fig3c). This is reflected in IRDs less than 50% for all groups of words (Fig4). However, although control, similar and phase 2 target words showed low IRDs, phase 1 target words demonstrated a higher IRD of 46%. This indicated that, like Nicholas, although not demonstrating a high enough effect size to be considered effective, the phase 1 target words showed a greater degree of improvement than the other words.
Rosalind: Visual analysis indicates that Rosalind did not demonstrate any improvement in her target words (Fig3d). As seen in Figure 4, Rosalind did not demonstrate any treatment effect for any words during the study, with IRDs of less than 50% for all word groups (control: 21%; similar: 21%; phase 1 target: 36%; phase 2 target: 12%).
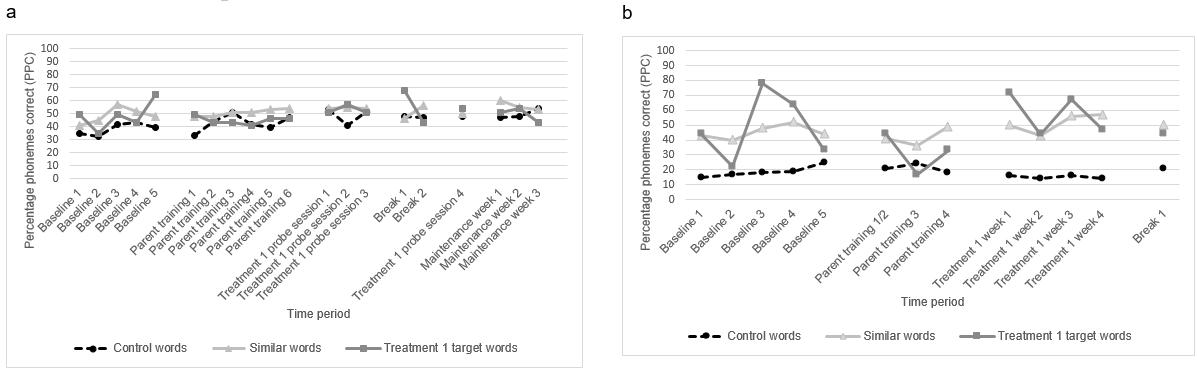
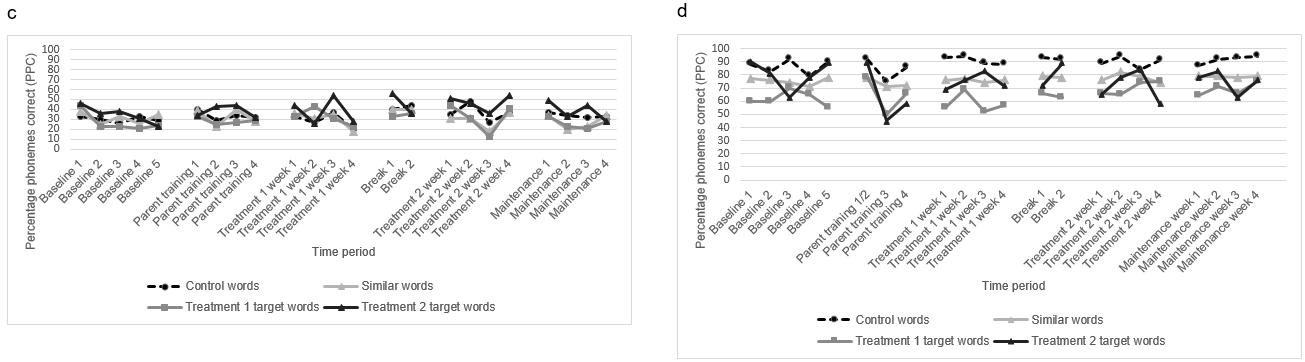 Figure 3: Percentage phoneme correct for all probe words across study period: (a) Brandon, (b) Nicholas, (c) Tony, (d) Rosalind.
Figure 3: Percentage phoneme correct for all probe words across study period: (a) Brandon, (b) Nicholas, (c) Tony, (d) Rosalind.
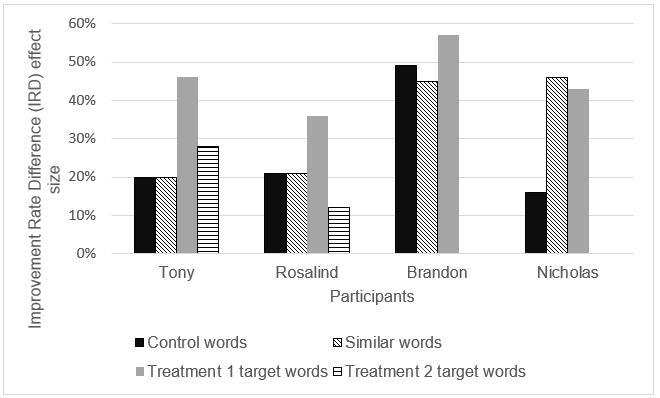 Figure 4: Improvement rate difference scores for all participants for all probe words.
Figure 4: Improvement rate difference scores for all participants for all probe words.
Parent measures
Data for all parents are summarised in Table 2.
Brandon’s auntie (Anna): Anna completed 12 home sessions and had a fidelity score of 82. She had difficulty with tactile cueing and judging Brandon’s responses correctly.
Nicholas’ mother (Carol): Carol completed two home sessions and had the highest fidelity score of 87. She had occasional difficulty moving back down the hierarchy when she judged Nicholas’ speech as correct.
Tony’s mother (Betty): Betty completed 35 sessions and had a fidelity score of 49. She had difficulty using simultaneous or slowed rate cue correctly, combining cues, judging Tony’s responses correctly and providing adequate instructions.
Rosalind’s mother (Emma): Emma completed eight sessions and had a fidelity score of 71. She experienced some difficulty moving up and down the hierarchy correctly, using the criteria to stop cueing and move onto another word, combining cues and judging Rosalind’s responses correctly.
Table 2: Parent outcome measures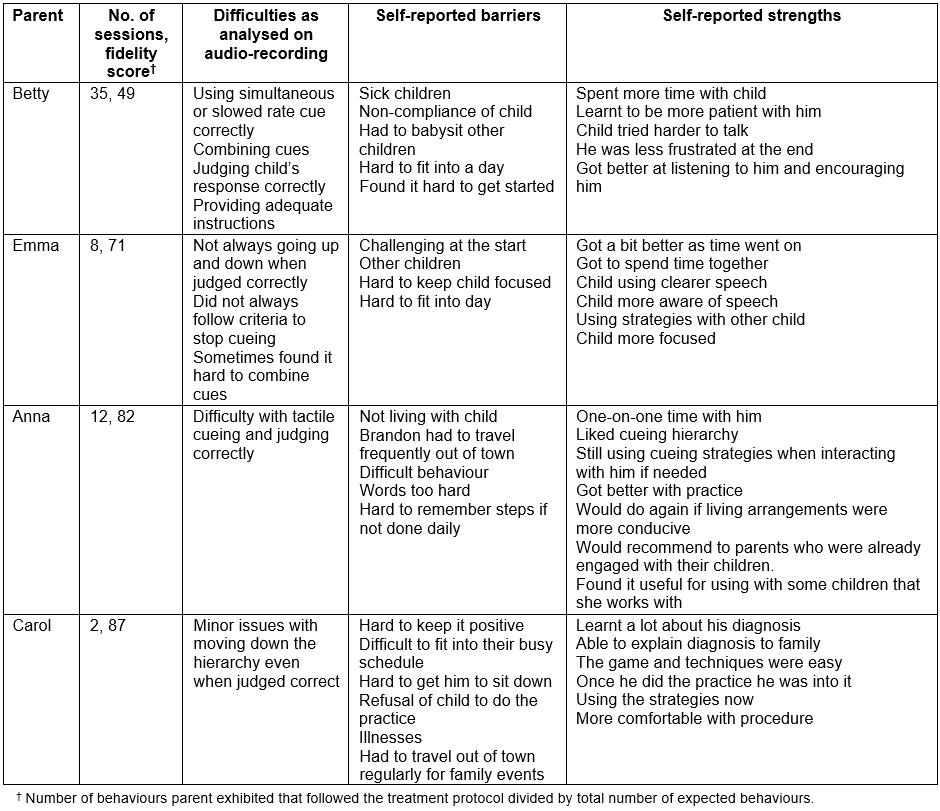
Themes from semi-structured interviews
The themes that emerged from the parent interviews have been divided into either the barriers to completing the therapy program or the benefits of the program. All themes were expressed by all parents during the semi-structured interview.
Barriers: Two themes related to the barriers of delivering the program at home. These were lifestyle challenges and behavioural challenges that the parent faced.
Social challenges: All parents reported difficulty finding the time to complete the program during the day. They often felt that there was not enough time to do the required number of sessions during the day. In particular, the parents living in households where there were other children experienced difficulty in finding either space or uninterrupted time to carry out the therapy. For instance, Betty had to provide child care for other family members due to the lack of childcare options in the tri-community. Emma had to prevent her other children from interrupting the sessions. The parents felt that they had many other household chores and they could not fit the therapy into their day. Emma described this difficulty when she said:
The hard thing was getting into the flow of things. Like having to cooking supper and ‘OK, [Rosalind], come over here.’ I don’t know, its, that part, that part of life, where life got in the way. Where I had to cook supper, but I knew I had to do a, I had to do the DTTC.
Other commitments such as needing to travel out of town for medical appointments or to visit family also interfered in their ability to carry through with the program. As an example, Brandon sometimes was required to travel south to another town to visit his birth mother.
Behavioural challenges: Parents often had to spend time getting their child motivated to do the therapy because non-compliance was frequently an issue. This was despite attempts at developing a reward system to encourage better compliance. In addition, parents often had to manage tantrums from their child during the therapy session or when their child felt that they could not do what was required of them. Emma said, ‘what I found hard was getting her to concentrate’. Anna also found it difficult to manage Brandon’s behaviour, particularly after he returned from visiting his mother:
… it was hard to go over there in the middle of the day when he had a bad day at school and then try and do with him, there was no progress ‘cause he was in his mood ….
Benefits
The two themes that emerged for the benefits of therapy were positive relationship building and development of therapeutic skills.
Positive relationship building: All parents reported finding that the therapy sessions allowed them to spend some quality one-on-one time with their child with CAS. Despite some of the difficulties with compliance, the parents felt that it was a positive experience and allowed them to have fun with their child when they were cooperative and motivated to practice. Betty reported the benefits of this one-to-one time as follows:
I’m spending more time with him trying to help him talk and through his rewards and stuff.
Emma described getting to spend one on one time with Rosalind:
I think we got to spend time together. Me and my girl. Because I’m constantly busy doing this and doing that. So, the time we do get together we cherish it.
Despite Brandon’s challenging behaviour, Anna still found the one-to-one time a positive experience:
‘Cause I got to spend that one on one time with him and we did do activities and stuff and that was good.
Development of skills: The parents all considered that they developed increased confidence in using the cues as the study progressed, and they felt that they were able to use the skills in conversation with their child. As Nicholas’ mother said, ‘we’ll always have the techniques’. The parents felt they could use the cues during normal conversation to help their child be more accurate in their speech production in the moment as opposed to during a structured therapy setting. The parents often found themselves using the cueing during the day with their child. Anna, Brandon’s auntie, found that she was using some of the cues in interactions she was having with other children with unclear speech that she encountered during her work. She also reported that she was using the cues in conversation with Brandon when she did not understand him:
‘Cause when I talk to him and I don’t understand a word that he’s saying, I kind of make him do it slowly. Are you saying this word? And if he says yes, then I’ll repeat the word to him. I’ll say, now you repeat the word. And he says the word back to me and sometimes I do the slow it down.
Some parents also reported that they got better at managing their child’s behaviour as the study progressed. Betty mentioned that she ‘just kept trying after him and getting him to sit still. It took a while, but he eventually got there’. Emma said:
The first two or three session that we had here I was just sweating bullets and really, ‘Oh I don’t think I have the, I don’t think I can do this.’ I had that. But after awhile I started, ‘Ok, alright then. Let’s go do this.’
Betty and Emma reported that as they became more comfortable with managing their child’s behaviour, their child’s compliance improved, and the parents were able to get them to work more effectively. For instance, Betty reported that Tony ‘tried a little harder to talk, he didn’t get as frustrated faster’.
Discussion
This research study aimed to explore the effectiveness of training parents in a rural and remote community to deliver a home treatment program for children with CAS in order to address the lack of adequate speech pathology services. All the parents, no matter their level of fidelity of the treatment protocol, had difficulty carrying out the program due to both social and behavioural challenges. Not surprisingly then, only one of the four children, Brandon, had a moderate treatment effect.
A better understanding of the therapeutic process and the impact of the social and behavioural challenges encountered by the four parents in this study may provide a possible explanation for the lack of treatment effect in three of the children. A DST paradigm can be used to explore these influences on treatment outcomes. DST proposes that development is the result of multiple factors interacting with each other14. Therefore, in understanding why the parent training in the present study was not successful in developing the speech skills of participants, we need to look beyond just the act of therapy and explore the influence of multiple factors on this therapeutic process. For this study, the impact of the parent–child interactions and the influence of social factors on the therapy process were explored.
Parent–child interactions
Several findings from this study highlight how the parent–child interactions impacted the therapy process. For example, the qualitative data from this study suggests that when a parent attempts therapy with a child, the nature of the parent–child relationship may work against providing effective therapy. Thomas et al13 reported similar parental experiences as parents found being a ‘therapist’ with their child particularly difficult and that their child’s behaviour at home was more challenging than during clinician-delivered therapy. Therefore, the dynamic of parent–child relationships may make the implementation of motor-based programs such as DTTC difficult for parents. This may be particularly so if the parent is unused to interacting with the child within the confines of a structured activity such as a DTTC treatment protocol.
The fidelity scores also demonstrate how parent–child interactions impacted treatment outcomes. Anna had one of the highest fidelity scores and Brandon had the highest treatment effect. Carol had the highest fidelity score and while her son Nicholas did not have a significant treatment effect, his target words still showed greater change than his control words. This might suggest that good fidelity of the DTTC protocol (and therefore greater parental skill in delivering the DTTC intervention) may be related to greater change in the children’s target words. It is of interest to note that the two parents who achieved the highest fidelity scores, Anna and Carol, shared some demographic similarities that the other two parents did not. Both were employed full time and had partners who were also employed full time; that is, they were both from households that were more economically secure. Emma and Betty, on the other hand, both came from households that relied largely on social assistance and they lived in social housing. The two high fidelity parents also had some degree of post-secondary education and Anna had experience in working with children at work. Emma was in the process of obtaining her first post-secondary qualification. So, factors such as social economic status, level of education and previous experience may impact the degree to which a parent is able to achieve good fidelity in carrying out a DTTC treatment protocol at home.
Social factors
Exploring therapy within a DST paradigm allows us to situate the therapy process within its social context and explore limiting factors to home therapy. In the present study, conducted in remote Canada, many social factors that existed as a result of the remoteness of the tri-community, such as lack of child care, travel due to geographical distances and overcrowding at home co-existed to create challenges for the parents to engage with the therapy in a consistent way. These factors created an environment that was not conducive to consistent, distraction-free therapy. This causes a dilemma because a strategy such as parent training, which has the potential to circumvent some of the barriers to service delivery that rural and remote clients face, may itself not be an appropriate strategy given the challenging social environment that may exist in such communities. Viewing speech pathology services within their social context may need to be considered by clinicians when deciding on the model of service delivery for their clients. This may be of particular importance in communities where there are societal challenges that may make a home treatment program more difficult to achieve.
Limitations
Given that this study only focused on four parent–child dyads within one rural location, there are limitations on the extent to which the results of the study can be generalised to other children with CAS and other locations. This is further compounded by the fact that two of the four parent–child dyads had truncated or altered treatment timelines; however, it is also possible that this truncation would be replicated in other communities due to equivalent social factors.
It is necessary, therefore, for such research to be conducted in other communities to determine if these results are replicated. This would include both rural and non-rural locations to determine if these challenges are experienced across the board or if rural parents face particular difficulties in implementing home treatment programs.
Further studies also may explore the role of target selection on the success of parent-implemented therapy. For instance, it is possible that the children in this study may have responded better to parent-led therapy if the targets selected were easier or if the goals were more about consolidating newly learnt sounds rather than introducing new sounds.
This study did not explore other possible outcomes such as the development of prosody (also a feature of CAS) or improvements in intelligibility. Therefore, the potential impact of parent-led treatment on these features is unknown.
The existing relationship between the first researcher and the parents may have led to parents to self-select the information they provided in the interview. However, this prior relationship may also have meant that parents felt more comfortable expressing their opinions about the process, particularly the challenges that they faced.
Conclusion
The present study highlights the complexities of training parents to deliver a motor-based treatment program, particularly within the context of a rural/remote community where social factors may create challenges in carrying out a home-based treatment program. The complexities of living in a remote location may make regular and intensive home therapy sessions difficult. The nature of a drill-like program such as DTTC brings the parent–child relationship into somewhat uncharted waters. It may well be that parents are not always the best situated to carry out motor-based therapy with their child. It is possible that other people in a child’s life such as early education workers or school tutors may be better placed to carry out regular and structured therapy programs. Therefore, further research into the efficacy of training other support professionals in a child’s life to provide this therapy is required.
Declaration of interest
The first author was employed in the health region where this research was conducted.