Introduction
Diabetes mellitus is one of the major public health challenges of the 21st century. It is estimated that by 2040, 642 million people in the world will have diabetes, 35% (224 million) of whom will have some form of diabetic retinopathy (DR), and 11% (70 million) will have sight-threatening diabetic retinopathy1-3. DR has been identified as the most common cause of vision loss in working-age adults.
The prevalence rate of diabetes, adjusted for ethnicity, age and gender, in Fijians aged 40 years or more is 41%. Approximately 60% of all diabetics in Fiji are undiagnosed4. Inequities in terms of geographic area have also been identified in Fiji, with those living in rural areas less likely to have their diabetes diagnosed5. This comes with an anticipated increase in the prevalence of DR, a complication of diabetes that affects the eyes. Every person with diabetes is at risk of developing DR, which when left unmanaged leads to permanent blindness. The high number of potentially undiagnosed DR cases and the outstanding barriers to DR management include a lack of appropriate resources in primary health centres, and limited knowledge of primary-level clinicians and community health workers (CHWs) in DR screening, diagnosis and management services6.
To alleviate these issues and address the diabetes continuum, it is important to strengthen the primary and secondary prevention pathways that help identify the disease early, halt its progress and prevent complications. CHWs are identified as the health system’s eyes and ears in communities. They provide a strong continuous link in communities and assist in the extension of health services for the zone nurse or district nurse.
Several studies have demonstrated the benefits of engaging CHWs, particularly in developing countries in delivering numerous public health interventions such as prevention and control of diseases, thereby increasing access and quality of care for underserved populations7-11. For instance, a 6-month training among CHWs in India for the management of diabetes led to a significant reduction in blood glucose levels as well as in blood pressure for the individuals. It also led to greater community engagement, and improved prevention and management efforts9. Similar training in Cambodia also reported the same12. A separate study of CHWs trained in India to screen people for DR showed an increase in uptake of screening by the communities10. In some training of CHWs it has been shown that their effectiveness peaks immediately after training but decreases over time, indicating that CHWs need periodic retraining7.
Studies have also shown that integration of CHWs is critical to enhance the quality of care, improve health outcomes and reduce the cost of care using programs involving CHWs13. A systematic review showed that when CHWs are integrated into health systems they are more effective in addressing health disparities and social determinants of health14,15.
Recognising the important role of CHWs in enhancing primary health care and strengthening referral systems across the levels of health care, the Ministry of Health and Medical Services partnered with the Fred Hollows Foundation New Zealand and the Pacific Eye Institute to roll out 1-day DR awareness training for CHWs across Fiji. The training provided the participants with adequate basic knowledge about diabetes and DR to create awareness of the need for proper diabetes profiling and make prompt referrals for diabetes eye screening, which would eventually reduce avoidable blindness and vision impairment in the Pacific. An outline of the training content is shown in Table 1.
This study seeks to explore the impact of the training on CHWs’ knowledge of DR and its influence on their referral processes, identify challenges faced by CHWs in referrals for DR screening, and their integration within the health system 2 years post-training.
Table 1: Content of 1-day diabetic retinopathy awareness training program for community health workers in Fiji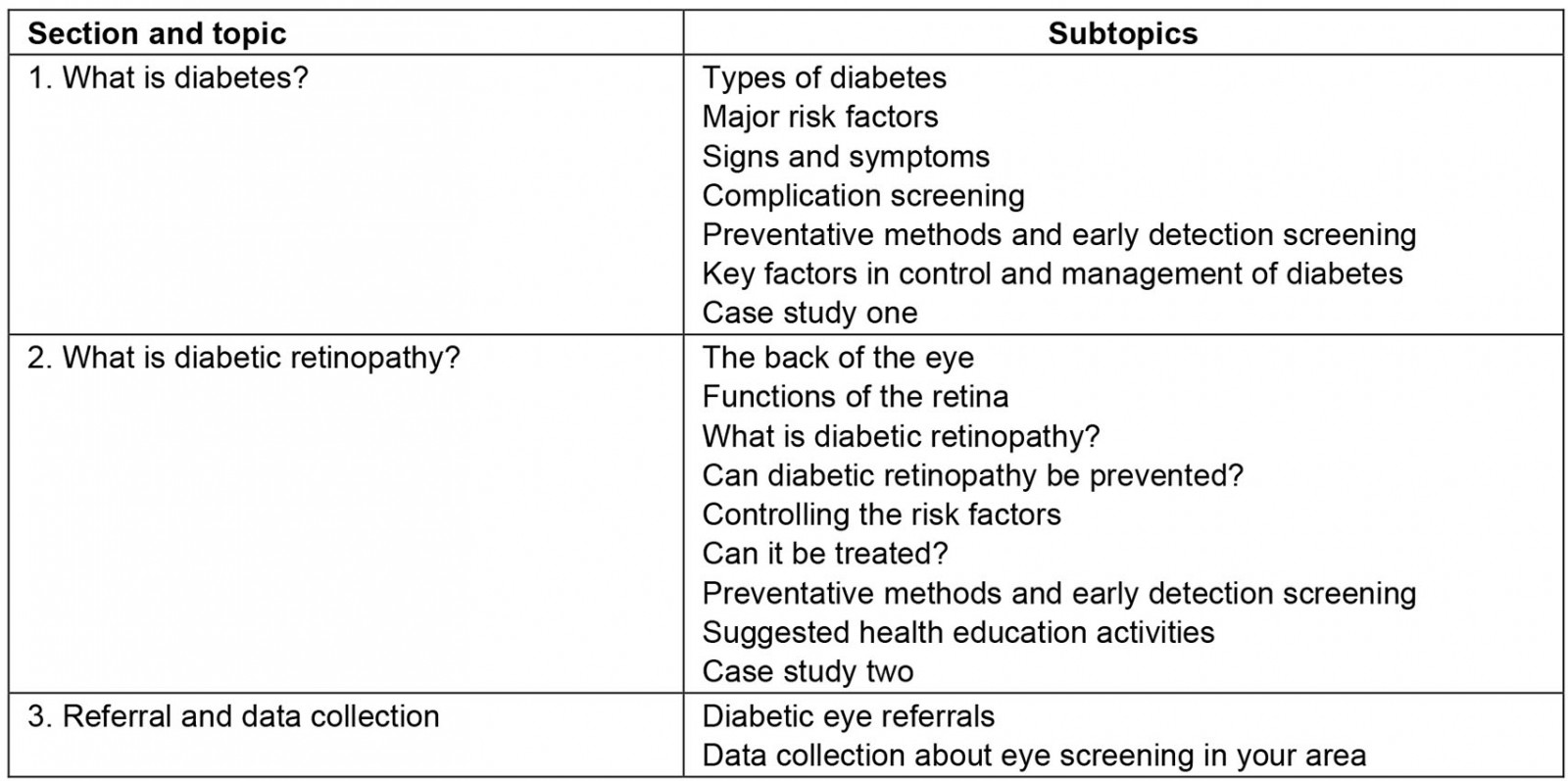
Methods
Study design and sample
A descriptive qualitative study design was used to explore the impact of DR awareness training and referral practices among the CHWs. Three focus group discussions (FGDs) were facilitated with the CHWs in January 2021 in three out of the four administrative divisions, namely Western, Northern, and Central Divisions, in Fiji.
Each administrative division in Fiji is led by a divisional medical officer and is responsible for providing public health services. There are five subdivisions in the Central Division, four in the Eastern Division, six in the Western Division and four in the Northern Division. The officers are responsible to the Deputy Secretary of Public Health, who heads the Public Health Division in the Ministry of Health and Medical Services headquarters in Suva. Public health services are provided through health facilities including 16 subdivisional hospitals, 77 health centres and 101 nursing stations. Each health centre is managed by a medical officer or nurse practitioner working with one or two nurses. It provides the first level of referral for several nursing stations and is generally staffed by one or two nurses – also known as zone nurses – who conduct outreach visits to communities in a designated nursing area. Community nursing stations, each staffed by a single nurse, are built and funded by the community, following approval by the government and according to government standards.
In addition, the Ministry of Health and Medical Services trained community members to serve as village health workers in Fijian villages and CHWs in Indo-Fijian communities. Patients may first see a village health worker, CHW or a nurse during an outreach visit or may go to a nursing station, health centre or subdivisional hospital.
The strength of the CHW model of care is that it has a high degree of flexibility in operation and it empowers community members and the CHWs themselves. Patients may be referred to a higher level health facility: one of the three divisional hospitals in Fiji16.
The CHWs were purposively selected to participate in FGDs by the DR program coordinator with access to a register that contained the profiles of CHWs. The inclusion criteria for a CHW to participate in the FGDs were that they had to be an active CHW and have attended the DR awareness training.
Fourteen CHWs participated in the three FGDs, with two groups having five participants (Central and Western Division), and the third group having four participants (Northern Division).
Data collection tool
A semi-structured, open-ended FGD guide was developed after an extensive review of local and international literature, which explored the impact of similar training on knowledge and changes in practice. The FGDs were vetted by the investigating team. The reason for selecting FGDs was to encourage participants to talk and interact with each other so that the group interaction encouraged respondents to explore and clarify individual and shared perspectives17.
Data collection process
Once the participants were identified, the DR program coordinator verbally explained the rationale including study methods over the phone using the participant information sheet. Those who agreed were provided a scheduled time to participate in a face-to-face FGD. The DR program coordinator assisted with convening the meeting and allocating a room for the FGD. Before each FGD, all participants signed a consent form for both participation and agreeing to the audio-recording. The researcher facilitated each FGD in English. Each FGD was audio-recorded. The duration of each FGD was approximately 60 minutes. The participants were acknowledged for their participation and compensated the monetary equivalent of their travel and meal costs.
Data management and analysis
All data collected in the form of audio files were kept in a password-protected computer. These audio files were transcribed verbatim immediately following each FGD by a member of the research team. To ensure anonymity, numbers were used instead of participants’ real names. A general inductive approach was utilised for analysing the collated qualitative data. Through a process of reading and re-reading the transcripts and discussion among the team, common and recurring issues were identified as key themes from the data. For each theme, a descriptive summary was written; indicative commentaries from the CHWs have been inserted to illustrate the views held by them.
Ethics approval
The ethics approval for the study was initially obtained from the College Health Research Ethics Committee at Fiji National University and then from the Fiji National Health Research Ethics Committee of the Fiji Ministry of Health and Medical Services (ID 303.20). Participation was voluntary, with the right to withdraw at any time. Informed consent was obtained for participation in the study and the use of an audio-recorder.
Results
Characteristics of participants
Of the 14 CHWs, 13 were female. All of them had a varying level of high school education and only one had tertiary education. The work experience of the CHWs was 1–18 years and those who had served 15 years did so voluntarily. The age range of the CHWs who participated in the study was 25–65 years. From 2018 onwards, the Ministry of Health and Medical Services commenced contracting the CHWs and paid them an honorarium for their work.
Themes identified
Five distinct themes were identified (Table 2) from the FGDs concerning DR knowledge, referral practices, challenges involved in referrals for screening, integration of CHWs within the health system and other spin-offs from the training.
Theme 1 identifies how new knowledge was acquired by the CHWs through an understanding of the concepts and clearing up misconceptions about diabetes. New knowledge led to participants becoming self-aware and making a healthy lifestyle. Their knowledge improved their advocacy skills around diabetes and DR.
Theme 2 highlights the differences in the referral practices of CHWs between pre- and post-training, with higher referrals after CHWs’ better understanding of referral pathways. This theme also highlights other factors that led to increased referrals such as the use of referral forms, enhanced communication and feedback with health facilities.
Theme 3 describes the challenges in making referrals for screening. These challenges are at various levels such as an individual level (eg poverty), community level (eg community support) and health-system level (eg cancellation of outreach visits).
Theme 4 discusses the integration of CHWs in the health system and touches on the issues of relationships between the CHWs with zone nurses, and support and respect including feedback systems.
Theme 5 describes other spin-offs from the training, which include how the training has empowered the CHWs, created role model families within the communities, and the CHWs’ positive lifestyle changes as a result.
In the analysis that follows, indicative commentaries from the CHWs are inserted to illustrate the views held by them.
Table 2: Themes and subthemes from focus group discussions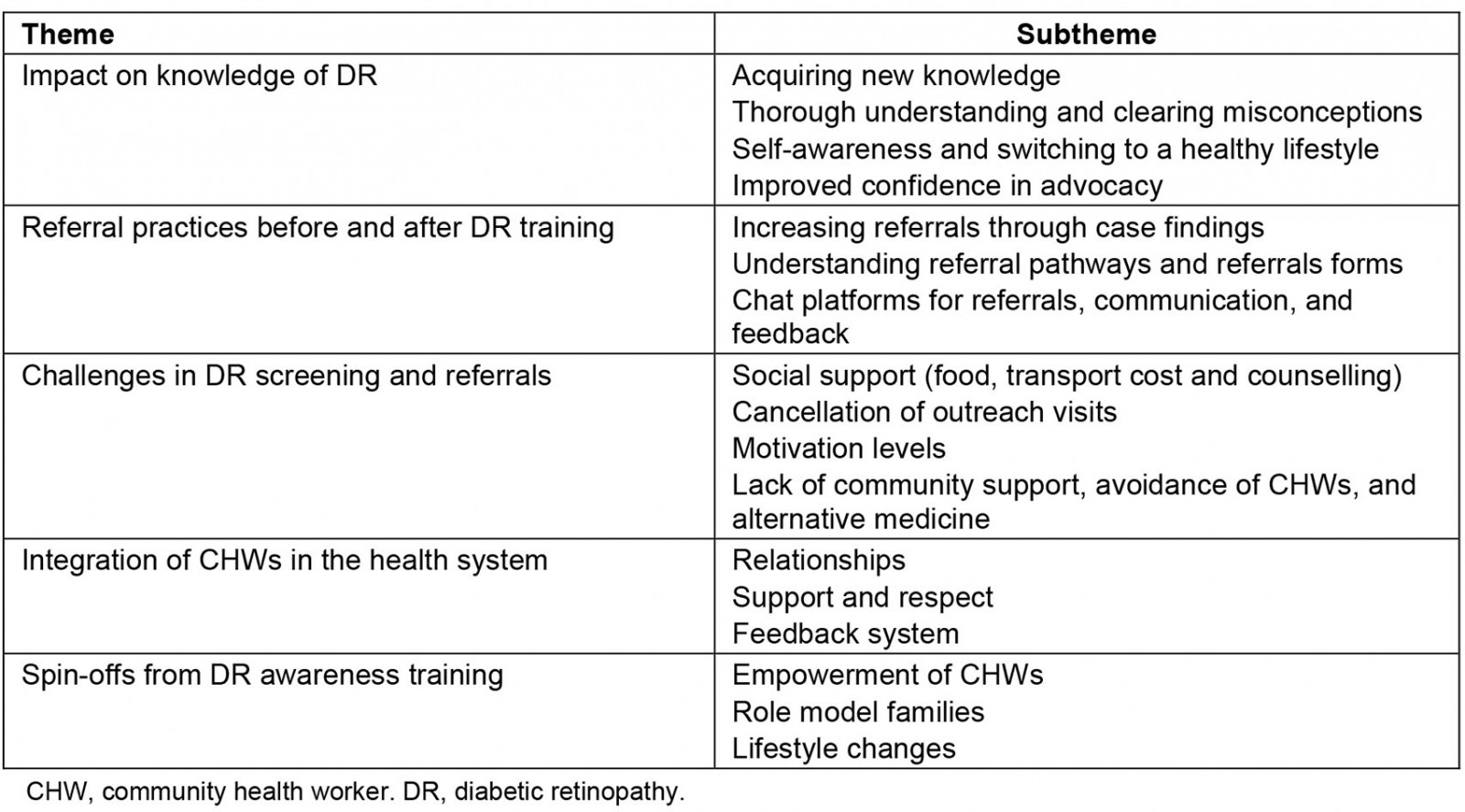
Theme 1: Impact on knowledge of diabetic retinopathy
All CHWs found the DR awareness training interesting, easy to understand and thorough. Queries asked by the CHWs during the training were answered and explained in lay language by the facilitator(s).
All CHWs felt that the training had improved their knowledge of diabetes, its signs and symptoms, prevention and care/management, as well as on DR as one of the complications of diabetes.
I learned a lot during the training and even as a CHW, I wasn’t aware of all those things such as symptoms of diabetes. Before we lived anyhow, but now have come across some cases in my village [and] I encouraged my village people to know about DR and change their lifestyle. (FGD1)
I can say that the DR workshop was the best one. It was good to attend because the doctor was explaining everything step by step and about keeping ourselves healthy. My mom was diabetic and got amputated. The workshop motivated me, and I told myself that I will never be diabetic, and I will change the way I eat. Now I am fit and it [is] just changing our mindset. (FGD2)
The CHWs mentioned that before the DR awareness training they only had superficial knowledge about diabetes and therefore they did not have enough confidence while talking to communities about diabetes and its complications. Their knowledge about diabetes was almost the same as people in the community. CHWs recalled only urging people to reduce sugar/sugary foods in their diet during community awareness sessions. According to CHWs, diabetes meant high blood sugar levels and higher odds of foot complications. CHWs also urged diabetic patients to protect their feet at all times particularly when outdoors or when engaging in activities involving tools as the chance of receiving cuts is increased. They said that any wound(s) would take a longer to heal, potentially resulting in amputation; they had come across many diabetes patients with amputated limbs.
The training helped clear many misconceptions about diabetes held by CHWs. New knowledge included learning that diabetes could result in poor vision or blindness known as diabetic retinopathy, that it is preventable if detected early, DR services are available for free in Fiji, and screening for DR is done during community outreach or at a health facility. CHWs also learned that diabetes can be managed, and vision can be improved if patients had healthy lifestyle practices and managed their diets appropriately. CHWs mentioned that the training also enabled them to know more about the structure of the eye, human anatomy and diet changes related to improving vision.
Being more knowledgeable about diabetes and particularly DR has helped CHWs increase community awareness on eye health and diabetes complications during community health awareness information sessions:
I did not have much awareness about diabetes before the training. After the training, I have started to take both diabetes and eye health seriously. I have been motivated to learn about diabetes prevention and eye care and share the knowledge with others in the village. I also advise people about food which is good and those that can cause blindness and are bad [for] diabetes and DR. (FGD2)
I got to know that diabetes not only affects the leg but also the eyes and the whole body. Before I just knew that it affected the legs resulting in amputation. (FGD1)
Before DR awareness training, CHWs lacked information on DR to share with communities. After the training, CHWs felt that they had gained adequate knowledge of diabetes and DR, and the confidence to talk about it within their community. CHWs mentioned that, regrettably, not being knowledgeable enough must have contributed to a lot of missed cases of DR for screening and treatment:
I think we may have missed much diabetes-related blindness because first, we didn’t know that diabetes can cause blindness, and, we didn’t know how to talk about diabetes properly like how we have been taught now. After training, we can share information properly with my community. (FGD2)
CHWs mentioned receiving the information, education and communication or health promotion materials on diabetes and DR, which they subsequently used in the community and considered valuable tools to disseminate accurate information on diabetes and DR to people:
The people in my community are very curious. They listen with interest. I used charts from our diabetic hub and show them the kind of life they should live. Now they know that if they do not lead a healthy lifestyle, their eyes will go bad and their leg may be amputated. (FGD3)
Further, all CHWs reported having improved community profiles with diabetes profiling that they developed for each of the households in their communities. The community profiles captured information such as basic demographic data, any underlying health or medical conditions, water and sanitation, and referral information for each community member. This enabled them to know their community’s health situation better. They continually updated the records of the individuals as well. The CHWs are required to complete a monthly report that provides details of the number of people who are ill, diabetic and/or visiting a health facility. The community profile register became a useful tool to report to their managers, the zone nurses, when they followed up with calls or village visits.
Theme 2: Referral practices and referral pathways
Before the training, CHWs ensured that existing diabetes patients attend their routine check-ups at the special outpatients department clinics and ensured that their medications were replenished. They encouraged people with slow-healing wounds to undergo diabetes and DR screening. They, however, did not endeavour to refer people experiencing vision loss/ blindness for screening as they were unaware that blindness was one of the complications of diabetes.
Post-training, the CHWs commenced referring not only the existing diabetes patients with vision loss/blindness for DR screening, but also those who were 40 years of age or over, had other symptoms such as vision loss, blindness, or increased thirst, to visit a health facility for screening for diabetes. All CHWs reported sending a significant number of people to a health facility after attending the DR awareness training and becoming aware of its signs and symptoms:
Before the training, we didn’t know that blindness can be one of the problems due to diabetes, so, I missed sending many people. Now I know, so I send anyone I feel needs to go for a screening. (FGD1)
Before the training, CHWs lacked clarity regarding the DR referral pathways for screening and treatment. The referral pathways became clear after the training. CHWs needed to refer patients to the zone nurses for DR screening, who then referred the patients to the doctors/ophthalmologist/eye departments for further treatment and management. During the training, the CHWs were provided with referral forms, required to be completed for every patient they referred to the zone nurses for screening. CHWs started keeping a record of referred patients in their community profile register. CHWs mentioned that when the patients took the completed referral forms to a health facility, they were prioritised and did not have to join a queue:
After the training, we knew about DR and we were also given referral forms. So, whenever we ask them to go for screening, we must complete the referral for that patient, and then we send them to the hospital. After the training, I have sent 10 people. Before the training, we only ask people to go to SPOD [special outpatients department clinic] for their checkup. (FGD1)
The Ministry of Health and Medical Services has started issuing CHWs with identity cards. Those who had identity cards had easier access to a health facility and were able to have the patients they accompanied seen more promptly than those CHWs who did not. CHWs were keen to obtain an identity card for their roles.
CHWs with good internet connectivity used chat platforms to share patients’ details including eye images with the zone nurses to receive instructions on whether patients need to be referred to them. This further enhanced communications among the CHWs and zone nurses. For urgent cases, CHWs phoned the zone nurses:
We are three of us in the Viber chat group. The group chat has helped in our communication as we can share information. Once we share a person’s information with the zone nurse, and if she is not sure then she shares it with the doctor, and we wait for the advice before we refer. The zone nurses respond in 30 minutes or an hour. (FGD2)
After the training, some CHWs have been able to identify new diabetes cases by asking patients they had a loss of vision:
For instance, 14 years old boy in my community said that he could not see well, and he drinks a lot of water and I suspected he had diabetes and referred. He was found to be diabetic, and he did not know before that he was diabetic. (FGD3)
CHWs in all divisions mentioned making regular village rounds to check on existing patients that are at home and cannot go to the hospital on their own, and connected them with the zone nurses. They advised patients to report to the zone nurses at their health facility or they accompanied patients to a health facility if they could not go by themselves. CHWs accompany the patients to the special outpatients department clinic, especially those who could not articulate their health conditions to healthcare workers:
We have domiciliary visits to check on the patients. If any patient is in a domiciliary case, and suddenly if he/she has something major like cannot breathe or shortness of breath, then we immediately call the zone nurse. We accompany these cases to the health centre or hospital. Sometimes they don’t want to go to the hospital and hide the seriousness of the case. We encourage them and at the end when they get better, they are thankful to us. (FGD2)
CHWs also helped the nurses organise the outreach clinics for screening and made a door-to-door visit to households when necessary to inform them about the scheduled outreach clinics.
CHWs who have served for longer in their positions are familiar with zones nurses and medical officers. This has enhanced their relationships and communication, and improved collaboration between CHWs and healthcare workers based at health facilities, allowing the CHWs to directly phone the nurses or medical officers at the health facilities, for ease of referrals:
It’s a small group of nurses and a doctor in our health centre. Most of the time I fill the form and refer patients and I don’t have to go. We just call the nurse or even the doctor because we know each other well. In an emergency, I always give a call to them. (FGD2)
Theme 3: Challenges for community health workers in the diabetic retinopathy screening and referral process
CHWs faced several challenges when referring DR patients for screening. First, people living in poverty cannot afford a balanced diet, transportation costs to a health facility, and other expenses involved in caring for a patient. Transportation costs were even higher for those who lived further from the health facilities. Elderly people could not take a long walk from their place of residence to use public transport. Some of these villages were serviced by a communal carrier; however, they were at a premium (FJD20 (A$12) one way) for those who were poor. At times, CHWs both accompanied patients and paid for transportation out of their own pockets:
I am in a Mahila Mandal [women’s religious group] and we collect money and help people who don’t have food or need any other support like transportation. We are only able to help a few and not everyone. (FGD2)
Second, people faced long waiting times at health facilities, which was frustrating for elderly patients who travelled long distances, were unaccompanied and were poor. The CHWs felt the burden on them was doubled when they had to support individuals who lacked family support, people from single-person households or domiciliary cases requiring more time of the CHWs.
Third, some individuals did not acknowledge the services rendered by the CHWs and were not cooperative, and needed the CHWs to present their identity cards. They either ignored their presence or avoided them altogether. CHWs mentioned that they tried to be persistent in their efforts to continually see the patients and encouraged them to undergo screening despite people avoiding them. Sometimes people used herbal medicines to cure diseases, and CHWs had to respect people’s choice; however, they continued to check to see how the patients were coping with herbal treatment. When herbal treatments failed, they encouraged patients to access health services at a health facility. CHWs usually revisited their patients to follow up if they accessed healthcare services at a health facility:
Sometimes some patients want to try herbal medicine and do not listen to us and hide from us. We let them cure themselves using herbal medicine, but we keep encouraging them to try medical help. We keep on visiting them regularly to see how they are coping and when they don’t get well, we talk to them and encourage them to take medical assistance and accompany them to hospital. (FGD2)
Fourth, sometimes scheduled community outreach screenings were cancelled at the last minute by the nurses. This caused inconvenience to the community as communities prepared meals for visiting health workers, and it is CHWs that spread the news about outreach to the communities. CHWs lose credibility with the communities when nurses cancel the outreach events. Further, despite outreach visits, some individuals would not turn up for screening despite the health teams of nurses and eye specialists visiting the community:
Before outreach, they [zone nurses] are the ones who call us and we inform the community that there will be a visitation. We walk down to every house to tell people and get everybody ready. I also put it on my noticeboard. They cancelled it 2–3 times saying that they don't have a means of transport. I went to get them and told them that people are waiting. (FGD3)
Other challenges included:
- patients being late or not presenting to a health facility despite being advised by the CHWs on adverse health outcomes
- CHWs not being bilingual to disseminate health messages effectively as some CHWs worked in mixed communities, compared to indigenous Fijian villages where CHWs could speak the vernacular
- lack of dedicated spaces in settlements for screening during outreach and confidential patient counseling, compared to dedicated village/communal halls in traditional Fijian villages
- to some extent CHWs difficulty in putting together a community profile and forgetting the knowledge gained over time.
Further, CHWs are not supplied with resources and consumables. Sometimes people in the community needed paracetamol tablets (pain relief medication) and equipment to measure blood pressure or diabetes, and it is an expectation of the community that these resources are supplied.
CHWs also followed up with patients in-person to check if they had been screened, after being referred by them. Currently, there is no feedback mechanism to notify the CHWs if their patients have undergone screening.
Theme 4: Integration of community health workers into the health system
Generally, CHWs felt that they were integrated within the health system. The participation of the CHWs in the DR awareness training and their subsequent work in advocating for diabetes and DR among other diseases, including making referrals for screening patients to health facilities, has improved their integration into the health system. The majority of the CHWs have served in their positions voluntarily for several years and have established a good working relationship with their managers (zone nurses). They are welcomed into the health facilities, feel respected, improved communication, and acknowledgement for their work made them feel part of the health system. There have been instances, however, where CHWs reported not being well received, particularly by new nurses. As one CHW said:
Sometimes some nurses do not recognise us for the work we do. She shouted a few times, not knowing that we help them by bringing the cases. I felt disrespected. (FGD3)
Theme 5: Spin-offs from diabetic retinopathy awareness work
CHWs felt empowered, having been trained in DR awareness and working within their communities, and they considered themselves privileged and being ‘called to serve their people’ in a spiritual context. Their work is supported by Turaga-ni-Koros (village chiefs). To improve the overall health of the village, chiefs used the health information collected by the CHWs to further advocate for good health. This is a source of motivation for the CHWs. The village chiefs also provide the meeting platform to CHWs to address their community members or other subgroups within the community, such as adolescents’ groups and mothers groups.
Within their community, CHWs modelled healthy practices by themselves, becoming model families to set examples for all households to follow. These included involving themselves in physical activity such as backyard gardening, and eating a healthy and balanced diet.
Apart from making referrals for DR screening, CHWs also endeavoured to address other issues in their community, helping the sick, elderly and domiciliary cases with food, transportation, and rendering other social support to the patients.
One of the CHWs mentioned that many of her family members have died from complications of diabetes, making her rethink and be conscious about her family’s diet and lifestyle. The training has assured her that people can avoid diabetes and DR by changing their diet, keeping physically active, and hydrating themselves:
After the DR training, when I returned to the village, I became more conscious of diabetes. Most of the ladies in my village are huge. I went around telling them, by knocking on every house and telling them about it, and encouraging them to do backyard gardening. I told them to eat healthily and now some of the ladies are doing it, they are planting pumpkin, eggplants, etc. (FGD3)
Before when we came to the city, my husband and I went to eat in the restaurant. Nowadays, when I come, I tell my husband he can go, but I won’t. I'll just eat the pineapple or any fruits at the market. (FGD3)
Discussion
This study aimed to determine the impact of the 1-day DR awareness training on the knowledge and referral practices of the CHWs, and this article reports the challenges experienced by CHWs in referring people for screening and CHWs’ integration within the health system.
Overall, in this study, CHWs reported significant improvement in knowledge of both diabetes and DR after the DR awareness training, similar to other studies8,11,18. It is noteworthy that CHW appointments are purely nominations by their community or village, based on certain desirable attributes and personal qualities such as having a good rapport, passion for community service and a desire to help people who are sick. A qualification in health is not a prerequisite but it may be an advantage. Prerequisites to serve as a CHW are some basic literacy skills to create and maintain records, and availability to undertake the work. Because CHWs did not have the subject knowledge, training in the specific area improved their knowledge of diabetes and DR.
Several studies have previously evaluated the impacts of diabetes-related training programs involving CHWs, and all have reported significant gains in knowledge by the CHWs19,20. The training discussed in this study was different from training for CHWs elsewhere because this training for CHWs was of 1-day duration only. Most training programs aimed at CHWs cited elsewhere have ranged from several days to months, and studies have evaluated the effects of training by assessing the level of knowledge pre- and post-training21. Despite the training being of very short duration, CHWs made significant knowledge gains. Another reason this training has made a significant impact is that it focused on DR only, thus the content was more easily assimilated by the participants. Future studies could potentially undertake pre- and post-training assessment to quantitatively assess the gains in knowledge. Further, the CHWs in this study requested periodic refresher training. Training of longer duration, which uses a variety of learning approaches – interactive in-class learning as well as e-learning and reflective learning – could potentially benefit CHWs and communities as well. A study also showed that, over time, CHWs needed retraining to refresh their knowledge11, which is consistent with the views of the CHWs in this study.
CHWs felt empowered in their positions among this cadre of health workers, where a desire to gain social recognition, and a sense of social responsibility and self-efficacy, motivated them to perform their duties; this has also been noted by other studies22. While the majority had served for a long period and built a good rapport, some indicated that at times they did not feel part of the team with the other facility-based healthcare workers, and they sought greater acceptance. Tshering et al, in their study among CHWs in Bhutan, describe several demotivating factors, including poor support from supervisors23.
The present study found that CHWs have a significantly high number of referrals of patients for screening for DR post-training. This could be attributed to their increased knowledge about both diabetes and DR, as they are better able to inform people about the signs and symptoms of diabetes and can encourage people to attend screening. Moreover, as they have also become more aware of the referral mechanism and pathways, they are better able to communicate this to their communities. In terms of referral of a patient by a CHW to health facilities, CHWs mentioned referring a significant number of community members for eyecare screening and subsequent treatment, with a high adherence rate; follow-up by CHWs was reported to be good. This could be because CHWs had a better understanding of the referral pathways and, with the provision of the referral forms to the CHWs, referring a patient with their details would be easier. A high adherence rate is potentially reflective of a good quality of eyecare service at the health facilities and would encourage more people to access the service. Other studies have shown similar mechanisms of referrals7, including the use of digital technology for communication and referrals24.
It would be valuable to capture information at each strategic point (eg health facility, Pacific Eye Institute) about who referred patients to access eyecare services or where they heard about eyecare services. This information could be used to invest in strengthening the referral pathways.
This study highlighted several challenges for CHWs. While the majority of the CHWs felt empowered and respected by both the community and other healthcare workers, which was a source of motivation, as noted in other studies25, for them to continue in their roles, some people avoided the CHWs, undermined their critical roles and saw them as insufficient as they only offered promotional services rather than diagnostic and treatment services26. Although the study resulted in gains in knowledge of diabetes and DR, the duration of the training was probably too short for the CHWs to improve the behaviour change of at-risk populations with diabetes in their communities21. Further, CHWs reported challenges in their work such as having to provide social support apart from their core work. This is consistent with studies in other settings such as in the USA, where CHWs took several roles, including connecting to community resources27.
In terms of the non-adherence to referrals by the community members, a similar investigation of the role of CHWs in Pakistan found that they reported challenges such as poverty, deep-rooted gender inequities and transportation difficulties. This was very similar to the challenges reported by the CHWs in the present study except that no CHWs mentioned gender inequities; in Pakistan these inequities could be due to the patriarchal values of the country28.
The feedback mechanism utilised by some CHWs and zone nurses is noteworthy as they have used chat platforms such as Viber to be able to refer patients in cases were CHWs were not able to accompany them to HF and where zones nurses recommended patient visits. Limitations of this method include internet unavailability in rural and remote areas and lack of funding by the health ministry. The use of mobile technologies for communication is not new within health care and varies in different settings29, and it has limitations unless there is 100% coverage within a country. Such technologies have been found to reduce consultation time and patients’ waiting time as well as the length of stay at the health facilities30.
Other studies have shown that engagement of CHWs has proved successful with the prevention and management of other diseases including diabetes in the community, and thus their services should be optimised8. The CHW model has been found effective for health promotion in disadvantaged communities in several ways. Quality of life has improved through better patient–provider communication, continuity of care, and because CHWs can provide support services for domiciliary cases or patients without a caregiver31.
Strengths and limitations
This study reported results from a purposive sample of CHWs from peri-urban and semi-rural areas, and thus this is not generalisable to all CHWs. It did not include CHWs from remote and maritime zones due to accessibility issues.
Nevertheless, this is the first primary study to determine the impact of the DR awareness training for CHWs with relation to their work in DR knowledge, awareness, referral and care. Further research focusing on the views of the recipients/community members regarding the DR-related services provided by the CHWs would provide insights on how to improve the work of CHWs.
Implications and recommendations
Based on the research, several recommendations can be made. The implementing agencies (Pacific Eye Institute and the Ministry of Health and Medical Services) should continue strengthening the capacity of the CHWs by continuing the training, as well as refresher training to those previously trained, to ensure early referral, screening, detection and treatment of DR. Financial and other social support incentives could be explored to ensure that patient access to DR services is improved. Feedback and communication between the CHWs and healthcare workers at health facilities needs to be improved.
Acknowledgements
We acknowledge the Fred Hollows Foundation New Zealand for granting this project. We thank all the CHWs who participated in this study. We also thank Dr Moneeta Pal and Dr Prarthana Dalmia for their support and valuable comments during proposal development and manuscript preparation.
References
You might also be interested in:
2018 - “Surfing the coastal wave”-a new way to consider workforce distribution
2010 - A multi-university evaluation of the rural clinical school experience of Australian medical students



