Introduction
Parkinson disease (PD) is a prevalent neurodegenerative disease that affects the elderly1. Patients with PD are characterized by both motor and non-motor symptoms, including rigidity, tremor, bradykinesia, cognitive impairment, and sleep disturbance2. In China, the prevalence of PD is approximately 1.7% among people over the age of 65 years3, and this percentage is continuing to rise as the population ages. Falls are common in PD patients with an average incidence of 60%; 35–90% of patients fall at least once, and recurrent falls accounts for 39% of all falls (range 18–65%)4. Falling causes pain, fractures, fear of falling, limited ability to perform daily tasks, and increased caregiver burden5. Compared with healthy controls, patients with PD have nearly twice the risk of fracture6. The cost of fall-related fractures in patients with PD is twice that of patients without fractures7, which has remarkable economic implications for patients and society.
Previous falls, increased disease severity8, movement variability9, freezing of gait10,11, and dyskinesia12,13 are predictors of falls in patients with PD. Moreover, cognitive impairment12,14, fatigue15, executive dysfunction16, and fear of falling17 increase the risk of falling. Most researchers focused on the impact of motor and non-motor symptoms on falls and ignored the impact of environmental factors, such as place of residence, type of housing, and bathroom facilities. Previous research found that, among older adults in Chinese communities, those living in rural areas had higher rates of falls than those living in urban areas, and the risk factors for falls differed between patients in different areas18. The same findings were reported in another study conducted in South Korea19. Due to uneven regional development and a lower economic level, older adults in rural areas were more likely to live in environments with inadequate facilities. Houses with barriers20 and bathrooms with fewer facilities21 were reported to be linked to falls in older adults.
The risk of falls in PD patients is increased by intrinsic and extrinsic factors. Although numerous studies have identified intrinsic factors contributing to falls, few studies have focused on extrinsic factors. Since China is a developing country with disparities between urban and rural areas, residence may be one of the external factors. This study aimed to analyze clinical features, clinical scale score, residence, and caregivers to determine potential risk factors associated with falls in PD patients.
Materials and methods
Participants
A total of 100 patients with PD were recruited from Anhui Provincial Hospital (Hefei, Anhui, China) between July 2017 and December 2020. The diagnosis of PD was based on the UK Brain Bank criteria22 and the 2015 clinical diagnostic criteria of the Movement Disorder Society23. The exclusion criteria were as follows: (1) a H&Y stage greater than 4; (2) remaining in bed or being in a wheelchair for long periods; (3) using antipsychotic medication; (4) having serious visual or hearing disability that affects balance; (5) having stroke sequelae or rheumatoid arthritis that impairs limb movement.
Data collection
Structured interviews were conducted by trained assessors to obtain clinical information and fall experience in the previous 3 months from patients and their caregivers. The patients were divided into fall and non-fall groups, based on whether they had fallen in the previous 3 months. Falls was used as a categorical variable rather than a continuous variable because it was easier and more accurate for elderly patients to recall whether they had fallen than how many times they had fallen in the past. Each patient’s information, including age, gender, disease duration, education level, body mass index (BMI), comorbidity, sleep disorder status (insomnia, daytime sleepiness, rapid eye movement sleep behavior disorder), was collected by paper-based questionnaires. Patients were classified as urban or rural residents, and their primary caregivers (those living with the patient and providing daily living assistance) were recorded. Those without a caregiver were defined as living alone.
The Unified Parkinson's Disease Rating Scale part III (UPDRS-III)24 and the Hoehn–Yahr (H&Y) scale2 were used to assess the degree of motor impairment and disease severity, in which a higher score or stage indicates a worse condition. The UPDRS-III is composed of 14 items that systematically evaluate tremor, muscle stiffness, postural stability, and limb flexibility, all of which reflect the severity of motor symptoms. The Mini-Mental State Examination (MMSE)25 was used to assess cognitive function, in which lower scores indicate poorer cognitive function and scores less than 24 indicate cognitive impairment. The Barthel Index was used to assess patients’ ability to perform daily tasks; a low score indicates a poor quality of life and a lack of self-care ability.
Statistical analysis
The Statistical Package for the Social Sciences v23.0 (IBM; http://www.spss.com) was used for the statistical analyses. Normality was tested to distinguish between normal and non-normal quantitative parameters, and mean±standard deviation or median (25th, 75th percentiles) was used to describe the results. Variations were evaluated using student t-test or Mann–Whitney U-test. The qualitative parameters were described using frequency and percentage, and differences were analyzed using χ2 test. Two-tailed p<0.05 was considered significant. Variables considered clinically relevant and showing a univariate relationship with the outcome (p<0.05) were enrolled in a forward conditional logistic regression model. The results were expressed as odds ratio (OR) with 95% confidence interval (CI).
Ethics approval
The study was approved by the Ethics Committee of the Provincial Hospital affiliated to Anhui Medical University (2018KY No. 30) and designed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
Results
The study included 100 patients (mean age 62±10.5 years; 51 males and 49 females), 42% of whom had fallen in the previous 3 months. All the patients participated in the survey and completed the questionnaires. The details of demographic and clinical characteristics in the fall and non-fall groups are shown in Table 1. Those who reported falls were older (mean age 66.4 v 58.8 years; p<0.001), had significantly longer disease period (median, 6 v 2.5 years; p<0.001), showed higher UPDRS-III scores, higher H&Y stages and lower Barthel Index scores (p<0.001). The patients in the fall group expressed lower MMSE scores and a higher proportion of MMSE<24 (p<0.01). The fall group had more patients with sleep disorders, living in rural areas, and living alone than the non-fall group (p<0.05). Gender, BMI, education level, hypertension prevalence, and diabetes prevalence did not vary remarkably between the two groups.
The variables that showed p<0.05 significance in the univariate analysis (age, duration of disease, H&Y stage, UPDRS-III score, Barthel Index score, place of residence, MMSE score <24 and with sleep disorders) were included in the forward conditional logistic regression. Finally, living in a rural area, having MMSE<24, having sleep disorders, and having a high UPDRS-III score were major risk factors for falls (Table 2).
Logistic regression showed that living in a rural area was an independent risk factor for falls in patients with PD. Rural patients have a 3.3 times higher risk of falls than urban patients (OR=3.337, 95%CI 1.15–9.65, p<0.05). Therefore, a post-hoc analysis was performed to compare the differences between urban and rural patients. Patients were divided into urban and rural groups according to their residence. Demographic and clinical data were analyzed using students t-test, Mann–Whitney U-test, and χ2 test. The results are presented in Table 3. No between-group differences were found for age, disease course, or gender. However, rural patients showed higher UPDRS-III scores (35.3±12.5 v 29.6±14.5, p<0.05), higher H&Y stages (median (interquartile range, IQR)=2.5 (2–3) v 2 (1–3), p<0.05), and worse Barthel Index (median (IQR)=75 (60–90) v 85 (70–95), p<0.05) than urban patients. Rural patients had lower educational attainment than urban patients. A total of 16 of 55 (29.1%) rural patients had secondary school degrees or higher, while 40 of 45 (88.9%) urban patients had secondary school degrees or higher (p<0.05). More rural patients were cared for by their children, whereas more urban patients were cared for by their spouses.
Data on patients in the fall group was stratified according to residence, and the results are presented in Table 4. No differences were found in duration of disease, UPDRS-III score, MMSE score, or H&Y stage in rural and urban patients. However, urban patients had higher levels of education, with 91.7% of them having a secondary or university degree, whereas 76.7% of rural patients had only a primary school education, or had never been educated.
Table 1: Demographic and clinical characteristics assessment: fall and non-fall groups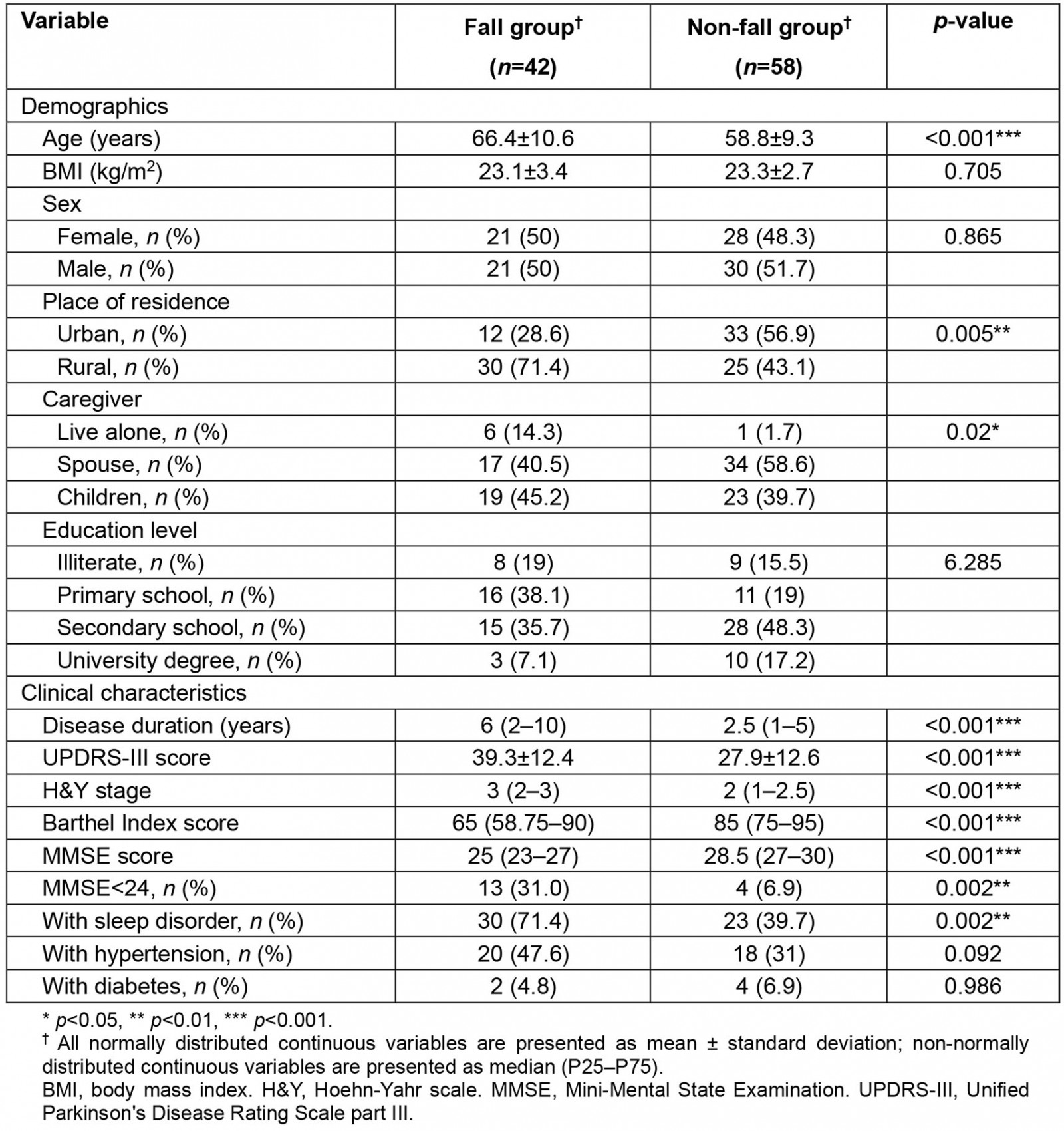
Table 2: Forward conditional logistic regression of fall risk factors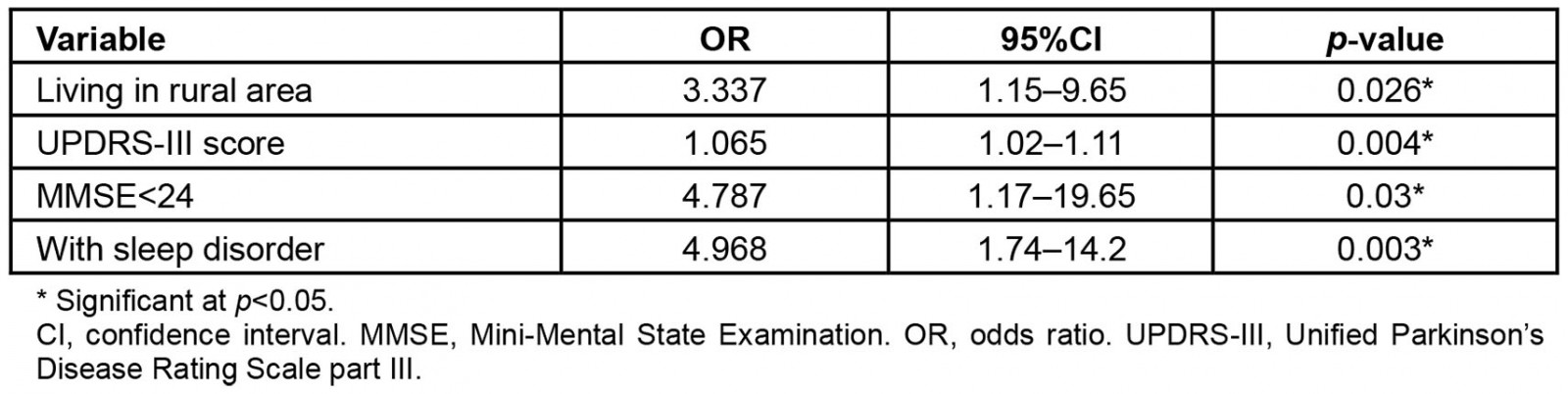
Table 3: Demographic and clinical characteristics assessment: comparisons of patients in urban and rural areas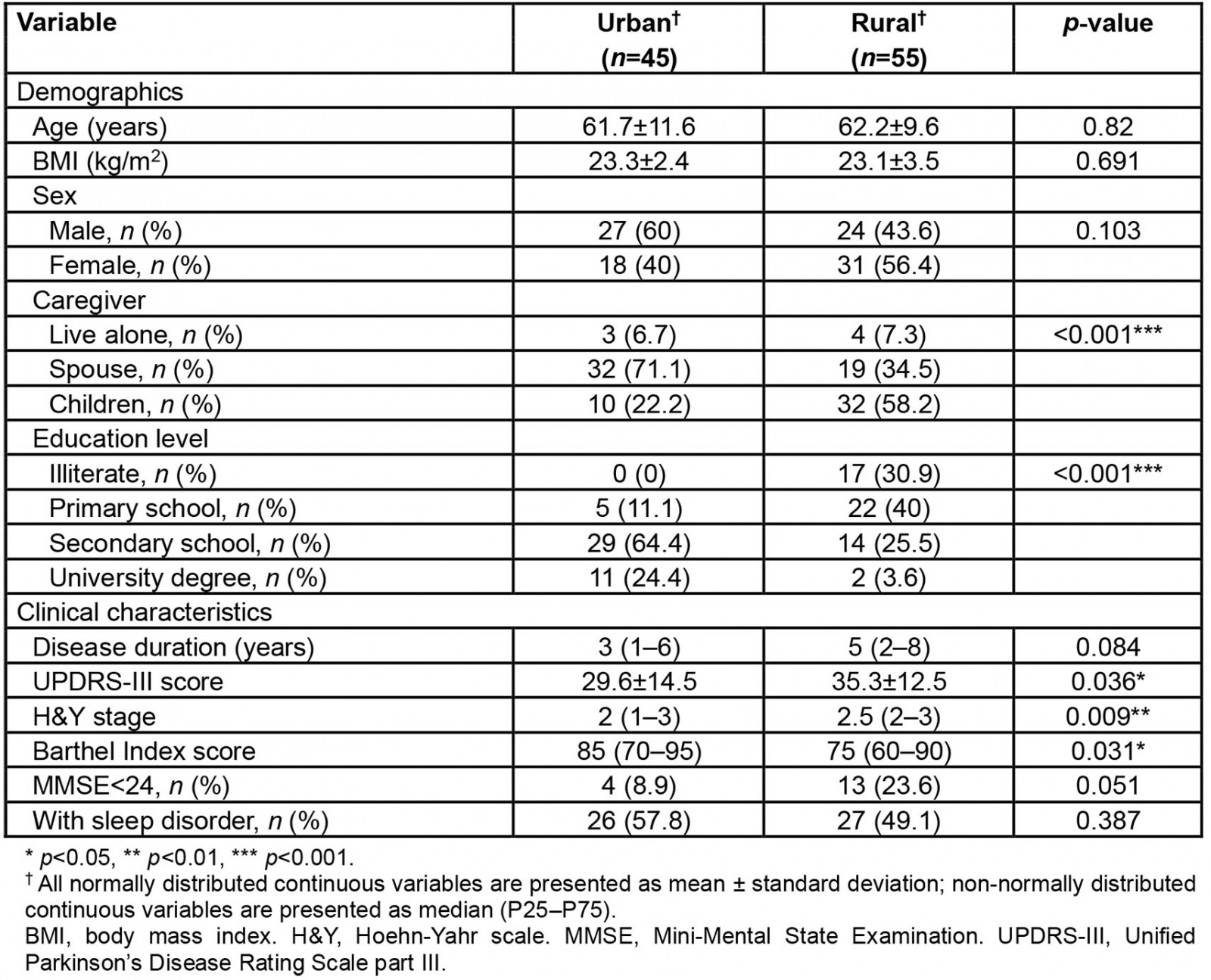
Table 4: Demographic and clinical characteristics of fall group patients in urban and rural areas
Discussion
In this study, the incidence of falls in the previous 3 months among patients with PD was recorded and disease-related indicators assessed. The results revealed that falls are very common in patients with PD; 42% of the patients had fallen in the previous 3 months. Early identification of risk factors for which intervention is possible is critical for patients who are at high risk of falling.
This research explored the impact of urban–rural differences on falls in patients with PD, which has rarely been reported in previous studies. According to multiple logistic regression, a high UPDRS-III score and living in a rural area were both risk factors for falls. The post-hoc analysis showed that rural patients had more severe motor symptoms and more advanced H&Y stages, and this could be related to their high rate of falls. A previous study based on a community elderly survey reported that elderly people in rural China have a higher risk of falling than urban residents18. The present study found the same result in people with PD. Urban residents in China have better access to public services, higher education standards and higher average income than rural residents18,26. Previous research reported that poor access to health care is linked to increased rates of disability, cognitive impairment, and all-cause death among the elderly in China; rural older adults had stronger correlations between healthcare access and health outcomes than urban older adults27. Many cities have easy access to medical services such as hospitals and medical personnel, whereas most rural areas do not have the same ease of access. Rural patients may be unable to be treated by specialist physicians and afford costly medications, which may have influenced their motor symptoms. Inadequate house facilities and limited awareness of the disease may complicate the situation.
It was noted in this study that caregivers vary between urban and rural patients. Rural patients are more likely to live with their children, whereas urban patients are more likely to live with their partners. However, no association was found between caregivers and falls in patients with PD.
The UPDRS-III is the third part of the UPDRS and reflects the severity of motor symptoms; it was remarkably associated with falls in PD patients in this study. Previous research reported an inverted U-shaped relationship between the probability of falls and the UPDRS-III score28. The risk of falling increases as the UPDRS-III score increases and then decreases as the value exceeds 50. This decrease may be because people with more severe diseases intentionally avoid walking. The H&Y stage also represents disease severity and was higher in the fall group than in the non-fall group, but it did not contribute substantially to falls in the logistic regression. This result may be because broad categories have less ability to show trends than continuous variables, such as the UPDRS-III.
The relationship between cognitive impairment and falls has been reported in many studies, especially in patients with PD11,14. Latt et al reported that mild cognitive impairment based on MMSE<27 was associated with an increased risk of falls in patients with PD11, which is consistent with the present research. PD patients with cognitive impairment are more likely to fall than the general elderly population; this may be associated with decline in a patient's attention, memory, and executive capacity12. A previous study reported that donepezil can reduce the risk of falls in patients with PD29. The drug may reduce falls by enhancing the attentive and cognitive function of patients rather than by affecting balance itself, but its practicality has not been widely accepted.
The present study’s data showed that the existence of sleep disorders was an independent risk factor for falls in patients with PD. The result was consistent with a recent study on falls in Chinese adults over the age of 50 years30, in which the researchers discovered that those who sleep fewer than 5 hours each night have a greater fall rate than those who sleep more than 6 hours. People with PD are more likely to have sleep disorders than the general elderly population, and many patients are long-term users of hypnotic drugs. Some ‘Z’ drugs, including zolpidem, zopiclone, eszopiclone, and zaleplon, increase the risk of falls and fractures31. Further research is needed to determine the association between hypnotic drugs and falls in patients with PD.
This study had several limitations. Falls are caused by complex factors, but intrinsic and environmental factors were not adequately included in this study, such as the daily dosage of medications, housing facilities, and the use of walking aids and hypnotics. The fall experience data used in the analyses was based on memories of patients or their caregivers from the previous 3 months. Thus, memory bias may exist, especially in patients with PD who have impaired memory. The incidence of falls may have been underestimated and repeated falls were not discussed. This is an exploratory study with only 100 patients included, which is a significant disadvantage when compared to similar studies. Due to the insufficient sample size, the results of this cross-sectional study were unstable. Prospective studies with larger sample sizes are needed in the future to draw credible conclusions.
Conclusion
Falls are common among people with PD and are associated with complex factors. Living in a rural area, high UPDRS-III scores, cognitive impairment, and sleep disturbance may be associated with falls. In addition, rural patients with PD have higher fall rates than urban patients. Multidimensional studies in PD patients are needed, and individualized interventions should be made to prevent falls.
Acknowledgements
We thank the Neurology Department of the Provincial Hospital affiliated to Anhui Medical University for assistance with data collection. This work was supported by the Department of Science and Technology of Anhui Province (grant no. 1704f0804011).
References
You might also be interested in:
2022 - Factors associated with adolescent birth in Indonesia: a national survey
2022 - COVID-19 fosters social accountability in medical education
2006 - New payment model for rural health services in Mongolia

