Dear Editor
International attention has been drawn to the alarming rates of firearm violence, injury, and fatalities in the US. Much less attention is drawn to the fact that most US firearm deaths are suicides and that firearm suicide rates are highest in rural areas1. We demonstrate the duality of rurality and firearm suicide using data from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research (CDC WONDER), which gathers mortality data reported through state death certificate registries1. We extracted national age-adjusted mortality rates for 1999–2020 overall and stratified by urbanization and firearm involvement for both US and West Virginia, a rural state with high rates of firearm ownership.
CDC WONDER data show a direct correlation between rurality and all-cause suicide mortality in the US, with urban categories (ie Large central and Fringe metro) having significantly lower rates than less urban categories (ie Micropolitan and Noncore) (Table 1). However, stratifying by injury mechanism demonstrates that firearm involvement is key in understanding this rural excess. Firearm-involved suicides occur at a higher rate than non-firearm suicides and follow an identical pattern to all-cause suicide rates: increasing rurality is associated with higher rates. This effect is more pronounced in West Virgina. Non-firearm suicides, however, do not display such a relationship, with variation across urbanization categories, and in West Virginia do not significantly differ by urbanization whatsoever.
Published research indicates that rural-specific social factors, including social isolation and a strong sense of self-reliance (‘rugged individualism’), may increase rural individuals’ risk for suicide2. What the data presented in Table 1 indicate, however, is that access to lethal means in rural areas may be responsible for a transition from attempt to completed suicide. This hypothesis is strengthened by US survey data indicating that rural firearm ownership rates are more than double those in urban areas3. Moreover, firearm owners are more likely to view firearm ownership as essential to their sense of freedom3, suggesting there is a strong cultural connection to firearms in the rural US.
Firearm-specific suicide prevention measures, such as ‘red flag laws’ precluding access to firearms during acute mental health crises, have demonstrated effectiveness4. However, few rural states have implemented such laws, potentially due to the connection between firearm ownership and freedom experienced by US gun owners. What is needed, therefore, is research into what suicide prevention measures may prove feasible in the rural US. This includes both how to frame existing evidence-based firearm suicide prevention strategies (eg red flag laws) so they are more readily accepted by rural gun owners, as well as developing novel prevention strategies.
The lack of research in this area was outlined in a scoping review of suicide prevention methods in rural US veterans, which noted that only one suicide prevention resource has been developed for this group and there are no evaluated interventions5. While this review was specific to the rural veteran population, it reflects a broader trend in suicide research. Rural health researchers should seek evidence-based, firearm-specific suicide prevention solutions targeted towards rural US populations.
Dr Eric W. Lundstron, Department of Epidemiology and Biostatistics, School of Public Health, West Virginia University
Dr Jacob K. Pence, Transitional Year Residency Program, School of Medicine, West Virginia University
Dr Gordon S. Smith, Department of Epidemiology and Biostatistics, School of Public Health, West Virginia University
Table 1. Age-adjusted suicide mortality in the United States with 95% confidence intervals†, stratified by urbanization and mechanism (1999–2020)1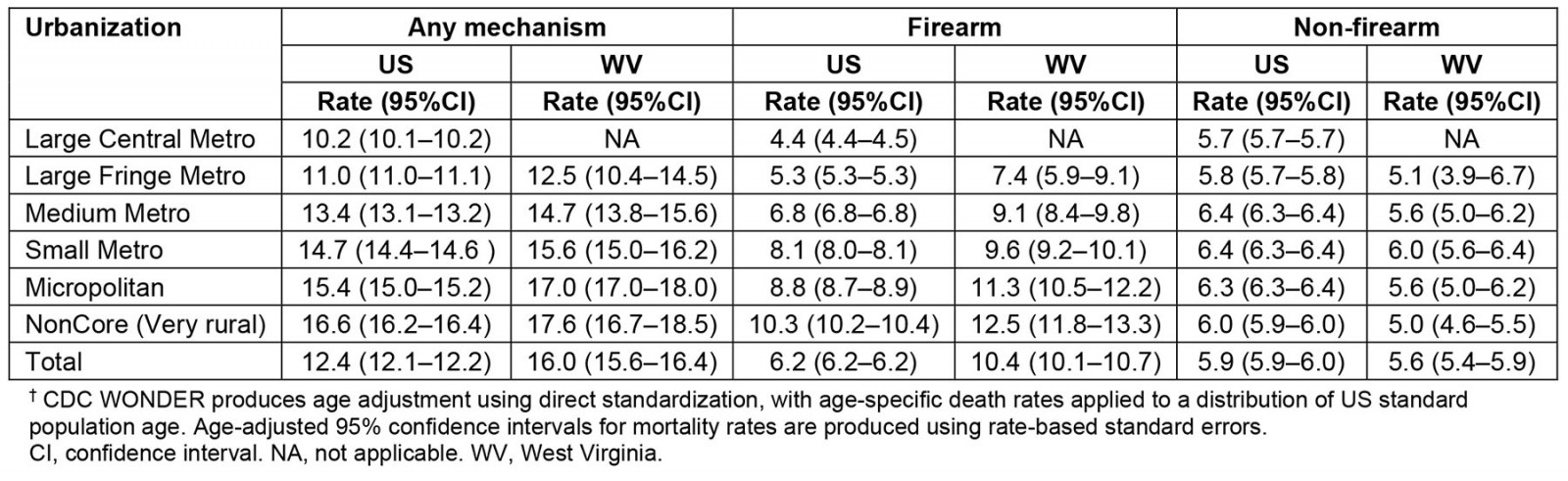
Funding
This work was supported in part by the National Institute of General Medical Sciences (2U54GM104942).
Conflicts of interest
The authors declare no conflicts of interest.
References
You might also be interested in:
2008 - Obstetric services in small rural communities: what are the risks to care providers?
2004 - Oil doom and AIDS boom in the Niger Delta Region of Nigeria

