Introduction
Psychological safety is the belief that one will not be punished or humiliated for ideas, questions, concerns, or mistakes, and it is essential for effective medical education1. Team members should share the belief that a team is safe for interpersonal risk-taking2,3. When a team feels psychologically safe, its members feel comfortable speaking up, asking questions, and sharing their opinions. Consequently, there is better communication, more creative solutions, and improved performance, subsequently increasing the teams’ effectiveness2,3. Creating a culture of psychological safety in a team requires leadership that actively encourages open communication, listens to team members, and creates a suitable environment4. In medical education, the collaboration between students and teachers is essential for learning, and psychological safety can drive this5. As psychological safety can substantially impact the learning and performance of medical students, it is a crucial concept in medical education.
The difficulty in improving psychological safety in medical education can be attributed to the hierarchy among medical professionals6. Medical students and residents experience a professional hierarchy in their relationships with their medical supervisors, which impinges on their psychological safety7. Although educational culture and background can affect attitudes toward teachers, various studies from multiple countries have examined the effects of professional hierarchy on psychological safety8,9. Based on our past research it appears that, particularly in rural contexts, traditional rural practitioners are initially not used to teaching medicine and to having a solid relationship with their students without facilitation and instruction10,11. When medical learners experience a strict professional hierarchy, there may be a loss of psychological safety in rural medical education. Educational systems and methods should therefore be revised to enhance and overcome the effects of professional hierarchy on psychological safety.
An increase in learning between students and residents can increase psychological safety. One of the learning methods for this is near-peer learning (NPL), which can drive collaboration and mutual learning between medical students and residents12. In NPL, learners proactively teach and learn with their peers based on their cases, and discuss their questions with teachers12. The application of NPL ensures that learning in community health practices is not limited to medical teachers, thereby broadening learners’ perspectives12. It can be applied in various educational contexts, including rural community-based medical education (CBME)13. In rural contexts, NPL can improve medical trainees’ participation in medical teams, which drives their learning14. It can also mitigate the lack of psychological safety in medical teams by making students feel a sense of safety15. Thus, the positive experiences and emotions associated with NPL may inspire medical learners to consider working in rural areas in future16.
By improving psychological safety, members of medical teams, including medical students, can collaborate as team members for the effective care of patients17 and to mitigate their burdens. In rural hospitals, experienced medical professionals with long tenures successfully communicate with each other and effectively include medical learners. Thus, psychological safety may be managed more effectively in rural than in urban hospitals. Psychological safety is essential for the effective involvement of medical students. Effective rural CBME with NPL may also increase healthcare students’ psychological safety and motivation, increasing the number of medical staff motivated to work in rural contexts. Moreover, driving rural CBME with NPL can facilitate the sustainability of rural medicine. In Japan, NPL applied in rural contexts improved motivation and self-directed learning in family medicine and CBME13,14. However, a lack of psychological safety among peers and medical teachers may impinge on the implementation of NPL in CBME. The clarification of psychological safety in CBME can facilitate the implementation of NPL. However, only very few previous studies have explored psychological safety in rural CBME or how to promote psychological safety. To promote psychological safety, we implemented NPL for rural CBME family medicine residents, medical residents, and students under the supervision of family medicine teachers18. The research question was, ‘How does NPL in CBME change medical trainees’ perceptions and behaviors of learning regarding psychological safety?’
NPL in rural CBME is useful for reducing the burden of medical teachers in these contexts due to the lack of medical resources13,14. By clarifying the process and effect on participants’ learning and psychological safety, this method may be effective in rural contexts that lack medical staff and educators. It could promote psychological safety among medical trainees and improve patient care in rural community hospitals with minimal resources. Therefore, this study aimed to clarify the effects of NPL in CBME on medical trainees’ psychological safety and learning.
Methods
This qualitative study used a grounded theory approach using medical students and residents undergoing training at a rural Japanese community hospital.
Setting
This study was conducted at Unnan City Hospital in south-eastern Shimane Prefecture, rural Japan. The hospital has 281 care beds: 160 for acute care, 43 for comprehensive care, 30 for rehabilitation, and 48 for chronic care. The hospital has provided CBME to university students and residents of tertiary hospitals since 2004. Its curriculum ensures that medical students and residents experience various clinical situations for treating inpatients, outpatients, and patients in homes and community care. Each clinical setting has a medical teacher11.
Medical students and junior residents receive rural family medical education in medical and tertiary hospitals. As part of their university or hospital curriculum, they train in a family medicine internship or residency program at a rural hospital for a month with medical teachers and family medicine residents. The rural hospital annually accommodates 40 to 50 medical students and junior residents for training.
The hospital follows a rural family medicine education curriculum that includes three teachers, and residents encounter various clinical situations while treating patients. In their first year, residents work at the Unnan City Hospital and treat typical diseases in both inpatient and outpatient settings. In the second year, they work at a rural clinic (Kakeya Clinic) for months to learn about home care and community-oriented primary care. To broaden their scope of practice in internal medicine, pediatrics, and emergency medicine, residents also work at general or community hospitals for 18 months19.
Participants
Between April 2021 and December 2022, 53 medical students and 16 residents were assigned to participate in the CBME curriculum, including family medicine, at Unnan City Hospital. They voluntarily joined from university or tertiary hospitals across Japan. The training aims to produce the competencies required in Japan’s general medicine areas such as person-centered care, comprehensive and integrative approaches, interprofessional work, community orientation, professionalism, and systematic practice. We invited all participants in the CBME curriculum or family medicine residency program at Unnan City Hospital to undergo semi-structured interviews. In total, 38 medical students, 12 second-year residents, and 8 family medicine residents agreed to participate in this study.
Near-peer learning in rural community-based medical education
The Community Care Department of Unnan City Hospital implements team-based patient management, including NPL. In this department, 100 to 120 patients are admitted to the hospital, and family physicians care for approximately 1800 patients annually19. Each family medicine resident is assigned 15 to 20 patients. During the daily morning conference, they share their patients’ conditions with other members, and discuss management plans for the improvement of psychological safety in NPL. During the day, they consult the department director on their patients’ conditions, and safely progress with their treatments for improving the quality of care through NPL13.
Among trainees in team practices, a family medicine supervisor supervises and shadows the three first-year, three second-year, and two third-year residents. Family medicine residents are allocated to two teams consisting of four or five members. In addition to the morning conference, each team shares and discusses their patients’ conditions and support each other, leading to effective patient management14.
Medical students and junior residents are allocated to each team. They belong to these teams and play the role of reporters and interpreters in patient management. Specifically, they take the clinical history and conduct physical examinations of all patients assigned to their team.
For psychological safety in NPL, family medicine residents and teachers encourage open communication and active listening, creating a safe space, providing constructive feedback based on learners’ characteristics, and promoting a learning culture18. They actively encourage medical students to speak up, ask questions, and share their opinions. They listen to the students and respond to their questions and concerns with respect and without judgement, to create a safe space in which they can make mistakes and learn from them. They provide students with regular and constructive feedback during discussions and conferences to promote a culture of learning that values continuous improvement, and encourages them to take risks and try new things. They respect the diversity of students and provide feedback to refine their medical skills and attitudes through weekly reflections.
Data collection
Ethnography: Ethnography was employed to investigate the research purpose. Two researchers (RO and TK) acted as participatory investigators. All medical students, junior residents, and family medicine residents who participated in the educational curriculum were informed of the study’s purpose, and written consent was obtained before the observation. RO worked in all hospital wards, observed interactions among medical students, junior residents, and family medicine residents in each ward and conference, and took field notes during the observations. TK communicated with the participants regarding their learning in the educational curriculum, and investigated their difficulties and growth daily.
Once a week, RO and TK discussed the participants’ learning in the curriculum. RO reviewed the field notes on participants’ concrete difficulties and growth in clinical situations and enquired whether TK had discussed this in his dialog with the participants. Moreover, RO and TK shared their perceptions about the participants’ learning and growth through these weekly discussions. They reflected on their observations, and discussed the participants to understand their learning in CBME with NPL. The discussion contents were noted by RO for profound observation and semi-structured interviews.
In the final week of the curriculum, each participant presented their learning to the members of the community care department covering four topics: their growth, drawbacks, emotions/feelings, and next steps. RO and TK listened to the presentations, and subsequently discussed their learning in the curriculum with the participants and its impact on their psychological safety.
Semi-structured interviews: RO interviewed all participants in the hospital conference room on the final day of their curriculum. The interview guide included four questions: ‘What did you think of your participation in the team?’, ‘How did you evaluate your learning in terms of participation in the team?’, ‘How do you evaluate the difficulties of participating in a team?’ and ‘Do you have any ideas on how to improve your team participation?’ Through the interviews, RO reviewed the field and discussion notes, and enquired about the changes participants experienced from the curriculum with respect to their psychological safety. Each interview, which lasted approximately 30 to 60 minutes, was recorded and transcribed verbatim. After each interview, RO and TK discussed the participants’ learning and psychological safety as well as their learning processes.
Data analysis
An inductive grounded theory approach was used in this study20. After reading the contents of the field notes, conducting semi-structured in-depth interviews, and holding discussions with TK, RO coded the content and developed codebooks based on the repeated reading of field notes as the initial coding for reliability. This study used the process and concept coding method21. RO and TK discussed the initial coding by reviewing field notes and interview contents until a consensus was reached. Then, RO induced, merged, deleted, and refined the coding, creating concepts by going back and forth between the research data and the initial coding, for axial coding. The axial coding focused on grouping tentative concepts and creating tentative themes accompanied with refining the codes, concepts, and themes. For triangulation, RO and TK discussed concepts and themes. The interview contents were analyzed iteratively during the research period after completing each participant’s CBME training for theoretical saturation. Finally, the theory was discussed by all the team members (RO, TK, CS), who agreed on the final themes.
Reflexivity statement
This study’s results were co-created by researchers and participants through interactions. The research team members possessed diverse expertise and perspectives related to rural medical education. RO is a family physician and medical teacher, with a master’s degree in medical education and family medicine, and experience in working, education, and qualitative and quantitative research, including grounded theory approaches in rural contexts. TK is a hospital clerk with a master’s degree in medical education and works at a rural hospital, where he managed medical students and residents for 10 years. TK also had experience with qualitative research analysis in rural contexts. CS is a medical educator and professor at a medical university, and specializes in community healthcare management, education, and research. To prevent biases, the research team discussed the findings from individual data analyses and explored alternative viewpoints during the process of making meaning of the data.
Ethics approval
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of Unnan City Hospital (protocol code 20220004; date of approval: March 2021). Participant anonymity and confidentiality were ensured throughout the study. All participants provided written informed consent before participating in the conferences and being interviewed.
Results
Results of the grounded theory approach
Three themes were identified using the grounded theory approach: facilitating learning, change in perception, and change in learning (Table 1).
Initially, the participants were nervous because they had not actively participated in patient management when training at their universities and hospitals. NPL facilitated their engagement in clinical practice. Residents and teachers of family medicine treated participants as team members. Constant reflection supported their learning, motivation, and participation. Furthermore, the acceptance from other healthcare professionals motivated them to actively learn.
Learning in an NPL-based team changed the participants’ perceptions of learning in CBME. They felt a sense of ownership of their patients’ management through discussions with their team members. They also felt safe because of the realization that they were recognized as team members. Participation increased their interest in collaborating with physicians.
NPL-based CBME changed participants’ learning behaviors. Through constant reflections with residents and teachers, they were able to control their motivation to learn medicine. By understanding their learning characteristics, they realized the importance of learning at their own pace. Through apprenticeship and legitimate peripheral participation (LPP), the participants observed the learning methods employed by residents and teachers and understood how to adjust their learning to fit the setting and patients (Fig1).
Table 1: Results of the grounded theory approach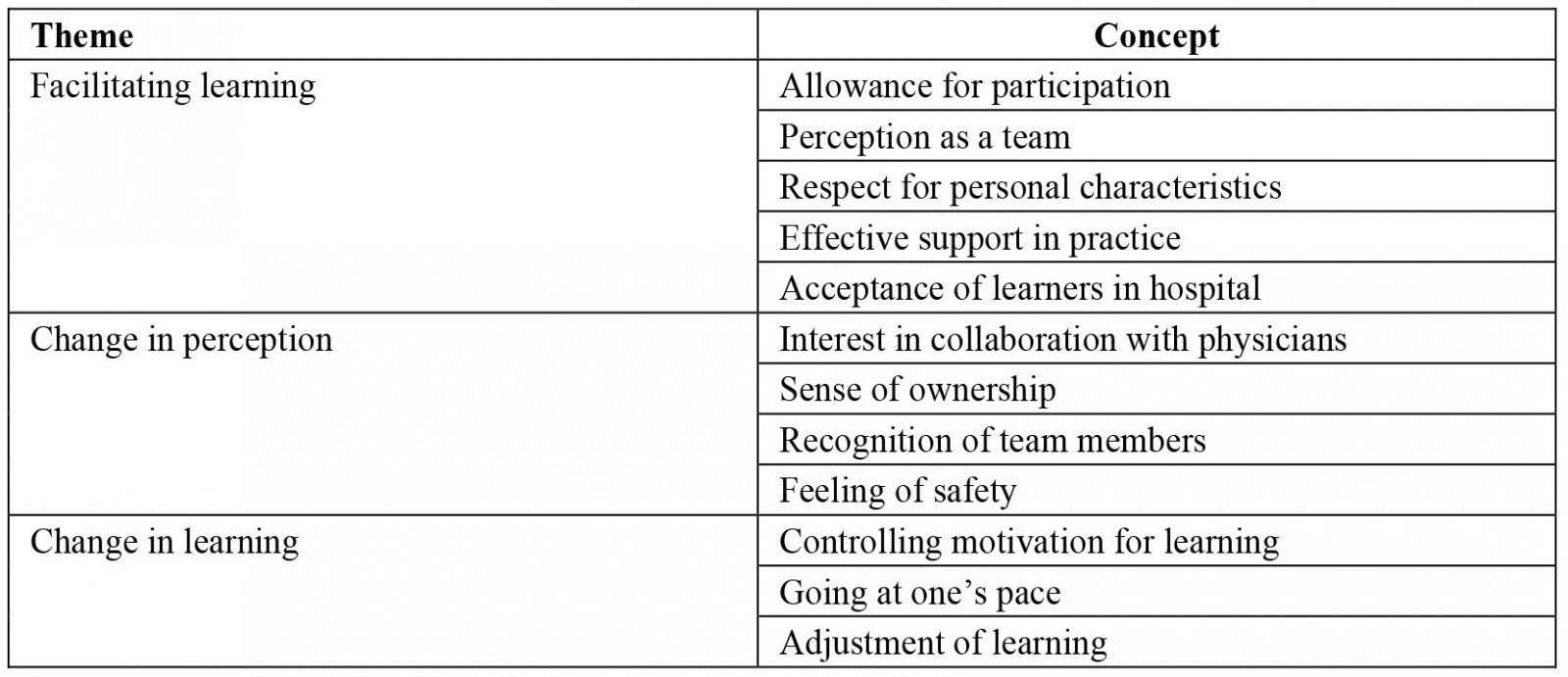
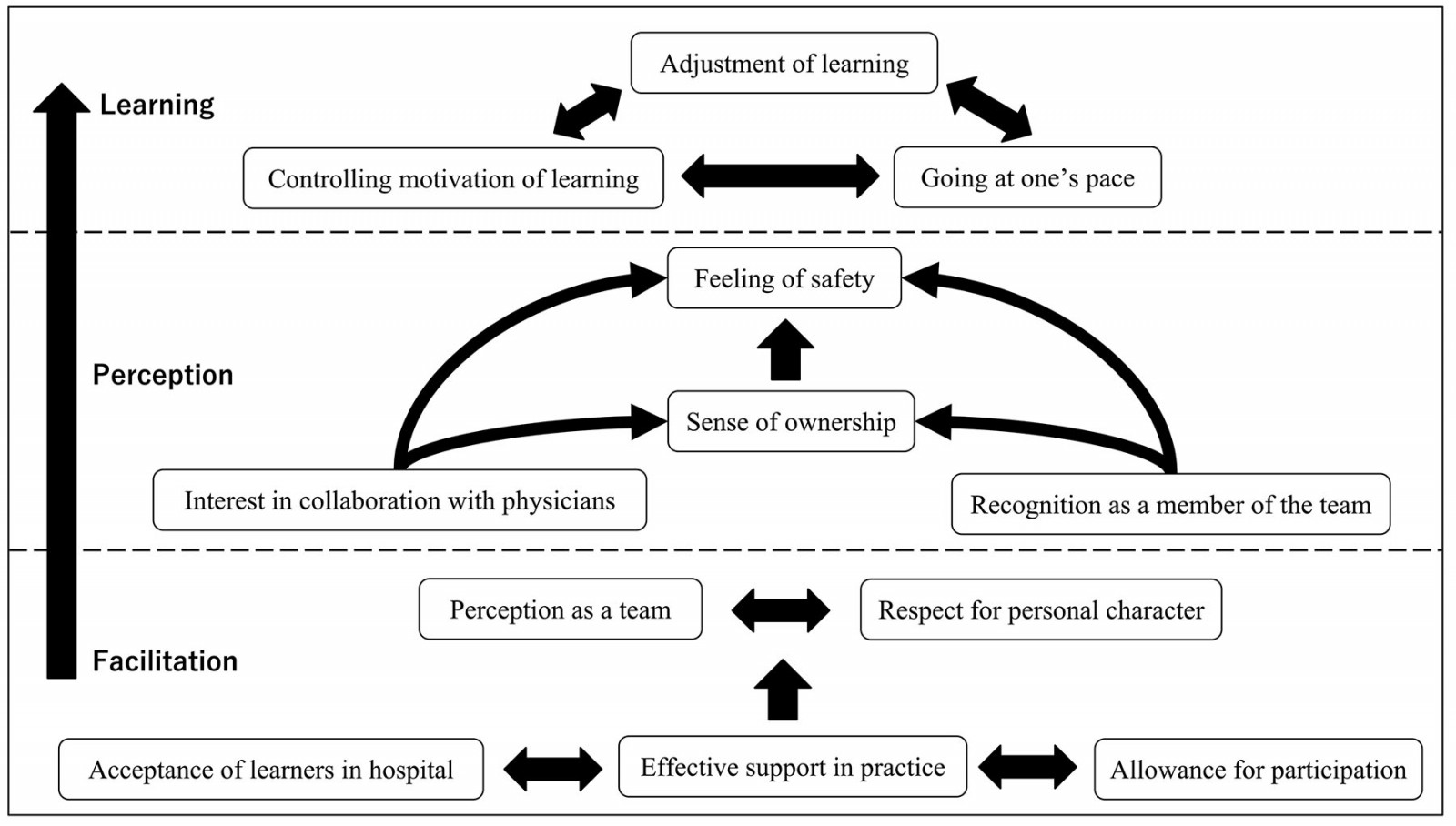 Figure 1: Conceptual figure of learning in community-based medical education based on near-peer learning.
Figure 1: Conceptual figure of learning in community-based medical education based on near-peer learning.
Facilitating learning
The attitudes of family medicine residents and teachers were an essential factor for effective participation. Initially, participants were nervous because they considered their participation limited to universities and hospitals. Residents and teachers encouraged them to participate in team-based treatments. Medical student 11 stated:
I was nervous about learning here because family medicine deals with many kinds of medical conditions, and I had not done anything like that. But the residents and teachers encouraged me to gradually participate in the teamwork for treatments.
Medical student 2 stated, 'The residents and teachers were very friendly and open-minded, so I could say any stupid thing about medicine. They answered my questions sincerely, and continuously learned with me.' NPL helped participants feel that they could participate in clinical medicine and be members of the team. Residents and teachers of family medicine treated participants as team members.
Constant reflection supported participants’ effective learning in NPL. They considered that learning in clinical medicine must follow teachers’ directions. However, NLP and constant reflection effectively supported their individual motivations and participation. Medical student 16 stated:
Every day, the residents or medical teachers helped me reflect on my experiences of the day. By reflecting, I was able to discover a way of learning based on my character.
Participants could reconsider their learning methods based on their previous experiences and new cases with the support of residents and teachers. Junior resident 4 stated, 'The teachers supported me in everyday learning. They did not enforce any way of learning. I could learn various cases at my pace with my way of learning.'
Furthermore, other healthcare professionals’ acceptance motivated participants to learn actively. Junior resident 1 stated:
This community hospital has various healthcare professionals supporting our education. In hospital wards, nurses know me and support my activities. The clerks are also friendly and support me in learning. I could learn safely and comfortably here.
The hospital’s acceptance was crucial to participants’ learning. The learning environment in the community hospital facilitated their participation, allowing them to feel safe.
Change in perceptions
The residents or medical teachers helped participants reflect on their daily experiences. By reflecting, they could understand their way of learning based on their individual characters. Participants were initially embarrassed in such a setting, because it differed considerably from previous educational environments. However, continual involvement and discussion with the residents and teachers changed their perceptions. Medical student 2 stated, 'I did not think that the residents and teachers would be so close to the medical students. I had not discussed medicine with medical teachers because there was a big gap in clinical experiences.' Medical student 3 stated, 'I could discuss my patients’ conditions with the residents. They might consider the discussion too easy, but I was amazed that they discussed matters seriously and openly.' NPL in CBME motivated participants to actively discuss their learning with physicians.
The perception of learning in CBME and their continual involvement in practicing as team members changed their perception of their allocated patients. Through discussions with team members, participants felt a sense of ownership in managing their patients. Junior resident 8 stated, 'The teachers always asked for my ideas about patient management. I had to consider the patients’ management continuously and seriously. It was a bit tough, but I trusted myself.' Moreover, participants realized that they were team members involved in learning. The sense of being a member motivated them to learn and discuss their clinical questions with residents and teachers. Medical student 6 stated:
The feeling of membership was strong in this CBME. I felt respected as a member and discussed my patients’ conditions openly with the residents. This learning environment encouraged me to learn more.
Psychological safety was created during rural CBME learning. The participants felt safe after realizing that they were recognized and respected as learners and members of the team. Junior resident 3 stated:
I could learn freely in this CBME. The residents and teachers supported me a lot in learning. I did not become nervous and confessed my difficulties honestly. I feel a kind of safety in such learning situations.
Recognizing participants as learners and members of clinical teams fostered their perception of such educational situations as being psychologically safe.
Change in learning
Through learning in NPL-based CBME, participants changed their learning behaviors. They controlled their motivation to learn medicine through discussions and reflections with residents and teachers. Medical student 7 stated:
The discussion with residents is useful for my learning. I could learn different methods to stimulate my motivation. Through reflection, I understood that my motivation could be driven by realizing my drawbacks and taking the next steps to learn.
Medical student 2 stated:
My motivation initially decreased in this training. But, through this training, I was motivated to learn medicine by experiencing various real cases. Reflecting on the realization of my motivation, the teachers increased my clinical experiences.
Continuous reflection enabled participants to notice their learning characteristics and use them in CBME. Junior resident 13 stated, 'In every reflection, the medical teachers and residents told me to consider that my learning functioned well. They said that I could learn using my methods of learning here.' The participants considered their learning methods in various clinical situations. Medical student 19 stated:
I have never considered in depth how I could learn in clinical situations. Through the experiences and reflections here, I was able to understand that I might get tired in some situations and not notice my fatigue until I nearly burnt out. I learned that I could control my learning and burdens to prevent burnout.
Junior resident 9 stated:
I was able to say that I cannot do more now. Whenever I was asked, I tended to say that I can do it. However, this trait might have impinged my learning. Through reflection, I noticed it.
Participants noticed the importance of their learning methods and characteristics. By understanding their learning characteristics, they realized the importance of learning at their own pace in clinical medicine for effective and continual learning.
The participants realized the importance of adjusting their learning methods, although they experienced some difficulty in learning clinical medicine using their methods. Through apprenticeship and LPP, the participants observed the learning methods of residents and teachers, and understood how to adjust their learning to fit their situations and patients. Medical student 15 stated:
I tried to learn everything I experienced. I checked textbooks a lot but could not complete everything. I was a bit depressed. However, through reflection and observation of the residents, I realized that I should change my thoughts, know the limitations in my learning methods and adjust my aim to learn.
Junior resident 11 stated:
Learning here was challenging for me. The amount of clinical exposure was huge, so I could not absorb all the content. Observing the residents was beneficial for me. The residents had the same difficulties but adjusted their aims to learn and focused on a realistic way of learning, not absorbing all the contents of their experiences.
The participants learned the importance of adjusting their learning methods and their concrete aims of learning through observation and reflection.
Discussion
This study clarified the specific learning processes in rural NPL-based CBME. NPL facilitated participants’ engagement in clinical practice. Constant participation and reflection supported their learning, motivation, and participation. Furthermore, other healthcare professionals’ acceptance motivated the participants to learn actively. Based on NPL, by learning in a team, discussing with team members, and realizing that they are recognized as team members, the participants felt safe, had a sense of ownership in their patients’ management, and an increased interest in collaborating with physicians. Furthermore, this changed their learning behaviors. Participants could control their motivation to learn medicine, realized the importance of learning clinical medicine at their own pace, and understood how to adjust their learning to fit their learning situations and patients.
NPL and medical staff’s attitudes are essential for increasing the acceptance of medical trainees and boosting their active learning in CBME. In this study, the participants were involved in the medical team and were treating real patients. In NPL, dialogue with patients is encouraged for mutual understanding and co-learning within a team. Previous studies have shown that NPL can increase active learning and improve learners’ knowledge and skills in clinical settings22,23. Moreover, medical trainees may be nervous about learning in different training situations, which may impinge their learning24. NPL can mitigate these difficulties by establishing effective relationships with doctors and other medical professionals in learning contexts25. As this study shows, medical trainees can reduce learning difficulties, and effectively and actively participate in medical training through NPL with respect for the professional workings. For effective initiation and learning in rural CBME, such NPL is critical and should be applied in various contexts.
Medical facilities’ acceptance of trainees is also essential for effective initiation and learning in rural CBME. In rural contexts, the relationship among medical staff is strong, which is critical for working effectively in outpatient and inpatient departments26. Medical trainees need to establish effective relationships with various medical professionals for effective learning27. Our study demonstrates that medical trainees were not stressed in their learning processes. Team involvement through the experience of NPL and the acceptance of medical trainees from hospital administrators about their medical training can explain this perception28. NPL can facilitate medical trainees’ participation in medical care. Therefore, their behaviors, supported by medical teachers in hospitals, directly affect patient care, which could be acceptable to other medical staff29. In addition, this study’s hospital had a long history of providing medical training to medical students and junior residents. Thus, hospital administrators and clerks were accustomed to accepting them and supporting their work and training within medical teams30. NPL can validate medical trainees’ activities, and the hospital’s acceptance of these trainees can be improved through continuous medical education in rural hospitals.
Psychological safety can be gradually established by continuously involving medical trainees in medical teams and patient care. Changing perceptions regarding the hierarchical relationship between medical trainees and teachers can be initially difficult9,31,32. However, as our study shows, medical trainees gradually became accustomed to collaborating with family medicine residents and teachers by overcoming their perceptions from previous learning contexts. This change can be supported by continual reflection and support for medical trainees’ participation in patient care. Continual reflection drives medical trainees’ participation in medical care and reduces the gap between trainees and teachers33,34. As this study shows, continual participation in patient management as a team member based on cognitive apprenticeship and LPP can make medical trainees feel a sense of ownership over patient care, which can improve their engagement in CBME35,36. Previous studies have shown that enhanced engagement in medical education can improve medical trainees’ psychological safety35,36. Improving their engagement and psychological safety can improve learning quality and patient care at medical institutions37,38. This study shows that this process can be driven by NPL-based CBME.
Respecting medical trainees’ learning interests and allowing them to observe family medicine trainees’ and teachers’ attitudes toward learning can make them self-regulated learners39. Controlling learning motivation is essential for continuous professional development40. As our study shows, continual reflection can support medical trainees’ learning motivation by respecting their individual learning interests. In medical education, trainees tend to lose focus on learning because of the overwhelming amount of medical information they are required to learn in clinical practice41. Medical trainees should reflect on their learning methods and focus41,42. As our study shows, reflection can facilitate learning within their control and help medical trainees learn at their own pace.
Furthermore, training with family medicine residents and teachers based on cognitive apprenticeship and LPP enhanced trainees’ adjustment to learning. They were able to monitor their progress and reflect on the effectiveness of their learning approaches using medical teachers’ support28. The trainees viewed their training as enjoyable and worthwhile. In addition, for self-regulated learners, engagement in and persistence with learning behaviors maximizes the degree to which learning occurs43,44. In this rural CBME, participants acquired specific methods of self-regulated learning by observing residents’ and teachers’ discussions and dialogs about patients and their problem-based learning. Self-regulation can be achieved through lectures and experienced learning43,44. The improvement of self-regulation in learning can occur during the progression of careers, and is driven by the facilitation of impressive clinical experiences and mentors45,46. This study suggests that rural NPL-based CBME can provide specific experiences for self-regulation through case-based cognitive apprenticeship and LPP, supported by continual reflection.
This study has several limitations. The first issue is participants’ motivation to learn about family medicine. In this study, we clarified the learning processes of multiple participants using iterative data collection. Another limitation is its transferability, because this study was performed in only one rural Japanese hospital. We used iterative data analysis and collected data over a long period to improve the reliability. Future studies should investigate effective educational methods in other regions and international contexts, using this theory. Additionally, the first author coded the interview data, which might have affected the credibility of the study. To improve research quality, the second author reviewed the processes of coding, concepts, and themes through theoretical triangulation. Lastly, this study shows only the qualitative results of NPL in a rural context, therefore future studies should investigate the change in psychological safety of medical trainees using quantitative methods.
Conclusion
Rural NPL-based CBME can drive medical students’ and junior residents’ engagement in clinical practice through constant participation and reflection. Respecting and supporting each learner’s motivation and participation, and effectively accepting them as team members, helps them feel a sense of ownership and psychological safety. Furthermore, rural NPL-based CBME can support learners in becoming self-regulated. Rural CBMEs may lack healthcare and educational resources. However, implementing NPL in rural CBMEs can make rural medical education more sustainable. Effective rural CBMEs can increase the motivation of healthcare students and the number of medical staff working in rural contexts.
Acknowledgements
We would like to thank all the patients who participated in this study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The authors declare no conflicts of interest.
Data availability
The datasets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.

