Introduction
In Canada, the 18.7% of the population that is rural1 is served locally by only 12.8% of family physicians and 2.2% of specialists2. Rural areas, clearly underserviced by physicians, are challenged with a population known to generally be older, poorer and sicker than the urban population3, along with poorer patient access to care, an undersupply of healthcare professionals in general, and limited hospital resources4. Although medical students and early-career medical graduates interested in or already practicing rurally have been reported as being attracted to the wide scope of practice and have perceptions of tight-knit communities with strong connections and need for rural generalists5-7, the challenging conditions faced by rural physicians have resulted in a struggle to fill rural practice openings. Between 2018 and 2022 this has resulted in a decrease in the number of rural physicians in some parts of the country8. The overall decline in MDs per capita8 and unfilled family medicine residency spots9 in Canada suggests that the challenges will continue to get worse, at least in the short term.
Over the years, a body of research has developed in response to the need to attract and retain more physicians in rural family medicine in a number of countries. Much of this research has focused on determining the factors and traits that are associated with medical students and residents choosing to practice in rural settings. These factors include personal aspects such as being raised in a rural setting, financial aspects, family ties, and lifestyle preferences10,11. In addition, rural doctors have been found to have particular mixtures of personal characteristics that appear conducive to managing the challenges of a rural and remote medical career. They have lower harm avoidance, being less anxious, more persistent, as well as having higher levels of self-directedness, which indicate a resilient personality12,13. Medical residents interested in rural practice have also been found to have similar traits14. That said, Eley et al (2019)15 suggests that most medical learners have personalities that are suitable for rural practice.
Being a rural doctor has been described as requiring ‘clinical courage’16, as care provided may at times stretch physicians beyond their formal training. Rural doctors from a variety of countries describe aspects of this clinical courage including the need to be able to accept uncertainty and consistently strive to prepare, understand and make use of the available resources, know one’s limits, and be there for the community as a whole7. It is expected that this ‘clinical courage’ would require confidence and a strong belief in one’s abilities to do what is required in a rural healthcare setting. Such confidence and belief, elements of rural self-efficacy, have been found to be associated with interest in rural medicine and rural practice intent, including in remote and very remote practice17,18 as well as being a significant predictor of subsequent rural practice19.
In considering how to improve the uptake of rural medicine by medical learners, it is important to consider how training and curriculum can influence rural practice intent. Although there have been no studies that we are aware of looking at rural practice self-efficacy at different points in the medical training, it is expected that this measure could be impacted by the medical school experience. Particular aspects of medical education, such as time spent in rural rotations20 and the development of rural medicine confidence18, have been studied and found to encourage rural medical careers. Other aspects of training – including exposure to telemedicine, GP role-models, methods to overcome uncertainty and co-designed medical education – have also been found to explain the perceptions of medical learners interested in rural medicine6.
Training and curriculum are also expected to impact rural medicine competencies, which in turn could be expected to influence rural practice intentions. The College of Family Physicians of Canada proposes 18 competencies in rural and remote medicine for evaluation in its certification, the majority of which are emergency-medicine-based, such as trauma, acute cardiac presentations and urgent respiratory presentations21. However, in their 2018 report, the Collaborative Working Group on the Future of Emergency Medicine in Canada described that those physicians trained in the specialty of emergency medicine did not believe that a general family medicine residency was an effective route to gain the competencies for the practice of emergency medicine22. Even The College of Physicians and Surgeons of Ontario had at one time declared that some family medicine graduates were not prepared for rural emergency medicine23 and suggested a remediation framework but retracted the statement under political pressure. If family medicine residents also believe they are not developing emergency medicine competencies, could this alter their practice plans? Despite the scope of practice inherent in rural medicine, there has been little to no research to date related to the association between specific medical competencies and rural practice intentions.
In the current study, we propose the rural practice affinity model (Fig1) in which general self-efficacy, defined by Bandura as ‘the belief in one's capabilities to organize and execute the courses of action required to manage prospective situations’24, leads to rural practice intentions when mediated by the medical training to develop both emergency medicine competency and rural practice self-efficacy.
In evaluating self-perceptions of competency in rural medicine, we focused on emergency medicine as it is a usual requirement for rural practice and, as previously stated, is a large focus of the College of Family Physicians of Canada’s Priority Topics for the Assessment of Competence in Rural and Remote Family Medicine21. In addition, emergency medicine is perhaps one of the most challenging aspects of rural medicine, at times forcing one to manage critically ill patients with limited resources. Rural practice self-efficacy is also important to consider as competency and confidence can coexist, but they are not synonymous; they measure different characteristics, develop differently25 and in medicine have been found to have a complex and weak relationship26-28. Demonstrating support for the model and understanding the relationship of its individual components to intentions for a rural career offers the potential to influence family physician resident selection, training and recruitment for rural medicine, all with the ultimate goal of improved access to rural health care.
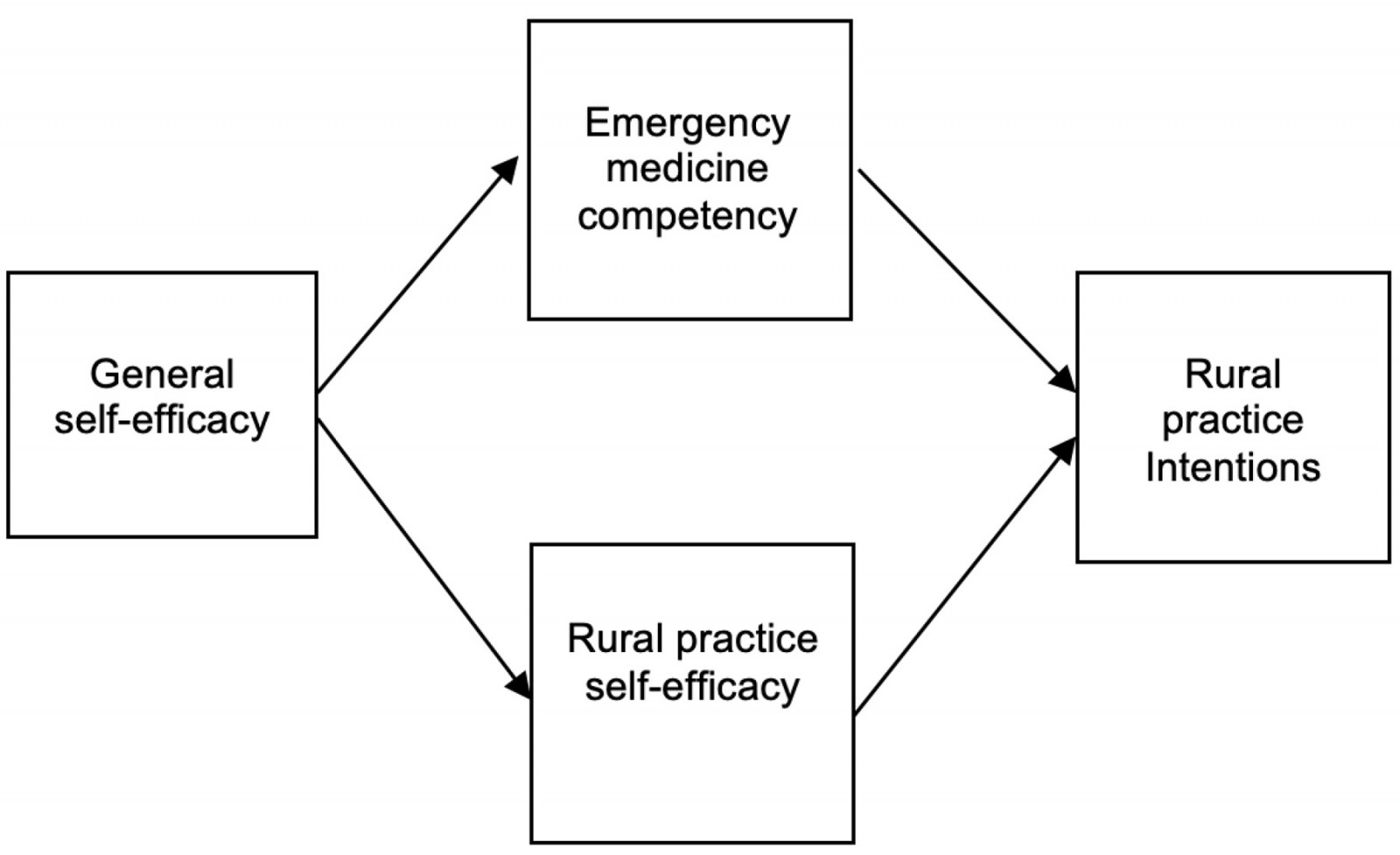 Figure 1: Components of proposed rural practice affinity model.
Figure 1: Components of proposed rural practice affinity model.
Methods
The data used to test the model was obtained via a survey of second year Canadian Family Medicine residents. The survey was created with the Qualtrics software tool (Qualtrics; https://www.qualtrics.com) and was accessed by respondents following an email link. As an incentive, respondents could enter a draw for a CA$300 WestJet gift card, with one draw occurring for each of the Canadian medical schools participating.
A request to participate, along with a survey description and the appropriate research ethics approval, was sent to the academic directors of all 17 Canadian family medicine residency programs. Fourteen approved the proposed research. In 2021, 2 months prior to the usual family medicine graduation date, an email with the survey link embedded was sent to these programs for forwarding to their second-year residents.
Measures
Demographic and data on factors known to influence a rural career choice (personal links to rural communities, relationships supportive of rural practice, and financial incentives for rural practice) were collected and accounted for when determining the strength of the hypothesized relationships.
Model component measures
General self-efficacy
General self-efficacy was assessed using the General Self-Efficacy Scale (GSE) 29,30. The GSE has 10 items, each with four response options (1=‘not at all true’ to 4=‘exactly true’). A sample item is ‘I can always manage to solve difficult problems if I try hard enough’. The scores of each item are added to give an overall score. This scale provides a dispositional measure and, having been formally tested, has been found to measure a unitary concept. The overall score based on the items was used in the analyses.
Rural practice self-efficacy
Rural practice self-efficacy was assessed with a six-item scale. Each item had a five-point Likert-type response scale (from 1=‘strongly disagree’ to 5=‘strongly agree’)18. This scale was created by Isaac et al (2015)18 based on the sources of self-efficacy as described by Bandura. A sample item is ‘I see people like me taking up rural clinical practice’. When internal consistency was assessed, it was noted that the reverse-coding of two items caused the internal consistency of the measure as a whole to drop, which is not an uncommon problem with reverse-coded items31. These two items were removed, leaving a four-item scale. The overall score based on the items was used in the analyses.
Emergency medicine competency
Emergency medicine competency was assessed with a nine-item scale, each with a five-point Likert-type response scale (from 1=‘strongly disagree’ to 5=‘strongly agree’). The scale was developed for this study, with each item being based on a different topic from the Canadian College of Family Physicians’ document Priority topics for the assessment of competence in rural and remote family medicine21. The topics selected for inclusion in the scale were those that pertained most directly to clinical skills, for example ‘I am competent in managing fractures and dislocations’. The overall score based on the items was used in the analyses.
Rural medicine practice intention
Rural medicine practice intention was initially assessed with nine items. One was based on an item from Isaac et al (2015)18: ‘In which geographical location would you most like to practice on completing your training?’ Three were from the SOMERS Index (2011)32, one using a Likert-type scale of 1–10 for the ease of living in a rural area; two items using a Likert-type scale of 0–10 for interest in working in a city environment and intent to work in a rural environment. Two additional items used a five-point Likert-type scale and asked about the positiveness of rural training experience, and the establishment of relationships with specialists that serve rural areas. Two questions asked about the number of months selected to spend in a rural environment during medical school and in residency. Finally, participants were asked whether they were in a rural family medicine residency program. Because of the varied response formats of the items, these nine items were standardized to place them on a common metric. When internal consistency was assessed, it was again noted that the reverse-coded items reduced the internal consistency of the measure. These two items were dropped (SOMERS Index: ease of living in a rural area and intent to work in a rural environment). The remaining seven items formed a cohesive measure of rural medicine practice intention as an overall score that was used in the analyses.
Control variables
A number of variables were measured to statistically control for their effects in the test of the model. Three constructs that have been associated with rural practice intent were assessed. Although individual items made up the scales, the overall scores for the constructs were used in the analyses.
- relationships: a three-item, five-point Likert-type scale (from 1=‘strongly disagree’ to 5=‘strongly agree’) asking if partner (if relevant) is receptive to living in a rural area, degree of family ties to a rural environment, and whether raised in a rural environment.
- financial aspects: a three-item, five-point Likert-type scale (from 1=‘strongly disagree’ to 5=‘strongly agree’) asking about loan repayment programs requiring rural service, financial incentives for rural practice, and adequacy of financial remuneration in rural practice. While these three items had low internal consistency, when combined into a single scale there was small but significant correlation with rural practice intentions
- personal aspects: a four-item, five-point Likert-type scale (from 1=‘strongly disagree’ to 5=‘strongly agree’) asking about rural practice offering work–life balance, sufficient practice opportunities, lifestyle opportunities, and/or a satisfactory social network.
Socially desirable responding was assessed and controlled for with the 13-item short form of the Marlowe–Crown Social Desirability Scale33. Again, several (n=5) items suffered from the reverse-coding problem and were removed from the analysis, leaving an eight-item scale.
Analyses
Model fit testing
A partial correlation matrix between the variables of interest (general self-efficacy, emergency medicine competency, rural practice self-efficacy, and rural practice intentions) controlling for the effects of relationships, financial aspects, personal aspects, and social desirability was created (Table 1) and subjected to a structural equation model using the LISREL (2017) program. The partial correlations ensured that the effects of the control variables were taken into account prior to running the model analyses.
Structural equation modeling is a regression-based approach that analyzes researcher-specified multiple paths between variables simultaneously. One value of this type of analysis is that it provides statistical support (or non-support) for a hypothesized model as a whole. Various fit indices indicate whether the data collected fit the model the researcher has proposed. Ways to improve the fit of the model to the data are also provided as part of the results. Another value of this analysis is that it tests the statistical significance of each hypothesized relationship specified in the model. For models that include a measurement component, structural equation modeling also ascertains the coherence of the measurement aspect of the proposed model. Because our model used single indicators (each construct was measured by its single scale value), this measurement assessment was not part of the model. Another advantage of this type of analysis is that it is possible to assess reverse-flow (eg feedback loops) between variables. However, our model hypothesized all forward-flow relationships between variables.
Table 1: Partial correlations of the rural practice affinity model variables
| General self-efficacy | Emergency medicine competency | Rural practice self-efficacy | Rural practice intentions | |
|---|---|---|---|---|
| General self-efficacy | – | 0.297 | 0.320 | 0.022 |
| Emergency medicine competency | 0.297 | – | 0.357 | 0.327 |
| Rural practice self-efficacy | 0.320 | 0.357 | – | 0.407 |
| Rural practice intentions | 0.022 | 0.327 | 0.407 | – |
Ethics approval
The primary research ethics approval (Romeo File No. 1467269) was obtained from Lakehead University Research Ethics Board.
Results
Sample and descriptive statistics
Approximately 1254 graduating family medicine residents from the 14 medical schools participating in the study received surveys34. Of those, 416 submitted responses for a 33.1% response rate. Seventeen respondents for whom large amounts of data were missing (one or more of entire scales were missing all items) were removed. Mean substitutions were made for three missing data points in the multi-item scales. The results following represent the 399 remaining respondents with little to no missing data.
The description of the sample by age, gender, and medical school are summarized in Table 2. In addition, 373 (93.5%) were graduating in the year of the study and 121 (30.3%) were in a rural family medicine program.
Table 3 shows the scale, number of items, alphas, means, standard deviations, and ranges. Interestingly, neither age (r=0.03, p=0.57) nor gender (r=0.03, p=0.62) was related to rural intent. Thus, these were not included as control variables in the model.
Table 2: Respondent demographics and medical school
| Characteristic | n | % | |
|---|---|---|---|
| Age group (years) | |||
| <25 | 10 | 2.5 | |
| 25–29 | 255 | 63.9 | |
| 30–34 | 96 | 24.1 | |
| 35–39 | 20 | 5.0 | |
| ≥40 | 18 | 4.5 | |
| Gender | |||
| Female | 264 | 66.2 | |
| Male | 132 | 33.1 | |
| Non-binary | 1 | 0.25 | |
| Cis woman | 1 | 0.25 | |
| (Missing) | 1 | 0.25 | |
| Medical school | |||
| University of British Columbia | 55 | 13.8 | |
| University of Toronto | 51 | 12.8 | |
| Dalhousie University | 41 | 10.3 | |
| Université de Montréal | 36 | 9.0 | |
| Université de Sherbrooke | 35 | 8.8 | |
| Université Laval | 29 | 7.3 | |
| McMaster University | 29 | 7.3 | |
| Northern Ontario School of Medicine University | 26 | 6.5 | |
| University of Ottawa | 22 | 5.5 | |
| University of Manitoba | 21 | 5.3 | |
| University of Western Ontario | 19 | 4.8 | |
| University of Calgary | 15 | 3.8 | |
| Memorial University | 11 | 2.8 | |
| Queen’s University | 4 | 1.0 | |
| (Missing) | 5 | 1.3 | |
Table 3: Scale descriptive statistics for model component measure scales
| Scale | Number of items | Alpha | Mean | SD | Range |
|---|---|---|---|---|---|
| General self-efficacy | 10 | 0.837 | 3.19 | 0.34 | 2–4 |
| Emergency medicine competency | 9 | 0.854 | 3.46 | 0.64 | 1–5 |
| Rural practice self-efficacy | 4 | 0.826 | 3.53 | 0.86 | 1–5 |
| Rural practice intentions | 7 | 0.768 | 0.00 | 0.65 | –1.26–208 |
| Relationships – rural | 3 | 0.791 | 2.65 | 1.28 | 1–5 |
| Financial | 3 | 0.336 | 2.01 | 1.54 | 1–5 |
| Personal – rural | 4 | 0.718 | 3.68 | 0.78 | 1–5 |
| Social desirability | 8 | 0.747 | 2.50 | 0.65 | 1–5 |
SD, standard deviation.
Rural practice affinity model fit
Our initial rural practice affinity model resulted in a poor fit of the model to the data (Table 4). Modification indices suggested that there was a significant path from emergency medicine competency to rural practice self-efficacy that should be added for an improved fit. This made sense in that competence in the area highly relevant to rural practice should have a positive effect on residents’ self-efficacy in rural practice. The revised model (Fig2) shows significant paths as hypothesized as well as excellent measures of fit (Table 4).
The paths are noted as beta values (similar in interpretation as are beta values in regression) and their significance is noted by the magnitude of the z-values (above 1.96 is significant). Fit indices should be at 0.90 and above, and the standardized root mean residual should be at 0.05 or below for a good fit of the model to the data.
Table 4: Rural practice affinity model fit statistics
| Goodness of fit measure | Initial model index | Final model index |
|---|---|---|
| Goodness of Fit Index | 0.95 | 0.99 |
| Adjusted Goodness of Fit Index | 0.73 | 0.85 |
| Normed Fit Index | 0.78 | 0.94 |
| Comparative Fit Index | 0.79 | 0.95 |
| Standardized Root Mean Residual | 0.10 | 0.05 |
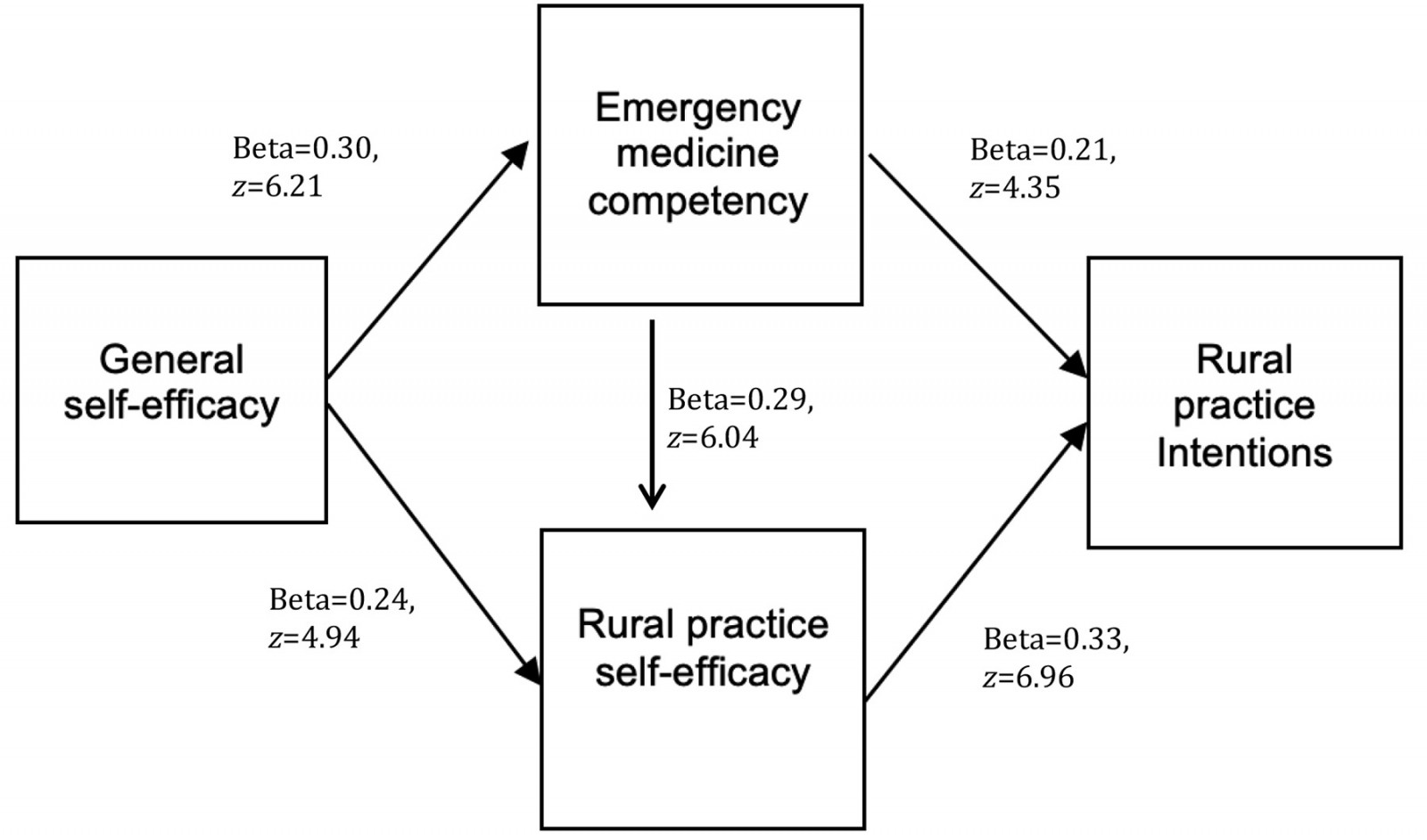 Figure 2: Final rural practice affinity model.
Figure 2: Final rural practice affinity model.
Discussion
While the initial configuration of our proposed rural practice affinity model was a poor fit, the modified model with the addition of the pathway of emergency medicine competency, mediated by rural practice self-efficacy, had excellent measures of fit with the data. The importance of general self-efficacy, a known mediator of personality traits and career intentions35, is recognized and is itself mediated by the more specific rural practice self-efficacy to rural practice intentions, a finding consistent with previous findings in the literature17,18. Furthermore, emergency medicine competency, which has not to our knowledge been previously studied in terms of its association with rural practice intentions or rural self-efficacy, has a central role in both mediating general self-efficacy to rural practice intentions, while also being mediated itself by rural practice self-efficacy to rural practice intentions. The unpredicted pathway between emergency medicine competency and rural practice self-efficacy provides us with some new understanding of the development of rural practice self-efficacy.
The addition to the original model of the path from competence in emergency medicine to rural medicine confidence made sense theoretically, practically, and statistically. The relationship of competence with confidence in medical learners has not been found to be straightforward in studies26-28. However, our study finds a significant positive association between them. This supports the proposed model of competencies that are important in the practice of rural and remote medicine21. Furthermore, the link of emergency medicine competency to both rural practice self-efficacy and practice intentions suggests that this is a curricular area that deserves greater focus and consideration of how to ensure that residents are meeting emergency medicine requirements and receiving robust training in this area. This is especially true when there are significant concerns from various groups on the efficacy of emergency medicine training in family medicine residency, as previously discussed.
It has been observed elsewhere that students encounter fewer patient presentations and procedures than recommended during emergency medicine rotations36,37. In rural settings, encountering all the required presentations may be even more challenging as emergency medicine volumes would be lower than in urban emergency medicine settings. Consequently, consideration may need to be given to alternative ways of ensuring that the required skills are acquired, particularly for learners interested in rural medicine. For example, there is evidence supporting the use of simulations as a way to improve confidence and skills for at least some types of presentations and procedures38-40. Further research is needed to better understand in which aspects of emergency medicine residents feel they require more training to be confident and competent, and the impact of initiatives to improve training. There may also be factors associated with the rural locations, such as remote support from larger centres, that would impact residents’ feelings of emergency medicine competency. While this model included the competency of emergency medicine, future studies could evaluate the relative importance of other competencies as they relate to rural practice self-efficacy and career intentions.
This study has a number of shortcomings. The data are based on a cross-sectional survey and all measures are self-reported. Self-reporting of emergency medicine competency is known to not correlate well when compared with formal evaluations carried out by external observers41. Perhaps the self-reported competency is more reflective of confidence or self-efficacy in emergency medicine rather than actual competency. In addition, since the respondents had not yet graduated, this study measures rural practice intentions that may not reflect the actual outcomes. However, over 90% of the respondents were near graduation and soon establishing their practice location. At this end stage in medical training, intention is the most strongly associated with actual work location (rural/urban)42 and the level of certainty of practice location and specialty is highest, within the order of 70% or higher having a strong certainty43. Unlike other studies that have focused on a single question to measure rural practice intentions18,44, this study incorporates a number of elements into the measure of rural practice intentions that demonstrate previous pro-rural behavior and perceptions, such as time spent in rural placements and positiveness of rural training experience. We suggest that this approach provides a stronger likelihood of forecasting actual future behavior, although this deserves further study and analysis.
Conclusion
Deciding on launching a rural medical career is influenced by many factors, and this study establishes how the relationships between the personal trait of self-efficacy, the medical education outcome of emergency medicine competency and that of rural medicine self-efficacy relate to this professional outcome. The proposed model was supported and should lead us to consider who we encourage to embark in rural medicine and how we support them through their medical education in being successful in this goal.
Funding
This research was supported by the Northern Ontario Academic Medicine Association 2019 AFP Innovation Fund.
Conflicts of interest
The authors declare no conflicts of interest.

