The worldwide shortage of rural medical practitioners has resulted in an increasing number of medical students being trained in country areas. This provides ample access to suitable patients, but the few teachers available are already overstretched and courses of lectures are not possible. Sturmberg1,2 described 'rural based longitudinal' patient-centred learning whereby the student is attached to patients whom they follow through a number of medical and allied health encounters. Such learning is serendipitous, driven by the availability of suitable patients.
The University of New South Wales (UNSW) School of Rural Health (SORH), Australia, provides 25% of UNSW medical students with 50% of their clinical experience in a rural setting. Students attend from Year IV of the 6 year course for a minimum of 18 months. Study in Year IV is directed to medicine and surgery and the developments described here refer to those disciplines. In the city-based schools, Year IV students rotate through a series of 6 week medical and surgical placements backed by courses of lectures. Students assume, in spite of warnings to the contrary in their handbook, these experiences will cover the syllabus.
The SORH integrates medicine and surgery across the whole year using patients as the base for student learning. This patient-centred approach, based on symptom presentation and self-directed learning, supplemented by bedside teaching and tutorials, results in a longitudinal approach rather than systematic blocks of learning experience based on clinical specialties or systems3. Students do not have access to some of the rare and more serious conditions seen in the metropolitan teaching hospital clinical schools, but they see a spectrum of disease far more closely resembling community morbidity. However, it comes to them in an unorganised manner with no relationship to the standard curriculum. Because students are required to adhere to the approved faculty curriculum on which they will be examined, they are anxious that their learning is unstructured; students and teaching staff have expressed a need for some means of tracking their progress.
Students are encouraged to take a certain level of responsibility for their own learning, but they and their tutors need to know what conditions they have, and more importantly have not, seen. When gaps are found, students may be able to fill them by asking their GP, or arranging to attend a specialist's private rooms. Staff also arrange special education days to cover subjects which are important, but not necessarily common. The School assumes responsibility to track clinical experiences4 to ensure a degree of educational consistency among all its students. Other clinical teaching environments have successfully implemented a technological 'encounter tracking' system5-7. In contrast, the SORH initially developed a paper-based system which was cumbersome and later, a Reflective Learning Diary. A student in Albury developed his own system which was popular at that campus, but not generally adopted for technical reasons.
The Reflective Learning Diary was a PC-based application that allowed students to log in and enter details about specific clinical encounters. It attempted to solve the data collection issue and to provide additional functionality by allowing students to enter case history details and to reflect on their clinical encounters. The two functions could not be separated. Because the students found it impossible to write up every case they saw, the tracking function failed and, after a trial, the Reflective Learning Diary project was abandoned.
STRAC - the web-based solution
Before beginning a new development, the School identified the issues surrounding the failure of the dual function Reflective Learning Diary, consulted with academic staff, IT staff and students, and developed a project design that resulted in the STRAC system described here. This was developed solely as a data-collection tool for student clinical encounters. It specifically excluded writing up case histories. The Reflective Case History Template is a separate learning tool described later in this article.
STRAC is a web-based application, which allows students to record their exposure, and rate their depth of understanding of the symptoms, and diseases they encounter while studying at the SORH. It is simple and intuitive to use: an encounter takes less than 30 seconds to enter. Unlike other web-based solutions7 it does not record detailed information about the clinical encounter.
STRAC allows both students and academics to generate reports showing the symptoms and diseases students have encountered, and, more importantly, have not encountered. Individual students can see at a glance how they are progressing, and also view their progress in relation to each other. This also creates an element of competition, which can drive students to repair the gaps in their learning. Reports are submitted to the Learning Management Committee (LMC) on a regular basis. The LMC focuses on the education and curriculum requirements of each campus.
The most innovative aspect of STRAC is the way it presents the various symptoms, conditions and diseases to the students. Using a 'tree' format similar in appearance to Microsoft's Windows Explorer, students are presented with a list of symptoms at the top level of the tree. Figure 1 illustrates this in relation to abdominal pain (tree 1). Clicking this opens the anatomical causes (tree 2): clicking gallbladder reveals three diseases of this organ (tree 3). The student might select cholelithiasis. This encourages the student to think about how they move from the presenting symptom, to the diagnosis. Part of the tree is illustrated (Fig 1).
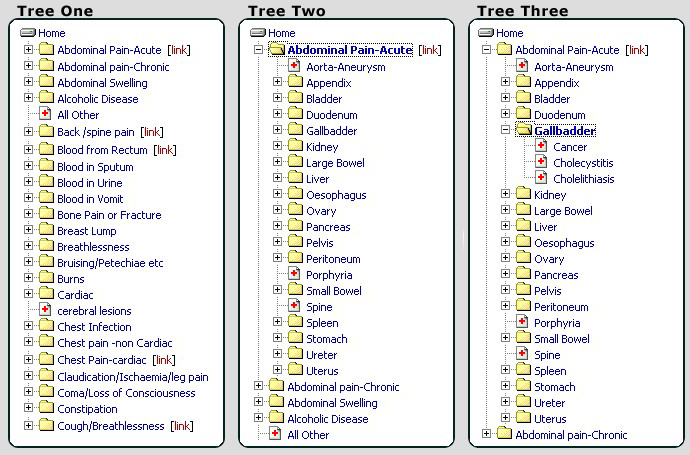
Figure 1: Tree 1 shows the initial state of the 'symptom tree', while trees 2 and 3 show an expanded symptom.
From a student's perspective, entering an encounter is simple. After logging in, students select the required symptom, anatomical structure and disease. Clicking cholelithiases extends the screen to allow the student to enter a rating for the encounter on a scale of 1-10 using a legend provided. This reminds them whether they merely encountered the clinical condition briefly, or examined it in depth. A mouse click enters the encounter. Students can enter optional comments about the encounter, which may be helpful for later review. It is most important for students to understand that their rating is for their own benefit: it carries no assessment weight or value judgement by staff. A student who has merely encountered a condition might enter 2, whereas one who has performed a detailed case write up or presentation might rate themselves 9.
STRAC reports
Progress reports from STRAC (Table 1) are regularly submitted to the LMC which must ensure that students meet the requirements set out in the curriculum, as well as ensuring a degree of educational consistency among all students, in all campuses across the School.
Table 1: An extract from a STRAC summary report
The report shown in Table 1 demonstrates how the LMC is able to analyse the information in a STRAC report. It shows each student's cumulative total for all encounters entered against each listed symptom. The number in brackets shows the number of encounters the student has entered against the symptom and is more objective than the self-rating function. The report also shows an overall group average for the cumulative totals, which helps when comparing the results both within a campus and between campuses.
Overcoming the technological issues
STRAC was able to overcome the issues relating to the Reflective Learning Diary by limiting functionality to one broad goal - a system that allows the tracking of student clinical encounters. This has kept the system quick to load, quick and easy to use, and intuitive.
Students are encouraged to make multiple entries for a single encounter where multiple presenting symptoms are seen, for example abdominal pain and jaundice. Students find that a single symptom may lead them to several diagnoses, a useful insight.
Updating the list of symptoms and diagnoses is simple; STRAC includes a feedback page, as well as a specific form for students to enter a request for a new tree item. Both these forms automatically email the requests to their tutors for consideration, and have been used extensively by the students, with prompt response by staff. The first stage of the tree structure has not increased greatly in scope, but the second and third stages have enlarged slowly in response to student request. This has not slowed the data entry process. Management of upgrades and changes are simple because they only need to be applied to the server, rather than every machine using the software. STRAC is available from any internet connected computer, including home. This has enabled it to be deployed at all campuses. It takes approximately 30 seconds to enter a clinical encounter. Even if students only use STRAC once a week, they can usually enter all their encounters in 5-10 minutes.
Although at present the symptom tree applies to medicine and surgery it could readily be developed for other clinical disciplines.
The Reflective Case History template
The two functions of the original Reflective Learning Diary have now been separated, with STRAC recording encounters and providing data reports and the Reflective Case History Template assisting student learning. Early experience with patient-based learning in Year IV students with limited clinical and self-directed learning experience showed that while they were excited by meeting a wide variety of patients, and used them to a greater or lesser degree as a basis for learning, they were not making optimal use of their clinical experience. Experiential learning on its own is not sufficient, and reflection on the experience enhances its value. To encourage such reflection the School has developed a simple Reflective Case History Template. Students are encouraged to use this regularly to develop their history taking and writing skills and to develop their clinical thinking. Local clinicians and teaching staff, if asked, lament the fact that students and junior medical staff do not know how to write a proper case history. This gave an additional impetus to the development of this simple tool. The fact that students know they will have to write case histories daily as resident medical officers also gives the process substantial validity for them.
The template is designed to prompt reflection at every stage. A small laminated case history outline is provided to students as a prompt for their notes taken at the bedside, encouraging thoroughness. In 2004 a summary of the content of a systems review was added because this is frequently incomplete and confused. At their convenience, students formally transcribe the bedside notes of selected patients onto a Microsoft Word document template that is easy to download for use anywhere. It presents traditional case history headings printed in bold type. As the student types, the headings below move down to make space, so that no restriction is placed on any section. The distinctive feature is that the student is provided with a 'reflection box' at the foot of each section, which poses relevant questions. After the presenting complaint the student is encouraged to reflect: Did I fully explore the presenting complaint? Did I allow the patient to express it in her own word? After physical examination the student is prompted to think about items they forgot, for example I forgot to examine the feet for peripheral neuropathy. Learning needs are identified, and the student is expected to comment on the impact of this disease on this patient. If the write-up is done promptly it can encourage the student to revisit the patient to obtain important information they forgot at the first encounter. They are expected to write a reflective case history once a fortnight.
As an example: a non reflective student new to the process, recorded a patient with 'crushing chest pain similar to the pain of reflux diagnosed 3 months before' but did not ponder how the diagnosis was established and whether it might be wrong. The patient was on treatment for blood pressure, asthma, osteoporosis and reflux but no details were provided and there was no thought that perhaps a beta-blocking drug might be causing the asthma or the treatment for osteoporosis might be causing oesophageal pain. Later the patient's blood pressure (BP) was recorded as 180/105 with no comment that either the BP treatment was not being taken or should be changed.
In contrast, a reflective student used the case write-up of a patient with liver disease to write in detail about liver function tests, and on the difficulties of reducing alcohol consumption in a sales representative; thus ensuring that his learning was firmly based in a clinical context.
The write-up is sent by email to staff for comment made on Microsoft Office 'track changes'. This imposes considerable work on the staff who attempt to respond rapidly, but they feel that the giving of detailed comment to each 'case presentation' is valuable. Students appear to gain greatly from the feedback and are most appreciative of it. It is probable when the system is fine-tuned that later in the year they would gain from critiquing one another's work. This would be educationally sound and reduce the load on busy staff, but it has not yet been introduced.
Summary and conclusions
In the past, the SORH invested significant time and money in attempting to develop solutions to the issue of tracking student clinical encounters, so as to make sure they meet syllabus requirements.
The first computer-based solution required students to reflect on every encounter. This resulted in very low utilisation and caused the instrument to be ineffective as a tracking tool. While further formal research is required, initial feedback from staff and students suggests that by de-linking the two elements, tracking and reflection, both have been enabled to work successfully.
The STRAC solution is simple, user friendly, and feedback has been very encouraging. Students and tutors find the system useful, and continue to use it diligently. The SORH is very satisfied with this innovative approach to helping students better direct their learning. Modification of STRAC may prove a useful way of assisting portfolio management, which is a feature of the new curriculum for the UNSW medical course
While students find that the writing of reflective case histories is hard work, their steady improvement in performance and particularly the increase in reflective comments is obvious to them and to the staff. The use of the system is further reinforced by the fact that a case write-up has become part of faculty assessment in Year IV. The new curriculum of UNSW requires the students to demonstrate capability as a reflective practitioner, and this simple task encourages reflection. Formal evaluation is difficult because numbers are small, resources limited, and a period of profound curricular change is impending. The process is described because it is simple, has face validity, and may prove useful to others.
Practice points:
- Longitudinal, patient-based learning in rural clinical schools requires some method of tracking what students have seen in relation to the syllabus.
- Students must reflect on clinical experiences to optimize their effectiveness. Mere patient encounter is insufficient.
- Developing separate web-based tools for each of these functions appears more successful than attempting to combine them in a single tool.
References
1. Sturmberg JP, Reid S, Khadra MH. A Longitudinal, patient-centred, integrated curriculum: facilitating community-based education in a rural clinical school. Education for Health 2002; 15: 294-304.
2. Sturmberg JP, Reid AL, Thacker JL, Chamberlain C. A community based, patient-centred, longitudinal medical curriculum. Rural and Remote Health 3 210. (Online) 2003. Available: http://rrh.org.au Accessed 9 May 2005.
3. Sturmberg JP, Reid A, Khadra MH. Community based medical education in a rural area: a new direction in undergraduate training. Australian Journal of Rural Health 2001; 9: S14-S18.
4. Sturmberg JP, Crowe P, Hughes C. Computer-assisted instruction: guiding learning through a key features approach in a community-based medical course. Medical Teacher 2003; 25: 332-335.
5. Alderson T St J, Oswald NT. Clinical experience of medical students in primary care: use of an electronic log in monitoring experience and in guiding education in the Cambridge community based clinical course. Medical Education 1999; 33: 429-433.
6. White CB, Albritton TA, Rindt K. MEOW: a web site to improve consistency and communication in clerkships. Academic Medicine 2001; 76: 542-550.
7. Meyer L, Sedelmeyer R, Carlson C, Modlin S. A web application for recording and analyzing the clinical experiences of nursing students. CIN: Computers, Informatics, Nursing 2003; 21: 186-195.


