Introduction
New Zealand (NZ) faces an ongoing geographic maldistribution of its medical workforce and a shortage of general practitioners1. Attracting NZ-trained medical graduates to posts outside of urban areas2 and increasing the popularity of generalist, primary care specialties, such as general practice3, are important steps toward gaining a more equitable distribution of health outcomes for underserved populations in NZ.
In addition to introducing dedicated rural entry pathways 15 years ago, both of the medical schools in NZ have embedded rural immersion programs4,5. These initiatives were predicated on international evidence that students from a rural background, or who have a positive rural exposure during training, are more likely to intend working rurally6,7 , or to practice in rural areas8-11.
Among the aims of rural immersion programs are providing students with insight into rural health, developing skills relevant for rural medical practice, and fostering learning through more continuity with patients and supervisors. Programs typically involve undergraduate medical students living and completing some aspect of their clinical training in a rural setting for a sustained period. The duration of rural immersion is one key factor of program design, as a positive dose–response relationship between the rural exposure duration and the decision to practise in a rural area has been reported10. Longer duration rural immersion programs for Year 5 students have been offered in NZ for more than a decade5,12. Furthermore, since 2012, both NZ schools have offered 5-week, rurally based interprofessional education (IPE) programs 13. While placement in one or both of these immersion programs is limited to a subset of volunteer senior medical undergraduates, most NZ medical students attain at least some experience outside urban centres during clinical rotations in Years 4–6 of their medical studies.
Early reports on the impact of NZ rural immersion programs on student experiences and attitudes toward rural practice are generally in line with evidence from international contexts suggesting a positive influence. For example, University of Otago rural IPE program participants reported an improved understanding of the rural health environment and greater confidence working interprofessionally compared to non-participants13. Similarly, long-duration rural immersion program participants from the University of Auckland reported that their experience confirmed their desire to work in a rural setting and promoted a positive view of the possibility of future rural work14. Yet the impact of rural immersion on NZ students’ rural practice intentions and work outcomes is unclear. One study found that the majority of participants in a long-duration NZ rural immersion program were working (62%) or intended to work (80%) in a rural setting within 4 years after graduation14. In contrast, a study into the impact of the University of Otago’s long rural immersion program reported no difference in the proportion of graduates practising in a rural setting (1–3 years post-graduation) between those who participated in the program and students who did not15.
For over a decade, NZ medical students have been invited to participate in a national longitudinal career tracking study (Medical Schools Outcomes Database and Longitudinal Tracking Project, or MSOD). Participating students complete surveys at entry to medical school, at exit from medical school (graduation), with follow-up surveys in postgraduate years 1, 3, 5 and 82. Having two medical schools in NZ with similar curricula and two lengths of rural immersion program, as well as longitudinal career intention data, presents a unique opportunity to evaluate the effect of rural immersion programs on the career intentions of NZ medical students. The specific aim of this study was to compare the effect of long (>33-week) rural immersion programs, with short (5-week) rural immersion or no rural exposure on student rural career intentions at the completion of medical school, while controlling for other variables associated with rural practice intentions, such as rural background16,17.
Methods
Definition of ‘rural’
The term ‘rural’ is used broadly in the literature to encompass either background or practice outside major urban centres. In NZ, there has been considerable discussion about the best terminology to use in health workforce terms18. There is emerging consensus that it would be preferable to use a three-category framework, namely Urban (population >100 000), Regional (population 25 000–100 000) and Rural (population < 25 000). These are comparable to the Rural, Remote and Metropolitan Areas (RRMA) remoteness classification categories used in Australia19. In comparing the three-category framework to the RRMA framework, Urban encompasses the M1 (Capital Cities) and M2 (Other Metropolitan Centres) of the RRMA categories, Regional is equivalent to R1 (Large Rural Centres) and Rural encompasses R2, 3, 4 (Rural Zones) and Rem1, 2 (Remote Zones)19. Based on the Urban–Regional–Rural framework described, the authors estimate from the 2013 census that approximately 50% of the NZ population are Urban, 16% are Regional and 34% are Rural20. The remainder of this article uses ‘Rural’ to denote a population of less than 25 000 and ‘rural’ to broadly denote non-urban status.
Participants
The participants were medical students at the University of Auckland and the University of Otago who had graduated between 2011 and 2017 and completed both the MSOD Commencing Medical School Questionnaire (CMSQ) and Exit Questionnaire (EQ). Survey responses yielded self-reported data regarding age, gender, ethnicity, population size of origin location (background), population size of the respondent’s intended region of practice (practice intent), specialisation preferences and membership of medical school rural clubs.
Education context and rural immersion program characteristics
The University of Otago has three distinct clinical schools, located in Dunedin, Christchurch, and Wellington, to which students are allocated for the final 3 years of their program. In contrast, the University of Auckland has one clinical school, within which students are allocated each year to one of eight hubs (three metropolitan (Auckland), two other urban (Hamilton and Tauranga) and three regional). Students must complete at least 1 year outside Auckland. For the present study, the rural immersion programs offered between 2011 and 2017 were classified as ‘long’ or ‘short’ based on the length of time for which participants lived in the rural environment. The locations of the medical school hubs and rural immersion programs are shown in Figure 1, and a summary of the characteristics of the rural immersion programs by medical school is provided in Table 1.
Long rural immersion programs are offered to Year 5 medical students at both schools. The University of Auckland’s long rural immersion program (Pūkawakawa) is based in Northland, which has a geographically dispersed population of 151 68920. Students on the program complete clinical placements at Whangarei Hospital, as well as a 7-week general practice/integrated care placement in the Rural areas of Kawakawa, Kaitaia, Rawene or Dargaville. At the time of this study, students completed an application and interview process to secure one of up to 24 places available. Students who had entered medical school via the rural origin preferential entry scheme or the Māori and Pacific admissions scheme received preference for placement on the program5,14. At the University of Otago, the Rural Medical Immersion Program offers placements to 20 students from any of the three clinical schools in Westland, Southland, Tararua, Clutha, Marlborough or Wairarapa. Each of these districts is made up of geographically dispersed Rural centres and, at most, one Regional centre. Students were selected for the program based on their application and a structured interview. At both universities, students who do not participate in a long rural immersion program complete traditional Year 5 clinical placements, including a general practice placement, located mainly in urban settings.
Both medical schools provide an opportunity for a subset of medical students to participate in short rural IPE programs of 5 weeks in duration. The aim of these programs is to provide clinically based interprofessional education that fosters collaborative practice and encourages health professionals to work in rural and primary healthcare settings13. In addition to medical students, students of dentistry, pharmacy, physiotherapy and dietetics participate in the short rural IPE programs. For the purpose of this study, only the survey responses from the medical students who participated in these programs were considered. The University of Auckland IPE program, the Rural Health Interprofessional Programme, is delivered in the Regional centre of Whakatāne. At the time of this study, places on the Rural Health Interprofessional Programme were given to medical students based in that region who volunteered to do the program as a 5-week option during Year 6. The University of Otago IPE program, Tairāwhiti Interprofessional Education, is undertaken by Year 6 medical students from the Wellington clinical school who are allocated to the East Coast region for their GP placement.
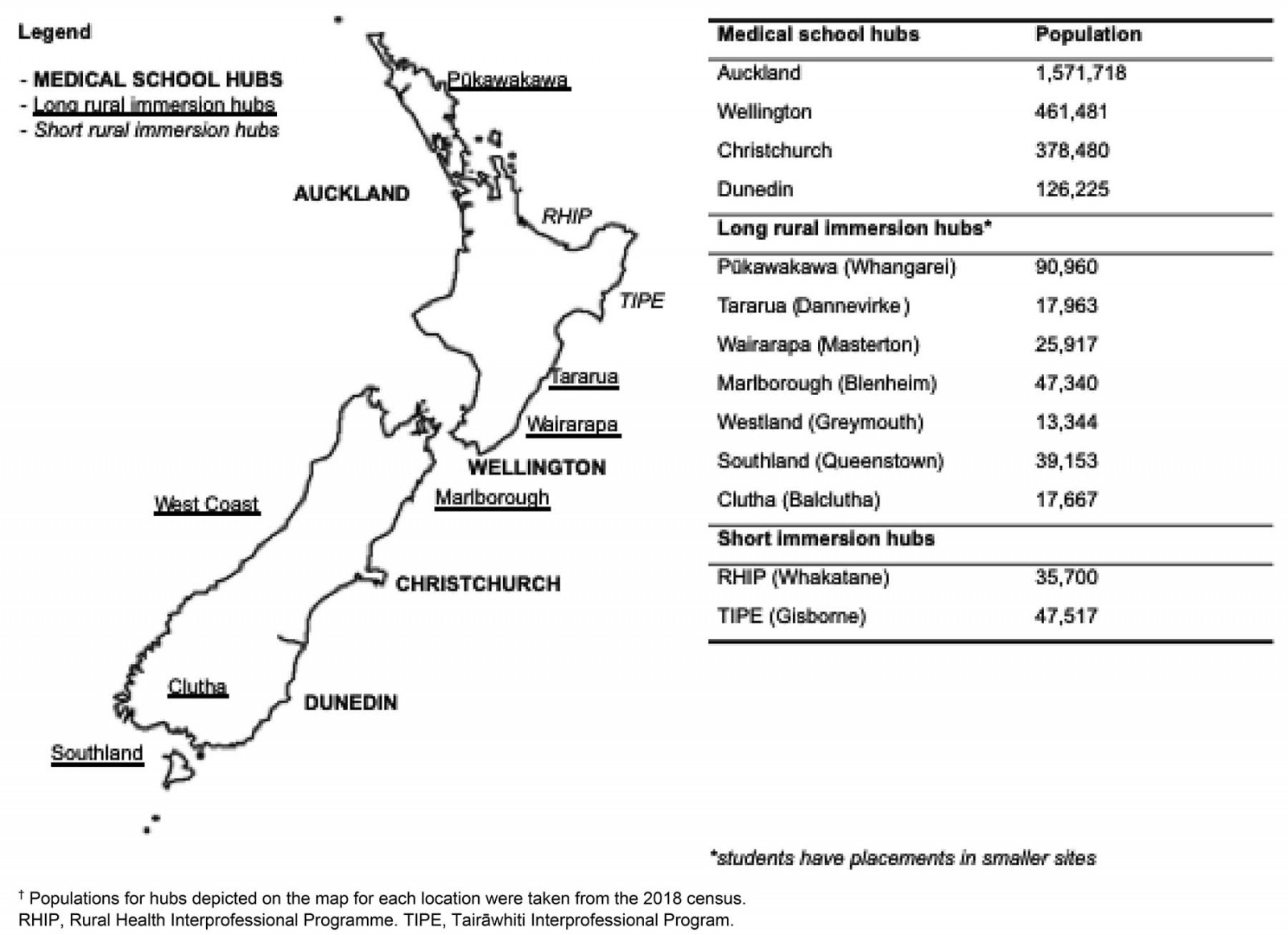 Figure 1: New Zealand map highlighting medical school hubs, long rural program locations and short rural program locations, usually resident populations (table inset).†
Figure 1: New Zealand map highlighting medical school hubs, long rural program locations and short rural program locations, usually resident populations (table inset).†
Table 1: Summary of rural immersion program characteristics by medical school 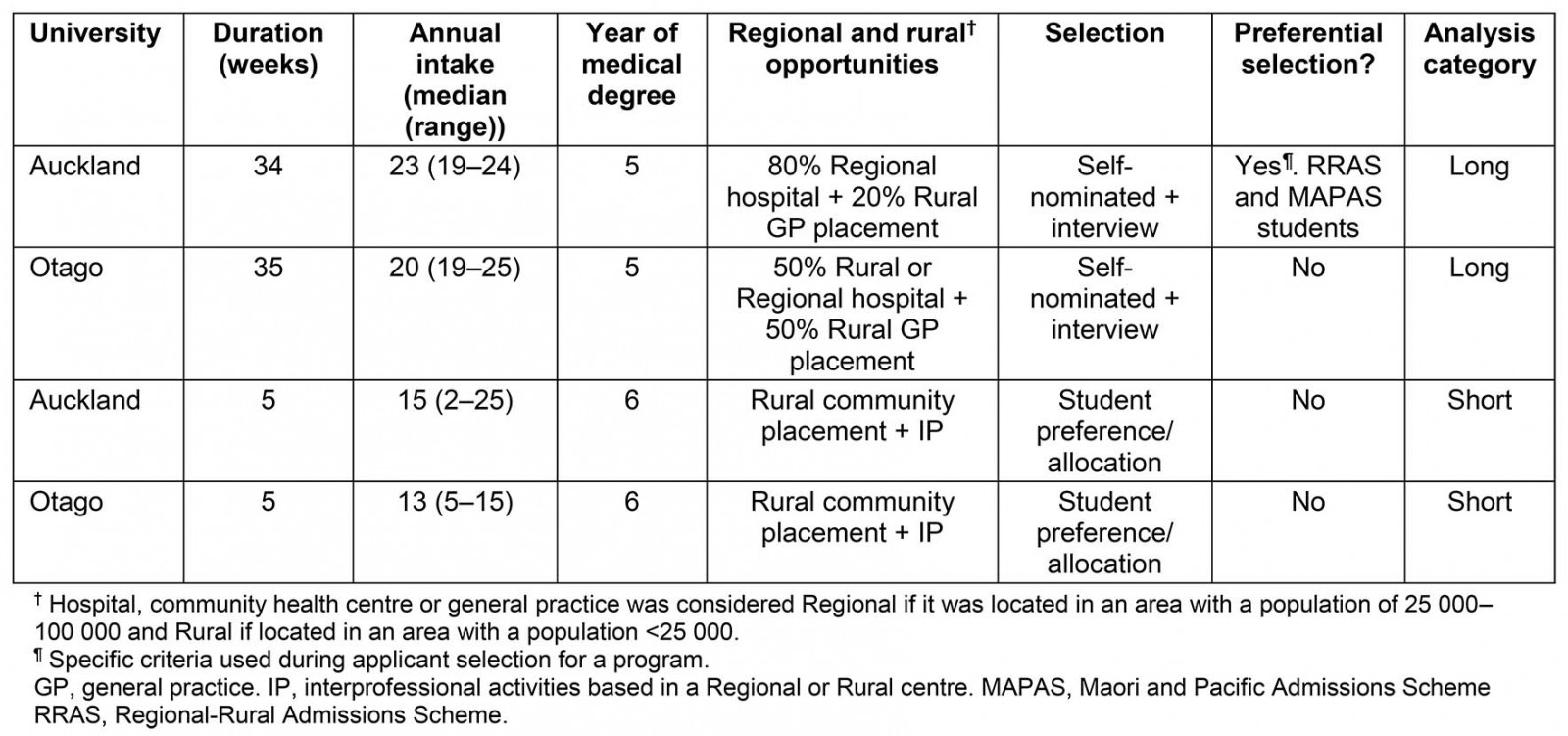
Data pairing
Using Microsoft Excel, participant CMSQ and EQ responses were paired on student identification numbers. Data regarding participation in rural immersion programs were collected from the program office for each school and then linked to the dataset.
Variable selection
Outcome variable: The outcome variable for this study was the preferred location of future medical practice at the end of the undergraduate medical program, henceforth described as ‘exit practice intent’. Exit practice intent was determined from the response to the following question in the EQ: ‘If in NZ, please indicate in which geographical location you would most like to practice’. Students could tick one of five possible options presented on a five-point scale: Major city (population >100 000), Regional city or large town (population 25 000–100 000), Town (population 10 000–24 999), Small town (population <10 000) and Not applicable (not intending to work in NZ). Those who ticked ‘Major city’ were classified as Urban. Those who ticked ‘Town’ or ‘Small town’ were merged into the Rural category. The respondents who selected ‘Regional city of large town’ formed the Regional category. Respondents who indicated no intention to work in NZ were removed from the dataset.
Explanatory variables: A rural immersion variable was derived from the linkage of program participation to CMSQ and EQ data. Students who had participated in Pūkawakawa or the Rural Medical Immersion Programme were placed into the ‘long rural immersion’ category. Rural Health Interprofessional Programme or Tairāwhiti Interprofessional Education participants were placed into the ‘short rural immersion’ category. It was possible for students to have participated in both programs – for the purpose of analysis, these students were placed into the ‘long rural immersion’ category. Those who did not participate in either rural immersion program were placed into a ‘no rural immersion’ category. Variables derived from the CMSQ and EQ that displayed an association with practice intent at the end of medical training14,21 or practice outcomes17 in previous work were retained for analysis. These included age at graduation, gender, size of town/city of background, entry practice intent, first preference for general practice specialisation at the time of graduation and ethnicity. A prioritisation criterion was applied to select one ethnicity if the respondent indicated more than one. From greatest to lowest priority the categories were Māori, Pacific Islander, Other and New Zealand European. The application of this criterion makes no assumptions in regards to the ethnicity that the respondent identified with the most strongly but is a data reduction technique adapted for the ethnicity categories presented in the CMSQ and consistent with that applied by the NZ Ministry of Health22. Both NZ medical schools have student-led rural health clubs that promote rural health and rural health careers. This variable from the EQ (rural club member) was included as an indicator of personal interest in rural medicine.
Analysis and model selection
Univariate statistical significance was analysed with χ² tests for categorical data and one-way ANOVA for continuous variables.
A multinomial logistic regression with response variable ‘exit practice intent’ (Rural/Regional/Urban) was built in the Statistical Package for the Social Sciences v25 (IBM; http://www.spss.com). Factors included ‘rural immersion’ (Long/Short/None), ‘background’ (Rural/Regional/Urban), ‘entry practice intent’ (Rural/Regional/Urban), ‘general practice first preference’ (Yes/No), ‘rural club member’ (Yes/No), ‘gender’ (Male/Female), ‘ethnicity’ (Māori/Pacific Island/Other/NZ European), ‘age’ and interaction term ‘background × rural immersion’. ‘Urban’ was used as the reference category for the response variable. Non-significant factors (p>0.2) were removed by backward elimination to arrive at the final model. Multi-collinearity among explanatory variables was assessed by factorising categorical variables and calculating variance inflation factors. No variance inflation factors greater than 2 were encountered, so the assumption of no multi-collinearity was satisfied. Missing data are reported in the descriptive summary (Table 2), but were excluded in the final multinomial regression model. Statistical significance was set at α=0.05.
Data processing, variable selection and descriptive analyses were performed in Python v3.7 (Python Software Foundation; http://www.python.org) using Pandas23, Numpy, Seaborn, Scipy24, Researchpy and Matplotlib25 packages.
Table 2: Cohort demographics for students intending to practise in rural, regional and urban locations in New Zealand at completion of their medical training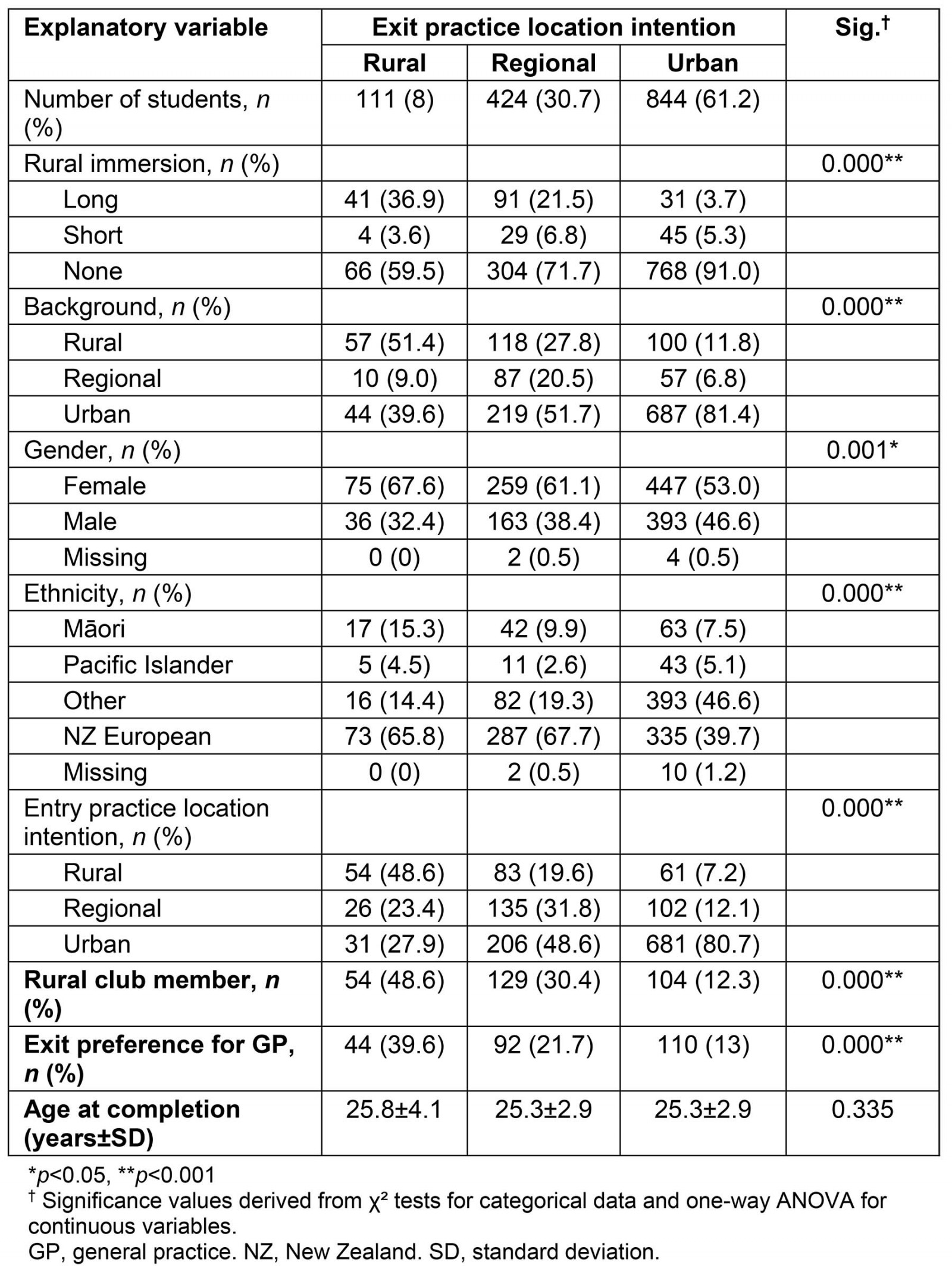
Ethics approval
For each survey, participants provided written informed consent for use of their responses and resulting data by MSOD. MSOD has been approved by the University of Auckland Human Participants Ethics Committee (#8539), and the University of Otago Ethics Committee (#07-155).
Results
Of the 2764 students who graduated from an NZ medical school between 2011 and 2017, 1393 students responded to both a CMSQ and EQ, yielding a response rate of 50%. Respondents were 57% female, 51% had NZ European ethnicity, 9% were Māori, 4% were from Pacific Islands and 36% identified as Other ethnicity. The group of non-responders were 53% female, 54% NZ European, 1% were Māori, 1% were Pacific Islander and 31% Other. Of those who participated in a long rural immersion program, 51.4% completed both a CMSQ and an EQ. For short rural immersion programs this was 47.9%, and for students who did not participate in either rural immersion program the response rate was 45.6%. Participants who completed both the CMSQ and EQ but did not provide either a background location or practice location intentions were removed, resulting in a study sample of 1379 students. Of these, 241 (17.4%) had participated in an immersion program. Of these 1379 students, 12 were excluded from the final multinomial model as they did not provide their ethnicity on the CMSQ or EQ.
Of the total study sample, 111 (8%) were Rural intending at exit, 424 (30.7%) were Regional intending, and the majority, 844 (61.2%) were intending to work in an Urban area. The univariate analysis in Table 2 shows that there are significant associations of career location intention with background, gender, ethnicity, entry location intention, rural club membership, general practice specialty intention and rural immersion experience. Age was the only variable to show no association.
Alluvial plots anchored by rural immersion category (none, short, long) were generated to visualise the flow of students from their background groupings (Rural, Regional, Urban) to their exit practice intent groupings (Rural, Regional, Urban), in an effort to explore whether rural immersion has a varying influence of practice intentions depending on background (Fig2). The width of the ‘stream’ in the alluvial plot is proportional to the number of students within each category, giving visual representation of whether or not the relationship between background and exit intention was modified depending on the length of rural immersion.
Figure 2 (panel A) shows the background and exit practice intent for students who did not participate in either rural immersion program (n=1138). The majority of students from an Urban or Regional background expressed an exit practice intent concordant with their background (77% and 53% Urban and Regional, respectively). Conversely, a minority of Rural background students expressed a concordant exit practice intent (15%), with the majority of Rural background students displaying an Urban exit practice intent (44%), followed by a Regional exit practice intent (41%). It’s worth noting that even though a minority of Urban background students expressed an exit practice intent discordant with their background, these students make up the majority of the Regional and Rural exit practice intent groups. A similar pattern is observed for the short rural immersion program group (Fig2, panel B).
In contrast, Figure 2 (panel C) shows that the long rural immersion group (n=168) comprises a larger proportion of students from a Rural (42%) or Regional (15%) background than the no rural immersion group (17% and 10% Rural and Regional background in the no rural immersion group, respectively). Unlike the group with no rural immersion, the majority of Urban background students who undertook a long rural immersion program (54%) then expressed a Regional rather than Urban exit practice intent. Moreover, a larger proportion of Rural background students expressed an exit practice intent concordant with their background (40%) compared to the no rural immersion group, although the majority still expressed a Regional exit practice intent (50%). Similarly to the no rural immersion group, a minority of Regional background students expressed a Rural practice intent (5%), while the majority expressed a Regional exit practice intent (46%).
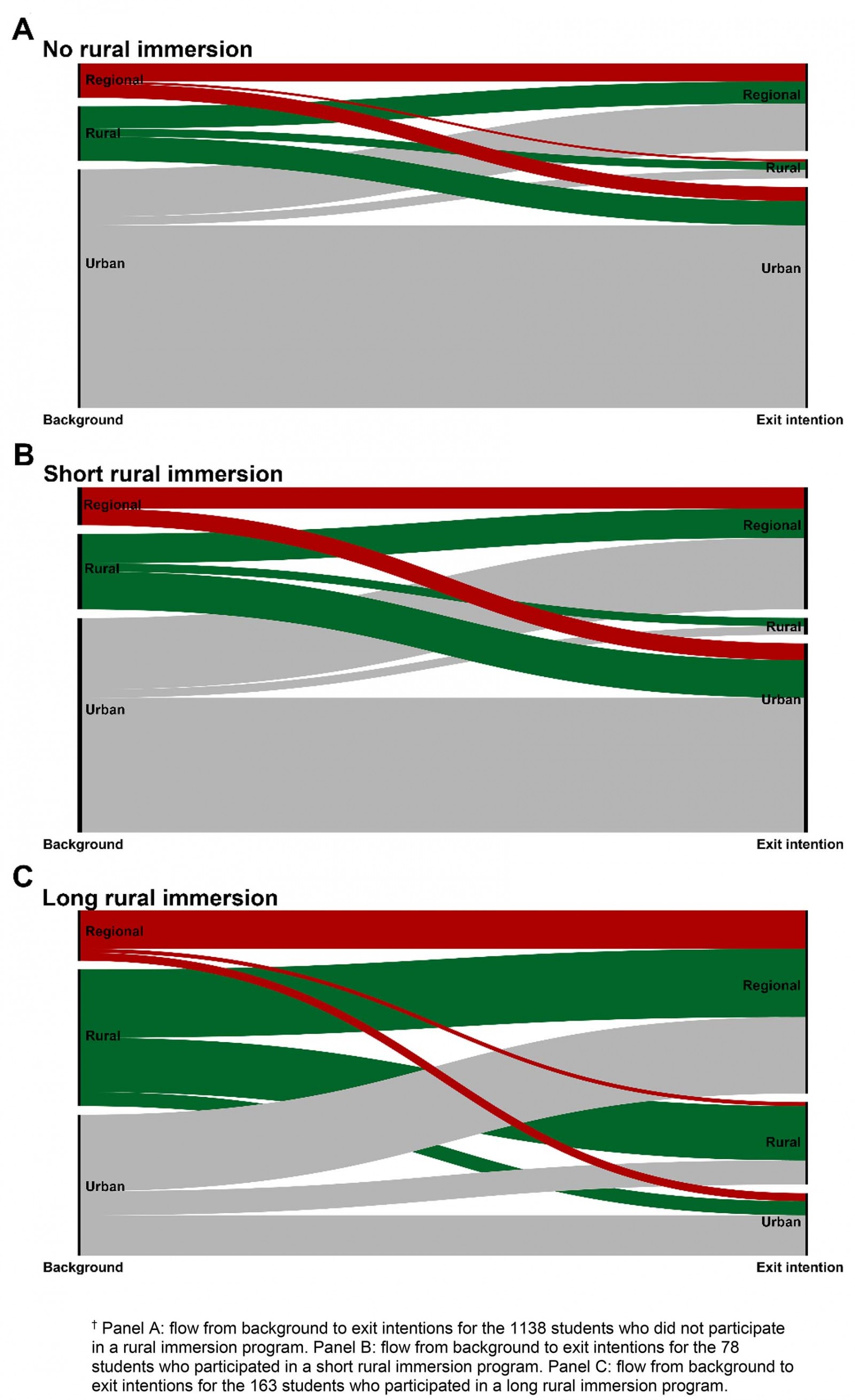 Figure 2: Alluvial plots of student background and exit intention by rural immersion category.†
Figure 2: Alluvial plots of student background and exit intention by rural immersion category.†
Multinomial model results
After backward, stepwise elimination, the final multinomial model consisted of the explanatory variables ‘rural immersion’, ‘entry practice intent’, ‘background’, ‘ethnicity’, ‘rural club member’ and ‘general practice first preference’. Explanatory variables ‘gender’ and the interaction term, ‘background × rural immersion’, failed to attain the significance level required to remain in the final model. The findings from this analysis are presented in Table 3.
Influence of rural immersion on exit practice intentions: Holding all other explanatory variables constant, participating in a long rural immersion program increased a student’s likelihood of having a Rural practice intention at exit, compared to an Urban practice intention, by 6.4 times (p<0.001). Long rural immersion was also associated with an increase in the likelihood of intending to practise in a Regional area at exit, compared to an Urban area, by 4.4 times (p<0.001). Short rural immersion had no impact on exit practice intention compared to no rural immersion (Rural and Regional exit intention relative risk (RR) 0.5, p=0.275; RR 1.2, 0.565, respectively).
Table 3: Multivariate multinomial logistic regression model for exit practice location intention†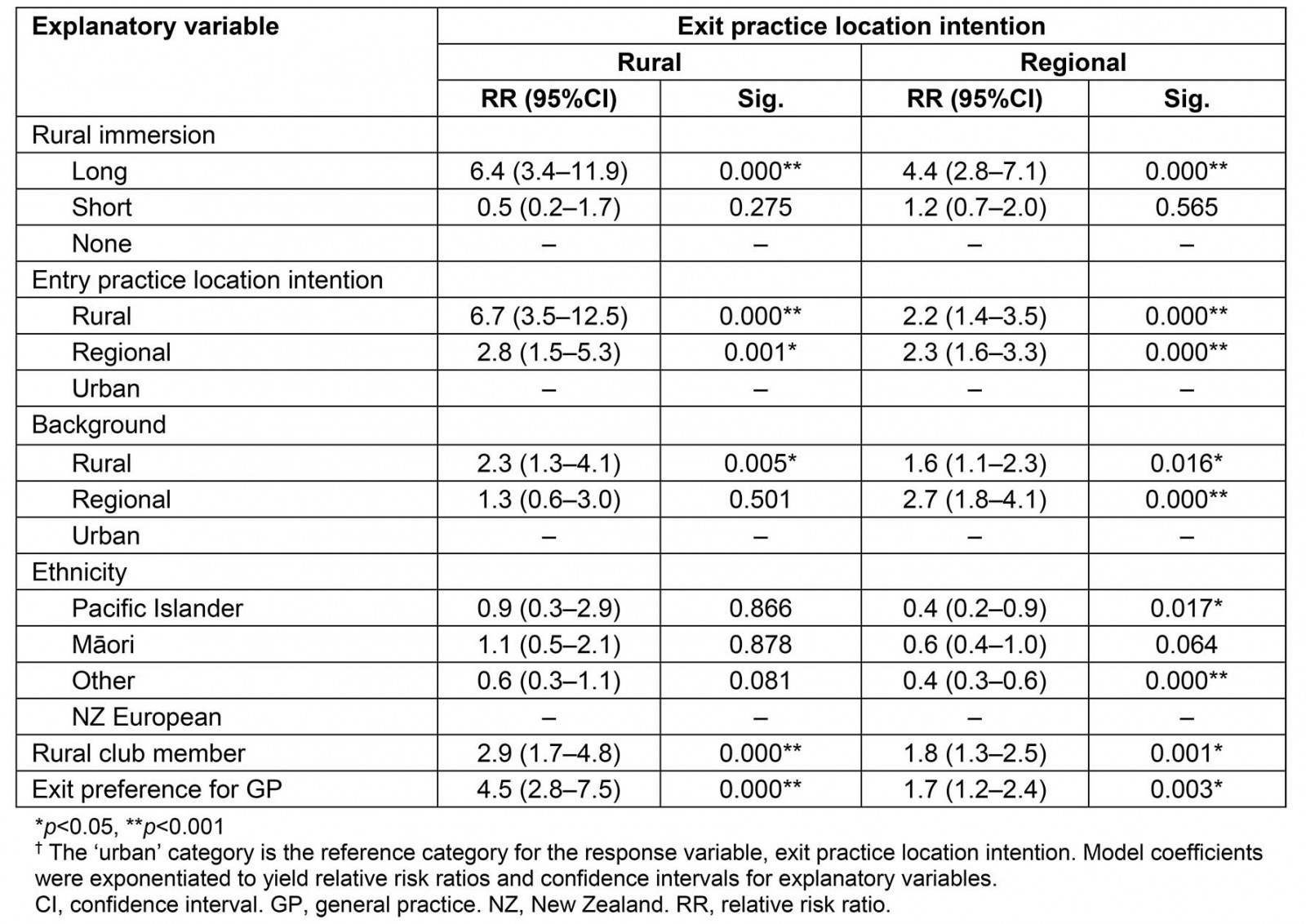
Sociodemographic characteristics of Rural intending students: Compared to students who expressed an intention to practice in an Urban area, Rural intending students were significantly more likely to have expressed general practice as their first preference for specialty (RR 4.5, p<0.001), be a member of a rural club (RR 2.9, p<0.001), have a Rural rather than an Urban background (RR 2.3, p<0.001), and have either a Rural (RR 6.7, p<0.001) or Regional (RR 2.8, p<0.001) practice location intention at entry to medical school.
Sociodemographic characteristics of Regional intending students: Compared to students who expressed an intention to practise in an Urban area, students who intended to practise in a Regional area were significantly more likely to have selected general practice as their first preference than another specialty (RR 1.7, p<0.05), be a member of a rural club (RR 1.8, p<0.05), have a Rural (RR 1.6, p<0.05) or Regional background (RR 2.7, p<0.001), or have had either a Rural (RR 2.2, p<0.001) or Regional (RR 2.3, p<0.001) practice location intention at entry to medical school. Regional intending students were also significantly less likely to have an ethnicity that was in the categories ‘Pacific Islander’ or ‘Other’ compared to having a ‘NZ European’ ethnicity (RR 0.4, p<0.05; RR 0.4, p<0.001, respectively).
Discussion
This study assessed the influence of rural immersion programs on the practice location intentions of more than 1300 NZ medical students who graduated between 2011 and 2017. Graduates who participated in a long rural immersion program were greater than six times more likely than non-participants to be intending to work in a Rural area, and greater than four times more likely than non-participants to be intending to work in a Regional area. In contrast, medical students who completed a 5-week, short rural immersion IPE program were no more likely than non-participants to intend to work outside an Urban area.
The present study adds to the understanding of the relationship between the length of rural immersion during undergraduate training and the odds of a rural practice outcome of medical graduates seen for immersion durations of one academic year (36 teaching weeks) or longer10. For example, students immersed in a rural program for one, two and greater than 2 years were 1.79, 2.26 and 4.43 times more likely, respectively, to be practising in a rural location in Australia compared to students with no rural immersion. Similarly, Playford et al reported that students who had rural exposure through attending a rural clinical school were twice as likely be working rurally than those attending a metropolitan-based clinical school17. The present study found larger relative risk ratios for rural practice intention associated with long rural immersion (6.4) than previously reported; however, it should be noted that the present study examined rural practice location intentions rather than outcomes. The significant independent effect of long rural immersion on student intentions reinforces the design decision regarding program duration that was made in the initial development of the long immersion programs5,12 and justifies the additional investment required to fund such programs.
The finding that short rural immersion had no independent influence on student practice location intentions is in line with research from Canada26 and Australia27, which found that rural immersion placements of a 4-week duration did not increase the likelihood of rural practice. In this case, it is possible that 5 weeks of immersion simply does not provide enough time for students to assimilate and form an emotional attachment to life in a rural area27. The present study’s findings need to be interpreted with caution as the numbers of students in this group was relatively small and the response rate was around 50%. Further, the intent and pedagogy of the short immersion programs in this study differ significantly from the design of the long rural immersion programs, as opposed to being just a shorter version. In the short rural IPE immersion programs the students spend proportionally less time on medicine-specific clinical rotations than in the long rural immersion programs, and a larger proportion of time focusing on IPE learning outcomes, which are essential wherever they practise13. Finally, it is important to note that this finding does not provide any indication of how effective IPE programs may be at influencing the career location intentions of students from other health professions who participate, as it only took into account the intentions of the medical students that participated in the IPE programs. Medical students make up a minority of the entire IPE cohort, with the remaining cohort consisting of a mixture of students from other health professions such as dentistry, physiotherapy or pharmacy. An impact evaluation of NZ IPE programs is currently in progress28 and will provide a more accurate portrayal of the effect of IPE programs on career choices for all health professionals who participate.
A novel feature of this study is the introduction of a three-category classification (Urban, Regional, Rural) for student background and practice intentions. Previous work in the NZ context has used a dichotomous classification (Rural (population <100 000); Urban (population >100 000))29. The adoption of a three-category classification scheme permitted a more detailed analysis, allowing the authors to detect shifts in intentions that take place between the Rural and Regional categories. Similar to previous studies15,29, a significant, independent effect of student background on practice location intentions at graduation was observed that persisted across the three-category classification. Further, the study found that while Rural background is a significant predictor for a Regional practice intention at graduation, Regional background students were no more likely than Urban background students to express a Rural practice intention. This finding supports the affirmative entry pathway into medical school for students from a Rural background, and highlights the importance of selecting students from a Rural background for improving workforce supply to Rural areas, as the Rural exit practice intentions group mostly comprises students with a Rural or Urban background.
Another important finding is that the impact of rural immersion on exit practice location intent was independent of student background, with the interaction term between the two factors failing to attain the significance level required to remain in the final model. This finding was unexpected, given that, first, the University of Auckland preferentially selected students with a Rural or Regional background for the long rural immersion program between 2011 and 2017 (Table 1). Second, a significant positive association between a rural background location and rural exit intention has been reported previously in NZ-based studies29,30. Finally, as illustrated in Figure 2 (panels A and C), a greater proportion of Rural and Regional background students who did the long rural immersion program displayed concordance between their background and intended practice location compared to students who did no rural immersion program. This pattern would be conducive to an interaction effect. However, the interaction effect was likely swamped by the high proportion of Urban background students who displayed discordance between their background and intended practice location after long rural immersion. Nearly three-quarters of Urban background students who participated in long immersion intended to work outside of Urban areas compared with only 23% of Urban background students without long rural immersion. This finding underscores the importance of providing more opportunities, such as long rural immersion programs, to Urban background students wishing to consolidate their Rural or Regional practice intentions. Given that Urban background students form almost 70% of the medical student cohort in NZ, curriculum interventions targeted at generating greater interest in rural practice in this group may have the greatest effect, in absolute terms, on workforce supply to rural areas31.
The present study has several limitations. First, it uses self-reported data and therefore introduces the possibility of social desirability bias. Second, students were not randomly allocated to the rural immersion programs. Students volunteer, or self-select, to go on the rural programs, which indicates a pre-existing interest in rural practice. Furthermore, having a rural background would have enhanced the chances of being selected into the long rural immersion programs, thereby introducing the possibility of selection bias. Third, the rate of students who responded to both the CMSQ and EQ was 47%, and only just over half of the total number of students who undertook a long immersion program were in the study sample. This gives rise to consideration of how representative the sample is, although the authors are unable to think of a plausible way in which non-responders from the long rural immersion group would behave differently to responders. Fourth, the study used length to define the rural immersion variable, and the authors acknowledge there will be considerable differences in the programs, including formal and informal curricula. While it is beyond the scope of this study to evaluate the specific aspects of success, the study findings suggest that having students apply in advance, implying a degree of self-selection, in addition to meeting stipulated criteria, then living in a rural area for a prolonged period, seem key components. Last, this study examined the influence of rural immersion on graduate intentions, not actual practice location. Although there is evidence for reasonable concordance between medical students’ practice location intentions and outcomes32, intentions do not always equate to actual behaviour. As the numbers of students grow over time, as well as the time they may be followed up, the models of rural immersion that are the most important in rural workforce terms will emerge. To this end, the study group plans to collect the first set of MSOD postgraduate year 8 data in 2020, and is starting to link MSOD data systematically with NZ workforce data.
Conclusion
This is the first study from NZ, and among the first worldwide, to use a nationwide dataset to assess the independent influence of rural immersion programs on student intentions while adjusting for key independent predictors of rural practice. A three-category classification for geographic background and career location intention permitted a more detailed understanding of the interplay among demographic variables and rural immersion in influencing career intentions. Medical students who participated in a long rural immersion program during medical training were significantly more likely than those who did not to intend to work in a Regional (population 25 000–100 000) or Rural (population <25 000) part of NZ after graduating. This effect is as marked for Urban background students as it is for Rural students. Given the larger numbers of Urban students, finding those students who are predisposed (eg who had expressed a rural intention at entry), who have GP intentions, or who are members of a rural club, may be a useful strategy in selection into long rural immersion programs. Following cohorts into their postgraduate years is needed to ascertain if these career location intentions persist.
Acknowledgements
The authors gratefully acknowledge the medical students who completed questionnaires, and Professor Sue Pullon (Otago) and Professor Ian Reid (Auckland) who made helpful comments on the manuscript. Yasmine Abid was funded by a University of Auckland Summer Scholarship in 2018–2019.