Introduction
Remote rural locations with low demographic density and large territorial extensions experience additional barriers to ensure access to primary healthcare services, which is more critical regarding specialized care1. The provision of specialized care faces difficulties in financial sustainability, insufficient human resources2, and adequate training to work in the context of rurality, even in high-income countries3.
Long distances with high travel costs and waiting times for specialized care are more severe for the inhabitants of rural areas4 and have been associated with concentration of specialists in urban clusters5. Barriers to specialized care are widespread and multifactorial, with consequences for timely access, health outcomes, and equity in urban and rural contexts6. Even so, few countries have established policies aimed at providing accessible specialized care for rural contexts. For example, Italy has a national policy for remote rural areas to guarantee minimum standards of access and avoid specialized care inefficiency, partly provided in small hospitals3. Australia and Canada have small hospitals under the responsibility of states and territories/provinces, and others, such as Spain, do not have national policies for these units in rural areas3.
Communication between primary health care and specialized care is weak in fragmented health systems. Support and logistical systems are not coordinated, aggravating the issues of coherence, quality, security, and access in all care levels7. In the Americas, PAHO/WHO proposes the arrangement of Integrated Health Services Networks (RISSs) based on four domains: care model, governance, organization and management, and allocation of financial resources and incentive system7. In Brazil, since 1988, the right to health has been guaranteed by the national constitution. Access to health services must be ensured through the Unified Health System (SUS), guided by the principles of universality, decentralization, comprehensive care, and social participation. The financing, organization and provision of health services by SUS is the responsibility of the three spheres of government: federal, state, and municipal8. Political–administrative decentralization in SUS determines the municipality as the sphere responsible for the provision and organization of primary health care in the territories. For specialized care provision, especially in small municipalities, cooperative arrangements between governments that guarantee full access to health are necessary9. The ‘health regions’, defined by national health governance, correspond to the health organization strategy for the provision of services among a set of municipalities. In the health region, the municipality with the greatest diversity of services becomes the headquarters and health reference for others. Health regions are inspired by the classic model of the Dawson report10 and, therefore, are organized through a hierarchy among services. Furthermore, the regions are planned according to the logic of healthcare networks and organized based on scale, quality and opportunity for access criteria. The provision of services and assistance flows are defined through agreements and pacts between managers of municipalities in the regional health territory. However, the understanding and provision of comprehensive care are compromised, among other factors, by the lack of guidelines guiding the structuring of a model for the provision of specialized care in healthcare networks (RASs)9.
According to Dawsonian logic, a minimum scope of actions to promote comprehensive care would be assured in the health regions, and primary health care provided in each municipality. More complex procedures would refer to health macro-regions (which gather several regions) or even the state capital, depending on the regionalization’s design. However, specialized care provision is concentrated in few health regions in the country, generally with greater economic dynamism9, and does not cover all primary healthcare requests11. Other issues are the insufficient and heterogeneous provision of specialized services, one of the significant challenges of the SUS11.
This mosaic of problems seems to share a common genesis and, among other aspects, derives from of the lack of definition of a model for the provision of specialized care consistent with the production of care in the RISS or RAS, as it was conventionally called in Brazil. This article aims to identify and analyze arrangements for the provision of specialized care in Brazilian remote rural municipalities (RRMs). It is argued that such strategies should be organized per the territories’ specificities and that, in the absence of models, informal and dispersed arrangements adopted by managers, users, and professionals tend to dissipate the scarce health resources, exacerbating inequalities and care fragmentation.
Methods
A multiple-case qualitative study on RRMs was performed through semi-structured interviews, complemented by analyzing secondary data from national health information systems. In the country, the definition of rural and urban municipalities gained a new typology in 201712, in line with OECD and European Union methodologies. This article is nested in a national study on the organization and use of primary healthcare services in Brazilian RRMs13.
The results of seven RRMs located in the Brazilian semi-arid region were analyzed. It is an area marked by water scarcity and low socioeconomic development and is a space of contradictions, with high social inequality14. The semi-arid region is a vast area concentrated in the Northeast region of the country and includes municipalities in the north of Minas Gerais, in the Southeast region15. Among the 323 municipalities classified as remote rural in the country, 64 are in the semi-arid (22 in the north of Minas Gerais, 20 in the state of Bahia, and 22 in the state of Piauí).
The RRMs in the semi-arid region were first characterized according to socioeconomic, demographic, and health indicators to define the intentional sample of municipalities in the study. Subsequently, the criterion for selecting municipalities that would approach the ‘type municipality’ was adopted considering these variables, which led to the selection of Morpará and Ipupiara (Bahia), Rubelita and Indaiabira (Minas Gerais), and Rio Grande do Piauí (Piauí). Given the RRMs diversity, it was decided to include municipalities with outlier characteristics in the area (Pilão Arcado, due to its above-average population, and Bonito de Minas, due to the lowest GDP per capita).
The territory’s classification was adopted in two areas to understand the intramunicipal characteristics: the headquarters, identified as the core; and the rural area, an inland area of the municipality, which corresponds to small and dispersed population groups located in regions far from the headquarters.
Participants and data collection
The study population consisted of 22 respondents: municipal health managers (municipal health secretaries (GM1) and primary healthcare coordinators (GM2) (14) of the seven cases), regional managers (GR) of each of the five health regions to which the seven municipalities belonged (5), and the state primary healthcare coordinator (GE) in each of the states involved (3). These key actors were primarily responsible for the management and organization of the RAS in the SUS, which, according to the Brazilian federative system, establishes the public and universal provision of health services under the responsibility of the three government spheres: federal, state, and municipal.
Interviews were conducted in person, in the respective workplaces, from May to October 2019, lasting from 1 to 2.5 hours, audio-recorded, and fully transcribed. Secondary data from national health information systems were adopted to characterize socioeconomic indicators, the health service network, and specialized care procedures for the seven cases. Procedures performed at the secondary care level were selected to analyze access to specialized tests: echocardiography, colposcopy, and obstetric ultrasound with and without Doppler. Such procedures were selected because they are part of the lines of care for, respectively, systemic arterial hypertension, cervical cancer and prenatal care used as tracer events in the national study, of which this article is part13. These data were accessed in the SUS outpatient information system and correspond to the tests carried out for the seven municipalities’ citizens from October 2015 to October 2020. A source–destination matrix was drawn up; that is, where each of these procedures was performed for the population residing in the selected RRM.
Data analysis
Thematic content analysis was carried out to produce the results, guided by the attributes of the RISS related to the provision of specialized care7: sufficiency of the health services network to provide comprehensive care, provision of specialized services in more appropriate places, integrated management of logistical support, available assistance coordination, integrated information system linking the network’s points, sufficient workforce, sufficient funding in line with the RISS targets, and a single governance system for the entire network. The results were presented considering the context of health services and the arrangements identified for the provision of specialized care, within which the RISS attributes are addressed. The authors aimed to ensure the findings’ quality and validity by triangulating the information from the interviews and secondary data. It was not intended to judge each municipality but to understand processes in RRM territories through representative settings.
Ethics approval
This study was approved by the Human Research Ethics Committee of the Sérgio Arouca National School of Public Health of the Oswaldo Cruz Foundation (no. 2.832.559).
Results
Context: health services in remote rural municipalities
The seven municipalities were distributed over three Brazilian states and comprised five health regions that should provide specialized care actions, mainly in the respective host cities. The characterization presented in Table 1 expresses the context of greater socioeconomic vulnerability of the RRMs and their respective health regions when compared to the states and Brazil.
The public provision of primary healthcare services stood out, with high coverage by the Family Health Strategy, the main Brazilian primary healthcare organizational model, with teams consisting of a general practitioner, a nurse, nursing technicians, community health workers, and the oral health team; residual coverage by private health insurance (<2%); and lack of private and public specialist services, which, according to state managers, historically conditioned intermunicipal travels frequently to the state capital and headquarters of the health macroregion to seek specialized care. Interdisciplinary teams (family health support centers) also supported primary healthcare professionals in developing educational and clinical actions (Table 2).
The travel modes to the specialized care varied, and evaluations were unanimous regarding the difficulties in the provision of transport means. People used municipal health transport considered to be insufficient, public transport financed by municipalities or their own resources (in general, city buses scarce and at times incompatible with scheduling visits/specialized tests), or rented vehicles with their resources. Sometimes, travel was a more significant challenge than the provision of specialized care itself, with more unfavorable differences for people living in the rural areas of the RRM, who endured greater distances and out-of-pocket expenses, as they needed to reach the headquarters to subsequently access a means of transport to reach specialized care providers (Table 3).
Distances and the dangerous nature of some routes became more severe the more distant the specialized care provision place, as in the cases of concentration in state capitals. Death could be an outcome depending on the severity of the case.
Also, providing health transport or intercity bus tickets was not enough. It was necessary to ensure some type of support for their stay (‘support homes’) when, for example, users were referred to the capital or the headquarters of the health macroregions, especially those from the inland region or who required prolonged treatment. Such costs placed a heavy burden on local budgets, which sometimes interrupted the regular provision of health transport to ‘balance’ public accounts.
Table 3 shows the distances traveled by residents of the headquarters and rural areas to the leading specialized care providers. The table also indicates the estimated travel times by managers, professionals and users participating in the study whose evaluations consider, in addition to distance in kilometers, road conditions, means of transportation and weather conditions.
Taking as a reference four specialized procedures performed by the SUS (which excludes procedures paid for by the users themselves or via private health insurance plans), the authors identified the municipality that concentrated most of the tests performed in 5 years (October 2015 to October 2020) and the respective distances from the seat of each RRM (Table 4).
Epidemiological parameters were not employed to estimate the sufficiency of the tests shown in Table 4. Also noteworthy is a budget ceiling from federal resources for specialized outpatient care, and procedures paid for by municipalities were often not reported in national information systems. Even so, the insufficiency of some procedures was observed, considering that it is the sum of the procedures performed in the SUS over 5 years. A low number of colposcopies was observed in all municipalities (except Morpará). In three cases, most examinations were carried out in the state capital, with distances reaching almost 800 km. The echocardiogram performance pattern was even more restricted. The shortest distance was 217 km and the longest 788 km, and in none of the cases was the main place of performance the health region headquarters. Obstetric ultrasound showed essential differences between approved and presented, indicating municipal contributions in test costs and performance in the city itself or the health region headquarters, which is reflected in lower distances covered for the service. The Doppler ultrasound, indicated in high-risk pregnancies, was not carried out or performed with municipal resources and not registered in the information system (Table 4).
Table 1: Characteristics of remote rural municipalities and health regions, semi-arid region, Brazil, 2020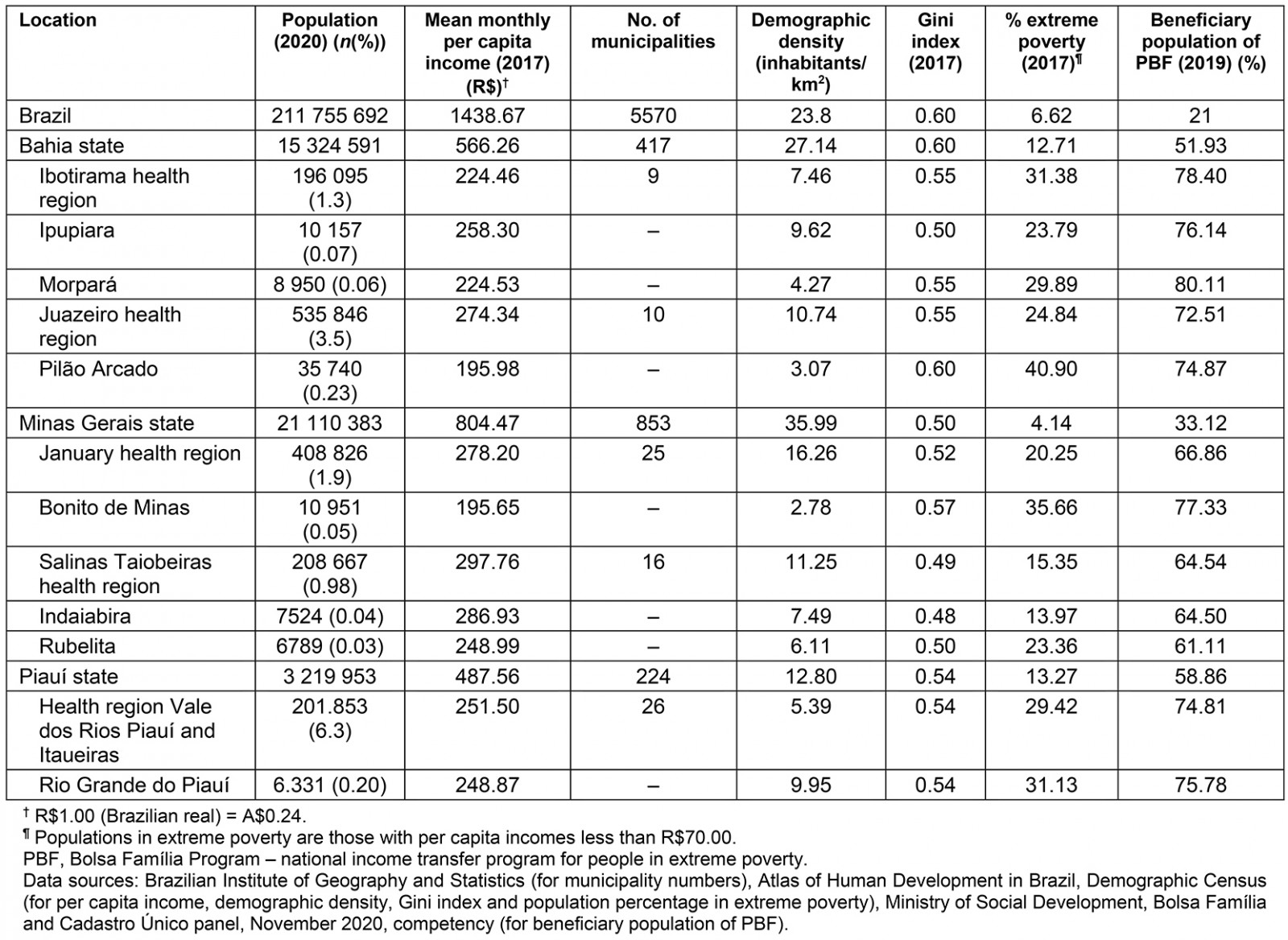
Table 2: Health resources and equipment in remote rural municipalities, semi-arid region, Brazil, 2019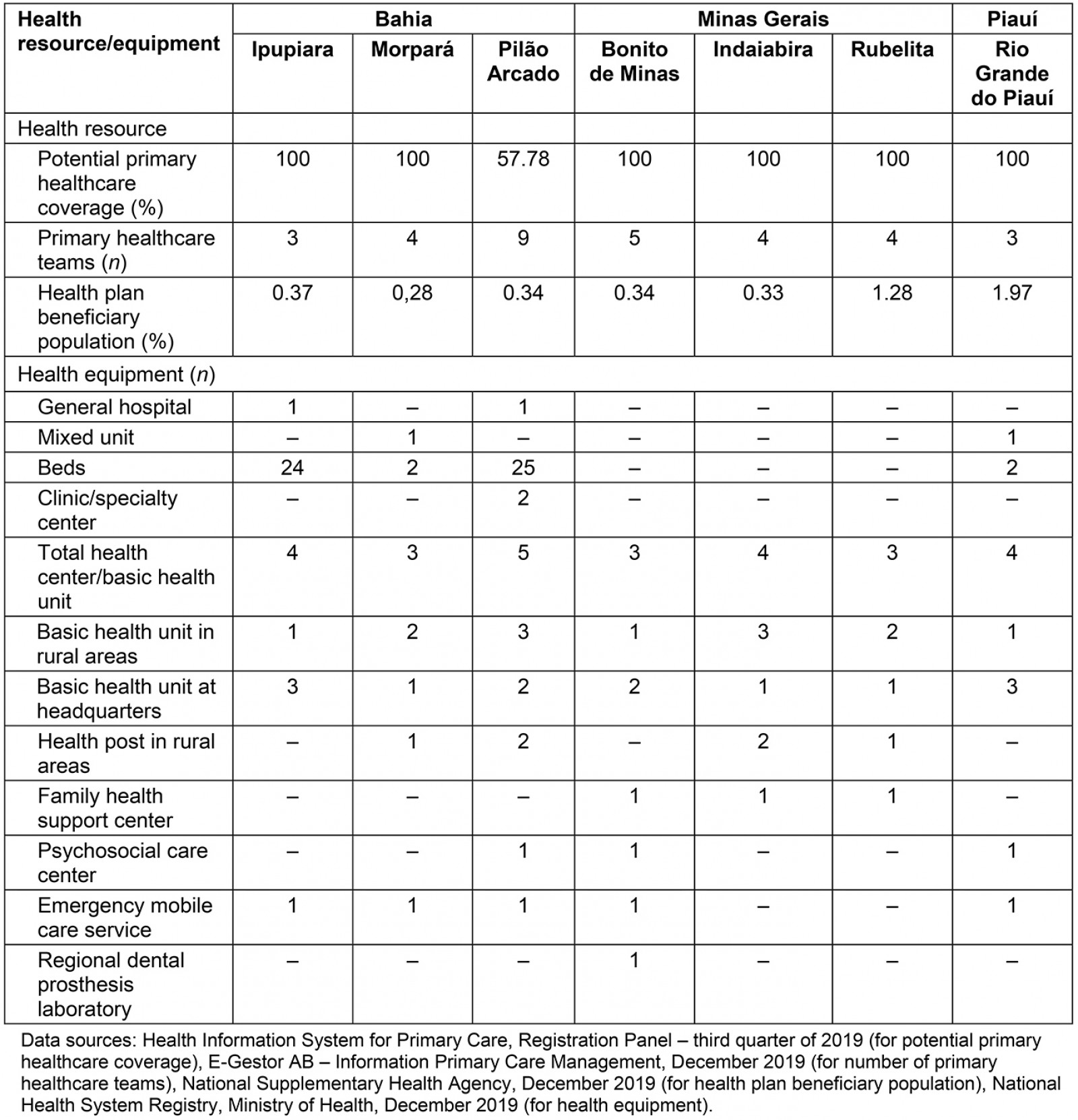
Table 3: Distance and time between remote rural municipalities, and between headquarters of health regions and macroregions and the state capital, semi-arid region, Brazil, 2020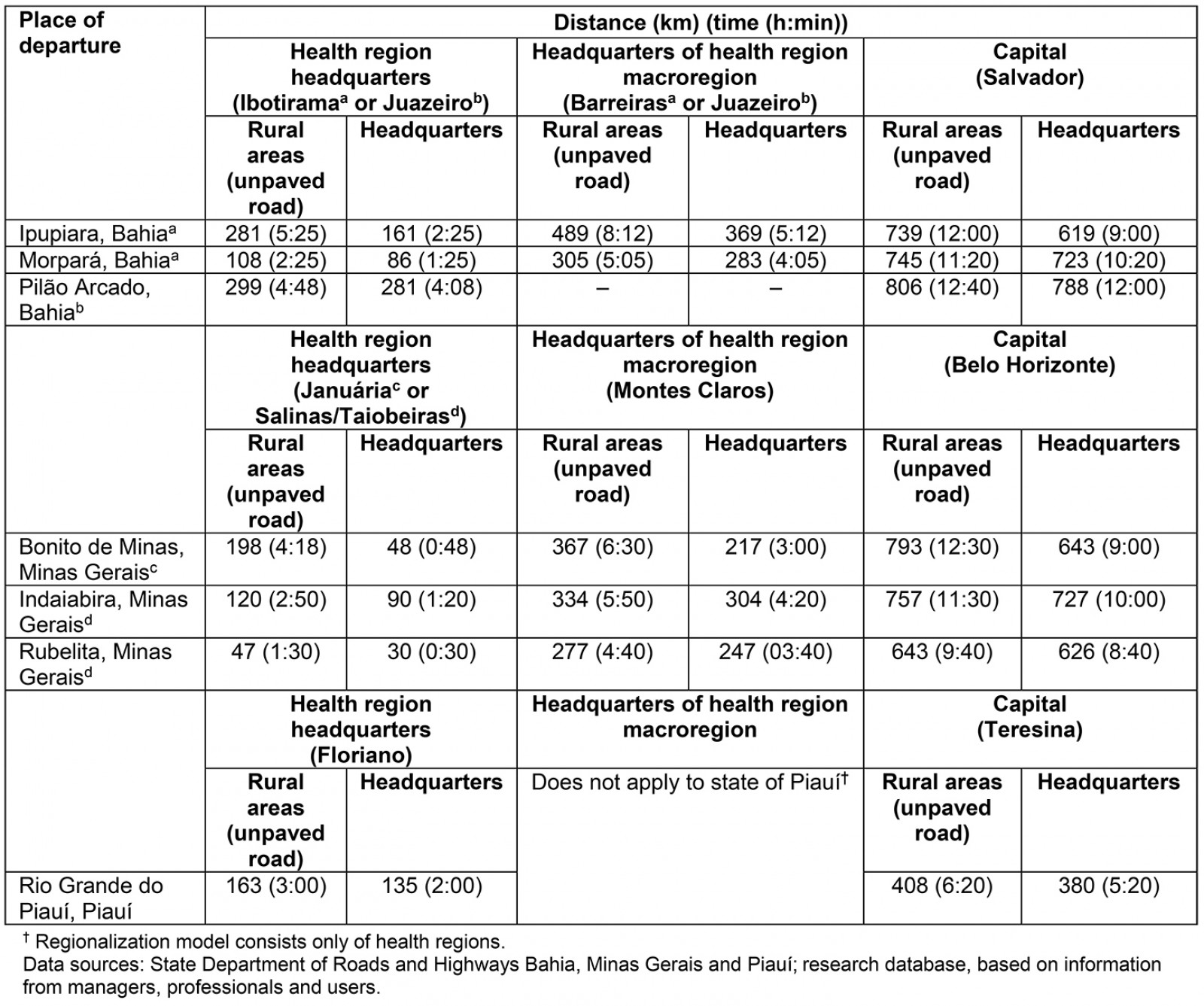
Table 4: Specialized tests by main place of performance, October 2015 to October 2020, remote rural municipalities, semi-arid region, Brazil, 2020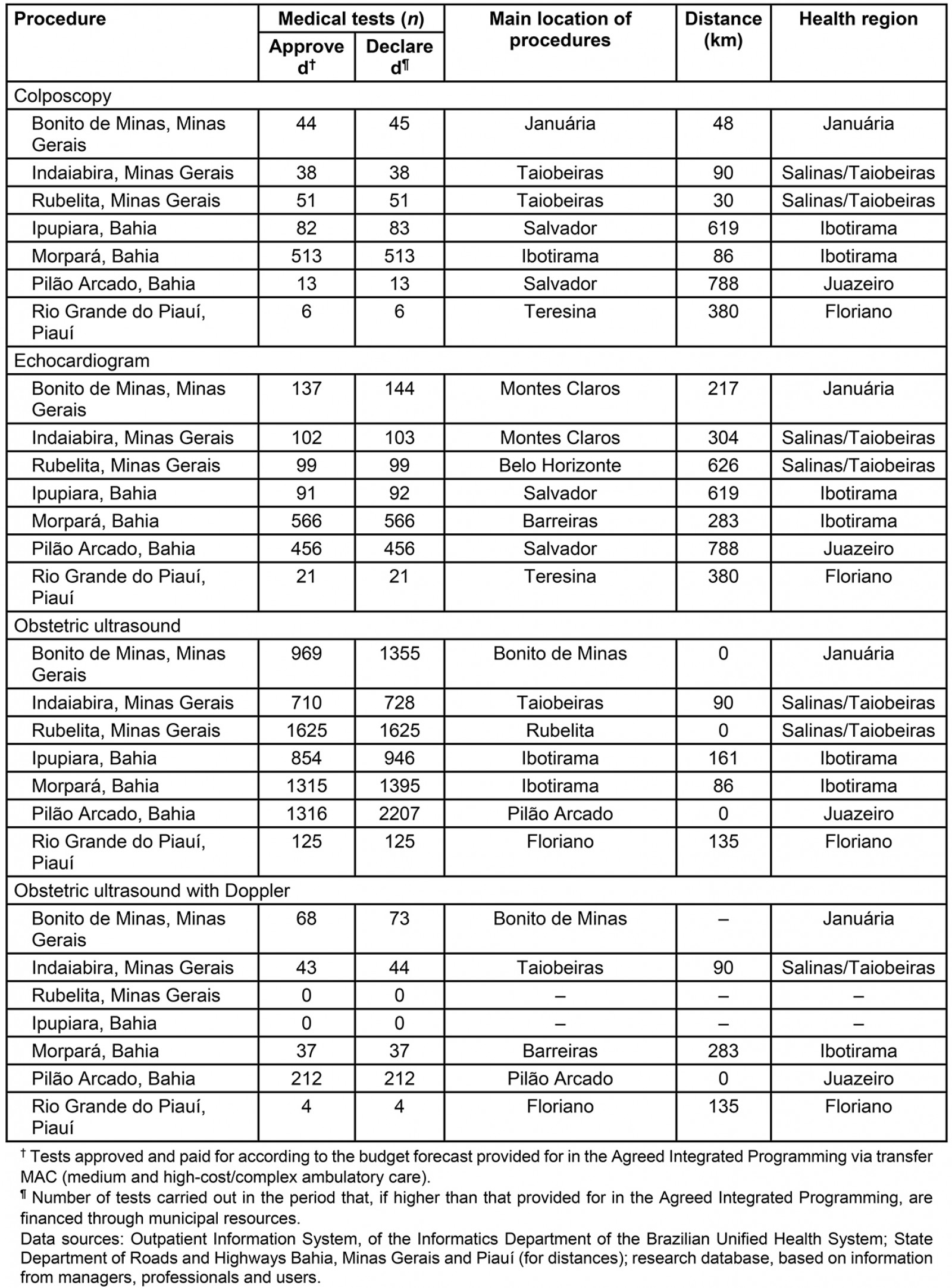
Arrangements for the provision of specialized care
Various arrangements were identified for the provision and financing of specialized care in the RRM, with different degrees of implementation, namely public provision through Agreed Integrated Programming (PPI) in the health region, health consortia, public provision in the municipality itself or neighboring municipalities, care in private health services through direct purchase (out-of-pocket expenses), and telehealth.
Public provision of specialized care through Agreed Integrated Programming in the health region: The main instrument for allocating financial resources for the provision of specialized care in the RRMs was the PPI, which was a negotiation instrument between managers in a health region to decide which municipalities/public and private service providers SUS financial resources would be allocated to ensure specialized procedures. According to the regionalization design, specialized care services should concentrate primarily on the respective health regions to guarantee more timely access and the services of greater technological complexity in the health macro-regions, which did not occur in many cases.
Taking as a reference some procedures presented in Table 4, it was observed that the public provision of specialized tests routinely requested to monitor cervical cancer, arterial hypertension, and prenatal care did not have as the main reference the city headquarters of the health region, in which, in general, the provision of health services negotiated via PPI should be concentrated. For some tests/specialists, despite distances of almost 800 km (rural area of Pilão Arcado), most referrals were made to the state capital. Sometimes, resources from special funds (parliamentary amendments) were invested in ambulances for user travel.
The long distances between the municipalities that provide specialized care and the RRMs (Table 3), and the irregular provision of transport implied lack of assistance and, currently, inequalities according to the managers’ assessments. Sometimes, it became more ‘advantageous’ for the user to pay out-of-pocket, especially for low-cost services performed in the municipality of residence or neighboring municipalities.
Distance to the municipalities with most of the specialized care provision evidenced more significant difficulties of access for the rural inhabitants. They sometimes had to travel routes exceeding 100 km (Ipupiara, Bonito de Minas, and Pilão Arcado) to the RRM headquarters and, subsequently, traveled to specialized reference services (Table 3). Also, as assessed by the informants, the provision of dispersed specialized care among various municipalities in the health regions overly encumbered health transport logistics.
The costs of tests and specialized visits in the country were set by the Ministry of Health and were outdated in relation to the medical market, considering the scarcity and low diversity of providers in the regions studied. Consequently, managers negotiated the purchase of services through agreements with private providers. The provider was contracted for the value of resources and supplied some procedures (above the fixed price).
In the cases studied, specialized care scheduling was performed, in general, by the user with a medical referral, in the municipal health secretariats. As there was no computerized system for scheduling appointments and specialized tests in the primary healthcare units, users living in the rural areas of the RRM needed to travel to the municipal headquarters, meaning more significant expenses, in particular for the most impoverished population.
Public provision of specialized care via Health Consortia: Two types of health consortia were identified. The municipalities of Minas Gerais had intermunicipal health consortia (CIS), established to provide specialized care that complemented the insufficient provision via PPI. The CISs had regional coverage and were financed through public resources raised by the municipalities. A ‘menu’ of services was provided by CIS in private providers and used according to the schedule made by the municipalities. As a result of the purchase of procedures linked to the Ministry of Health’s values, many private providers were not interested in providing their services, thus limiting diversity.
In general, specialized care provision via CIS was reserved for urgent situations and more significant access difficulties. The regional manager affirmed that the CIS strategy was essential to the municipalities as it ensured part of the specialized care not supplied via PPI and guaranteed some scale in the purchase of services at better prices.
In Bahia, regional health polyclinics have been implemented through interfederative health consortia since 2017, with voluntary adherence to the municipalities, to provide specialized care services in the health regions. Contrary to the CIS model in Minas Gerais, the polyclinics had state equipment, direct specialized care providers, with management and financing shared between municipalities and the state. The objective was to guarantee specialized care provision through care flows coordinated by the primary health care and health transport by minibus, a critical resource for the RRM. According to the state manager of Bahia, the concern with the integration between primary health care and specialized care was mentioned only in the initiative to implement regional polyclinics. In the other evaluations, care coordination was assumed non-existent as there were no shared electronic medical records. Some transit of clinical information was incumbent upon the user themselves or, as in small municipalities, primary healthcare managers and professionals seeking information about care provided in other services. Community health workers were identified as the primary informant of a user’s situation, allowing some care continuity.
In Ipupiara, the municipal manager considered that there was no interest on the part of all municipalities, as the municipal financial contribution for maintaining the polyclinics was high. Political alignment between municipal and state governments, too, was identified as a determining factor for adherence to CIS.
Public provision of specialized care in the municipality itself or neighboring municipalities: While timely and discontinuously, depending on the availability of municipal financial resources, to some extent RRM provided specialized care at their headquarters through direct purchase of private services (clinics or professionals). Such an organizational option aimed to cover the insufficient provision of services via PPI, especially those with greater demand and lower cost, such as obstetric ultrasound. Also, a popular and political appeal was noted for the provision of specialized care in the territory itself, mainly due to the difficulty of traveling to other municipalities. A municipal manager said there was an understanding that it would not be necessary to provide specialized care in RRM, but the managers were pressured and sometimes met the political interests and concerns of the population.
In Indaiabira, the municipality adhered to the CIS and entered into agreements with private clinics in the municipality of the health region, with its resources, because it was impossible to meet the specialized care demands even with CIS and PPI.
In Ipupiara, the municipal manager hired a psychiatrist and an orthopedist. In addition, the manager provided ultrasound and X-ray tests in the municipality, paid for with municipal resources. Morpará provided psychiatric care to users referred by primary healthcare teams. The same professional was also a cardiologist and sometimes met the demand for surgical risk. More recently, an ultrasound device had been purchased, although the problem of a professional for the tests remained.
Ultrasound was also available in Pilão Arcado, according to the respondents’ report and secondary data (Table 4). A contracted doctor performed the tests every 2 weeks. Rio Grande do Piauí municipal managers said ultrasound tests were provided biweekly, with weekly appointments with a cardiologist (not shown in Table 4, which shows a low number of obstetric and Doppler ultrasounds in the municipality itself).
Care in private health services through direct purchase (out-of-pocket): Users resorted to out-of-pocket payment to speed up the care itinerary due to the scarce specialized care provision, prolonged time, or even distance to access some appointments and procedures via the public system.
Primary healthcare professionals recommending users to seek, when possible, private health services to carry out visits and specialized tests through direct disbursement to shorten waiting times were commonly reported. In some cases, the community itself and health professionals were mobilized to obtain resources to finance the procedures.
In some cases, municipal management encouraged seeking private services, intermediating discounts, indicating well-known professionals, paying for transportation, or some other subsidy in a nearby municipality. In Ipupiara, transport lines were created to meet the demand for private health services in neighboring cities.
Many users reportedly did not even seek the SUS, turning directly to private providers because they already knew the hardships or impossibilities of public road access.
Telehealth: Minas Gerais municipalities had telehealth services in cardiology, and teleconsulting was hardly used. Electrocardiograms seemed to be the most frequent test. Bahia state management reported that electrocardiogram telediagnosis and, more recently, teledermatology were implemented in the state, including purchasing equipment for the poorest municipalities. Rio Grande do Piauí (and municipalities in the health region) did not use telehealth, or the use was limited to professional training and training activities.
The respondents did not indicate routine telehealth use by health professionals for several reasons: insufficient internet and computers, mainly in primary healthcare services in rural areas, low adherence by professionals, lack of technical support from regional and state administrations, delay in responding to teleconsulting, and technical difficulties of municipal management to implement and use some telehealth instruments. While federal policies for the computerization of primary healthcare services have been reported, they have been insufficient to achieve universalization of this process. There was no quality internet access, and, in most cases, the provision was the responsibility of each RRM.
Table 5 presents a synthesis of the results according to the RISS attributes6 and definitive statements by the key informants who give density to the study’s findings.
Table 5: Summary of results and expressive statements, according to attributes of the Integrated Health Services Networks – remote rural municipalities, semi-arid region, Brazil, 2019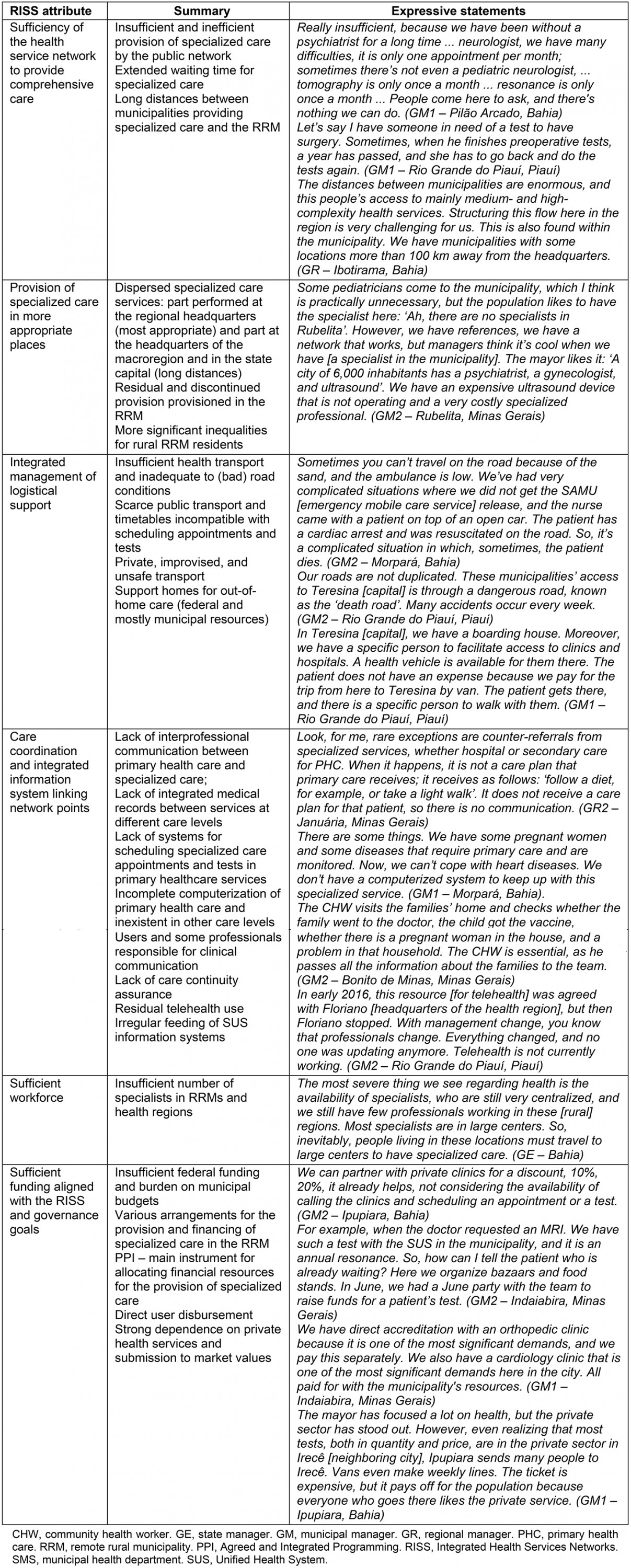
Discussion
The results indicate that the analyzed cases were not close to the RISS parameters and attributes, a situation currently found also in other Latin American countries, whose health systems are characterized by fragmentation and weak network performance7. Various modalities for the provision and financing of specialized care in the RRM were identified, with public and out-of-pocket resources unable to respond quantitatively and qualitatively to the demand for specialized care integrated with networks.
The cases presented are made up of municipalities and health regions vulnerable in several aspects, without the economic dynamism that acts as a determinant for the attraction of specialized professionals16 and without national policies for regulating the health workforce, especially concerning medical specialties17. On the other hand, the assessment was unanimous on the insufficiency of federal and state resources compatible with the conformation of RISS, which overloads the meager municipal budgets and conditions an inefficient, uncoordinated, and discontinuous specialized care provision pattern undertaken locally.
In the context of this study, timely provision of specialized care in an adequate place was not achieved, resulting in a fragmented, low-resolution model. The fragility of the regionalized health networks, aggravated by SUS underfunding, confers care gaps and unacceptable commuting to undergo basic procedures (such as colposcopy and echocardiogram). Prolonged efforts and long times to achieve health care in general – more severe in rural contexts – can also lead to the direct search for private care with out-of-pocket payment, as found in this study, or even more accessible care alternatives such as pharmacies18.
Such evidence takes on more dramatic contours in the context of rurality, due to the socioeconomic vulnerability of the population and municipalities, insufficient resources and health equipment in the regions and great distances to be covered. Factors such as isolation, road quality, and climatic conditions have a bearing on the decision to move to obtain health care4. All the mapped difficulties do not favor access and can cause discontinuity, delayed and unrealized care, and therapeutic opportunity loss19,20.
The experience of regional polyclinics in Bahia, via CIS, with cofinancing and leadership from the state management, seems to be an arrangement more suited to the provision of specialized care from a regional perspective. Furthermore, it improves care coordination by primary health care and increases access to specialized care by offering health transport for the population to travel to the service11. A challenge would be widespread support and political gains from specialized care provision in the city itself or initiatives by the local manager, despite the dissonance regarding health needs, as often seen in other contexts3.
In Latin American countries, there are incipient studies on the relationship between transport and health, and policies aimed at mobility, which, when they exist, are mainly focused on urban environments21. Health transport is an essential component of logistical support to access specialized care and did not obey clinical and organizational rationality – now provided by the municipal management without assured continuity and sufficiency, now at the expense of the users themselves and with spending incompatible with household income, in an unsafe and improvised fashion. The context of insufficient or absent health transport is also that of low investment in infrastructure (unpaved roads and insufficient public transport) and the lack of other public policies. In this sense, while geographic location plays an essential role in determining access to health services, it should not necessarily translate into inequities, insofar as policies and actions for improving rural health are more effective if they address the set of vulnerabilities affecting these populations18.
The authors could not identify integrated information systems linking the RISS points, such as shared electronic medical records. The precarious computerization of the primary healthcare services and systems for scheduling the specialized care caused yet more travel for users, which, for rural residents, represented a barrier preceding visits or tests. In a fragmented network, the impossibility of communication, coherence, and low cooperation between primary health care and specialized care22 can result in scheduling unnecessary specialized procedures that cause dissatisfaction to users when they have to postpone their routine activities to attend health services23, especially among older adults leaving their comfort area1, and dissipate the already insufficient health resources.
The incomplete primary healthcare computerization draws other problems, which lead to the underutilization of telehealth, a strategic resource in remote areas. In Australia, telehealth also lends itself to specialized visits accessed by the user and is reimbursed by public insurance for amounts higher than the face-to-face visit3.
The development of telemedicine strategies in remote areas can improve access to specialized care and avoid preventable hospitalizations, an investment target in many countries3,4. Also, the availability of telephone contact with health services for rural residents, an easily accessible measure, could improve obtaining clinical guidelines and general information for access to care18, which was not observed in this study.
Despite the previous municipal efforts to resource specialized care, the failure to feed into national systems hinders monitoring of the sufficiency and adequacy of procedures according to epidemiological parameters and sizing the financial and human resources necessary for planning RISS7.
It is noteworthy that the RRMs tend to present a more fragile and vulnerable governance system to political party harassments to the detriment of technical–sanitary issues in constructing the RISS24. This feature compromises care flows and transfers the responsibility for constructing alternative therapeutic itineraries to users, often with iatrogenic results.
Finally, the greater the dispersion associated with lower population density and longer commuting times to access health care, the greater the need for integrated, comprehensive care in primary health care. The concentration of specialists in urban centers results in dependence of rural populations on primary healthcare providers who, sometimes, develop an expanded scope of practices without adequate training and infrastructure6, a priority field for interventions. The resolution of primary health care can also be increased through the incorporation of areas such as mental health25, access to pharmaceutical care at home26, e-health interventions27, combination and integration of telemedicine and home visits carried out by health professionals health28, drive in–drive out and fly in–fly out models29, among others. No less important is recognizing that the insufficient and discontinuous provision of health professionals in remote rural municipalities, especially doctors, threatens the sustainability and maintenance of health care. This is a global problem for rural areas in which policies to reduce scarcity involve measures at the individual and contextual level, such as the establishment of medical schools in rural areas that contribute to the improvement of the infrastructure of rural health services, and enable the involvement of local communities and promotion of daily experiences of doctors and students with the reality of rural medicine30.
Limitations
This study considered the experience of managers at various levels of the health system of the Brazilian semi-arid territory, whose perceptions and evaluations were synergistic as to the challenges for the provision of specialized care in RRMs, caused by local and regional characteristics, which can be different from other rural scenarios, such as in the Amazon region31. The experiences of other key actors, such as users, were not considered, although secondary data such as the local production of specialized exams can confirm the barriers to access to specialized care.
Conclusion
In rural Brazil, the disorganization or lack of a systemic response based on regionalized networks generates several care improvisations. The less structured the RISS, the more informal the arrangements that emerge, with gains for the private sector to the detriment of SUS users.
The cases studied bring about essential contextual elements for planning the provision of systemic and regional specialized care at the risk of defining innocuous proposals for the reality of RRMs in the Brazilian semi-arid region. Considering the various challenges that condition the concentration of services and health professionals in urban centers, some possible arrangements are indicated to streamline specialized care provision in these contexts.
The first concerns the mobility capacity of RRM users. Public and safe integrated health transport systems are a crucial element for access to health, as is the definition of care flows that correspond to real and feasible routes within the municipalities (headquarters and rural area) and in the health region.
Another action refers to the increase in the resolving capacity and linking users to primary health care, including urgent care and investments in information and communication technologies that enable the clinical coordination and streamlining of the provision of specialized resources via telehealth to professionals and users.
Strengthening social participation levels and collegiate regional management bodies are strategies to mitigate intervening factors, such as political and private interests, which hinder organized and reasonable provision of specialized care. Regional governance must combine policy and technique to retract mechanisms based on users’ accountability to seek the necessary resources for health care, which are not representative of SUS universalizing precepts.
While such organizational strategies are fundamental in different contexts, it is argued that they are crucial to enable access to specialized care in RRMs since these populations have no other care options and are exposed to more significant inequalities. Social policies must provide for specific actions for the RRM, notably for their rural areas, without which health actions will be less effective. To this end, they must be accompanied by sufficient federal funding for the establishment of RISS and the strengthening of collaborative regionalization between municipalities, from a Dawsonian perspective that, while not representing anything new, has barely advanced in the country and seems to be outside the current agenda of political priorities.
Acknowledgements
The research project Primary Health Care in Remote Rural Territories in Brazil, of which this article is a part, was financed by the Ministry of Health of Brazil. This article is part of the postdoctorate done by the first author at the University of São Paulo Public Health Faculty, supported by a grant from the National Council for Scientific and Technological Development (CNPq) Senior Post Doctoral Program (Process 104130/2020-2). We thank the CNPq for its support to PF Almeida and A Bousquat through the Productivity in Research Scholarship.