Introduction
Translating research knowledge into practice and policy is a high priority for researchers, health professionals, health managers and policymakers to ensure that research has real-world impacts by effecting improvements in health practice, quality of care, and health consumer outcomes1-4. Aligning local health policy, models of care, and health practice with contemporary research evidence is even more critical for rural and regional health services within the communities that experience comparatively poor health outcomes5,6. Health-professional-led research tends to address real-world practice issues and, therefore, the findings tend to be more readily translated into practice7-11. However, successful and sustained translation of health-professional-led research into practice is not guaranteed, and capacity-building strategies are needed to support health professionals to engage in practice-based research and translation12-14.
Despite the expanding field of implementation science, which promotes the development and use of evidence-based frameworks and strategies to guide research translation15, many health services fail to effectively translate evidence-based policies, programs and practices16. Fundamental to achieving the translation of evidence into the health service context is the research translation capacity of the people who work in those settings14,17,18. Within the healthcare context, health professionals, program managers, administrators and others who identify local practice or policy issues, or misalignment between existing research knowledge and current practice, have an opportunity to engage in research translation. For the current study, emerging health professional researchers (emerging researchers hereafter) are people working in health settings who have little or no formal training or experience undertaking research.
Research capacity building encompasses the development of both organisational and individual capabilities12-14. There has been considerable work aimed at building research capacity both at organisational and individual levels in health services12-14,19. Factors influencing research capacity and outcomes are well-documented, such as the identification of organisational priorities20,21, protected time for research activity21, the implementation of embedded researchers4, partnerships between academic institutions and health services15, knowledge brokers20,22 and mentoring23.
Although improving research translation is an implied aim of building research capacity, comparatively few training programs have focused on building health professionals’ research translation skills24. Programs that have focused on research translation skills and capability tend to vary in terms of their target audiences, objectives, curriculum, outcomes, and evaluation methods12,24,25. Few programs provide guidance for health professionals on how to operationalise implementation strategies to translate evidence into practice, with even fewer examples from rural or regional areas, where research activity and infrastructure are generally less mature than that seen in metropolitan areas5,6,26. Enduring workforce shortages create additional challenges to conducting and translating research into practice in rural settings and to sustaining research translation capacity and capability-building efforts27,28. The key learning and support needs for emerging researchers, to enable successful engagement in translation-focused research and implementation in rural settings, are not established.
Implementation frameworks such as the Consolidated Framework for Implementation Research are important for understanding key factors that influence the implementation of an intervention29,30. The features of an intervention, which in the current case is a rural research translation capability-building program, can have major influences on implementation; for example, stakeholders’ perceptions of the relative advantage of implementing a research translation capability-building program. In a bid to optimise the development, implementation and evaluation of a rural research translation capability-building program, the research team identified the need to work with relevant stakeholders at multiple organisational levels to co-create the program and incorporate features that were important to them31. Through previous scoping and research to inform and implement a multimodal research capacity and capability-building program for rural health professionals24,32, the authors identified the need to involve first-level managers in the capability-building initiatives. This exploratory work begins to integrate manager, mentor and emerging researcher perspectives on the capability building and support needs of emerging researchers into the research capacity-building program.
Informed by a knowledge gap identified by an academic health science centre concerned with building research translation capability, the current research seeks to answer the question: what are rural health researchers’ perspectives on capability-building needs for emerging researchers to enable the translation of research into health practice? For this study, the following working definition of research translation as described by the field of implementation science, is adopted: the work undertaken to adapt and implement research knowledge into health practice and health policy both locally and more broadly14,33,34. The findings of this exploratory study were intended to inform the development of a multimodal research translation capacity and capability-building program and the basis of future investigations into research- translation capability-building programs for health professionals.
Methods
Study design
This qualitative descriptive study drew on a social constructionist paradigm, which recognises that people experience and make sense of the world in different ways, through their social interactions35. Qualitative description is a flexible qualitative research methodology that facilitates the exploration of the experiences and perspectives of people who have particular knowledge or experience of a phenomenon36. The research team comprised members with varying levels of research capability building, education, and health services research and translation experience. The research team brought these perspectives to the data collection and analysis process.
Participants and setting
This study was conducted in the Barwon South West and Grampians regions in Victoria, Australia. Participants were recruited from three key groups: emerging researchers, health managers or team leaders with an expressed interest in research (managers), and experienced academic or health services researchers (mentors). Participants were recruited from health services, universities and a local primary health network, all situated in rural or regional areas37,38. Potential participants were identified by research team members, through their networks and invited by email to participate. A participant information and consent form was provided and those interested in participating were asked to read, sign and return the consent form prior to participation.
Data collection and analysis
Data were collected through three focus groups, each comprising a mix of emerging researchers, managers and mentors, none of whom worked directly together to avoid any perceived or actual power imbalances. Focus groups were conducted by videoconference and lasted approximately 1 hour. A researcher with extensive interview and focus group experience and no managerial or collegial relationship with participants (AB) conducted the focus groups. An interview guide consisting of eight discussion points was used flexibly to ensure the discussion was rich and free flowing yet focused enough to address the research questions. Interview questions prompted participants to reflect on and describe their understanding of research translation, and their perceptions of the capability-building and support needs of emerging researchers to engage in translation-focused research. The focus groups were audio-recorded and transcribed. Participants completed a participant demographic questionnaire prior to the focus group.
Data were analysed using a five-stage framework approach39. Three researchers (AS, AWS and OK) familiarised themselves with the data and conducted initial manual inductive coding. These initial analyses were used in the development of the initial coding framework, which was agreed upon by the three researchers. The coding framework was used by one researcher (AS) to code the data using NVivo v12 (Lumivero; https://lumivero.com/products/nvivo) and the coding was cross-checked for consistency by another author (OK). The three researchers reviewed the coded data to identify patterns and generate themes, which were then interpreted in light of the existing research capacity and capability-building literature.
Ethics approval
Ethics approval was obtained from the Barwon Health Human Research Ethics Committee (20/183).
Results
The participant sample (n=19) comprised emerging researchers (n=12), managers (n=4), and mentors (n=3). Participants represented four health services, one university and one primary health network. Most participants (n=14, 74%) were female and their ages ranged from 29 to 67 years. The time spent working in their profession ranged from 2 to 45 years. See Table 1 for more detailed demographic data.
Participants understood research translation to be a binary concept comprising research that is grounded in health practice and the activities required to adapt and implement research evidence in the local context. Their understandings of the concept provided context for the description of the four key themes related to research translation support needs for rural health researchers. The themes identified were: understanding the study and translation context is vital to enacting change; engaging with stakeholders identifies research and translation priorities and suitable approaches; mentor and managerial support assists navigation of research translation activities; and access to clinical and research networks promotes research translation partnerships and collaborations. These themes are presented below with illustrative quotes.
Table 1: Demographic data for online focus groups (n=18)†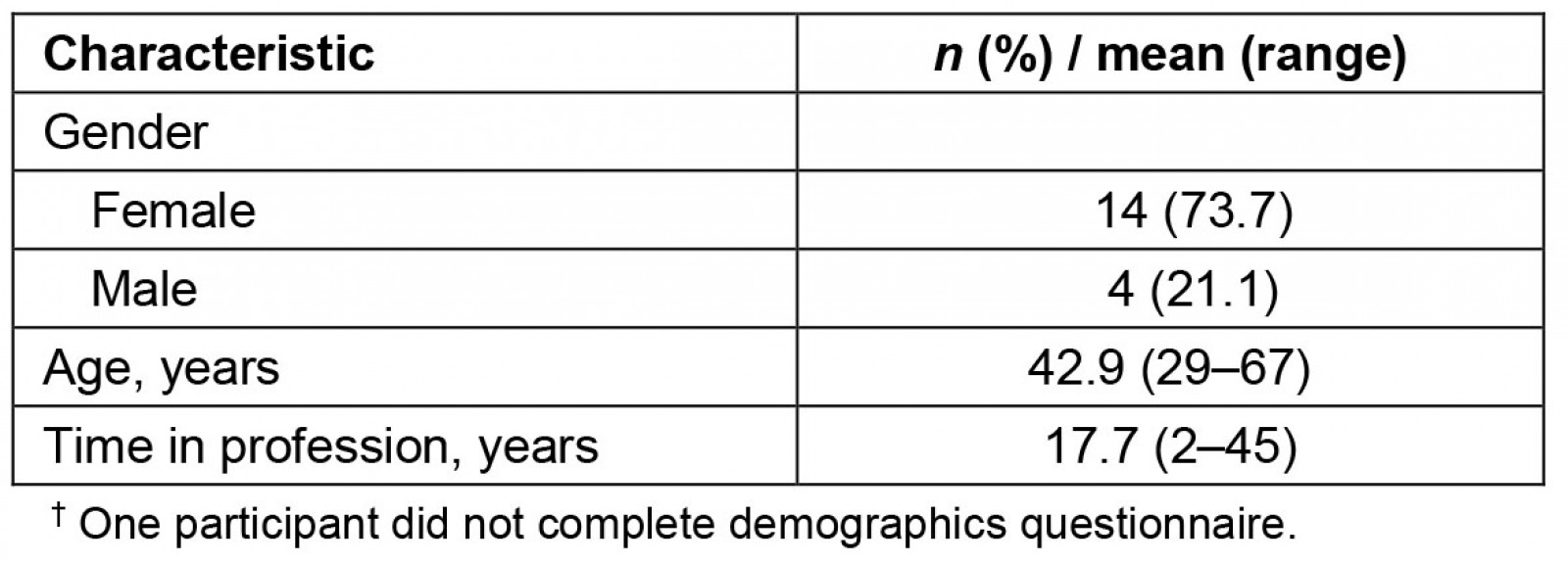
Theme 1. Understanding the study and translation context is vital to enacting change
An understanding of the original research (ie study) context was identified as a key step to determining whether and how to translate relevant research into practice. As this participant explained, an understanding of the organisational context of the study was considered fundamental to determining the implementation approach for the local setting, or indeed, whether the research should be translated:
[Metropolitan university health service] were running a study into whether medical and surgical physios were of use over the weekend, whether it was increased rates of discharge on the weekend would affect the length of stay. I think the results actually indicated that in some circumstances they increased length of stay … But unless you’ve been working at [metropolitan university health service] you don’t really know how their physio structure is, what the nurses normally do with the patients on the ward … Access to rehab might be much slower than – there are so many other contextual things that you then have to decide whether that’s something you’d want to go ahead with, looking at it in our local environment. Because it is such a large systems change. (Emerging researcher 2)
Therefore, there is a need for emerging researchers to have the skills to evaluate both research evidence and clinical context to then translate that knowledge into local practice accordingly:
… it’s about being able to extrapolate what you read in the paper and the types of people that are included for as much of a homogenous trial as you can create and translating that to what you can actually do with people in a more sustainable environment without research funding. (Emerging researcher 2)
The participant quoted below took this further by describing in more detail the skills and insights needed for emerging researchers to tailor the research evidence to the local health context and implement it using context-appropriate strategies:
There’s the translation skill in being able to pull some research that makes sense to an environment and actually being the messenger. So, being able to pull something from a paper or from the evidence and being able to make sense to a workplace, and there’s real skill in that … something has worked in the UK that’s had this amazing effect, well what’s it going to look like for my health service here in [location] or here in [location] and what do we need to do differently for our – how are we going to make this translate the way we want it to and that’s translation and there’s some real skill in that operationalising of that. (Manager 3)
There are multiple factors emerging researchers grapple with when considering the uptake and translation of research into practice in their context:
With timing [of research], I see people around me worry a little bit about being on either end of the spectrum of translating research. You don’t necessarily want to be the cowboy who’s adopting something new and barely tested – on one single study and changing the whole way you practice on the basis of that. But at the same time, you don’t want to be a laggard in a world of research where we know it already takes a long time to get studies published from when they’re actually done. Then people have to find them, interpret them, then figure out how to make system changes around them. (Emerging researcher 3)
The translation context is multifaceted and encompasses the research study environment, translation context, and timing-related factors. Building skills and capability in analysing and understanding these factors is crucial for emerging researchers to enact evidence-informed practice change.
Theme 2. Engaging with stakeholders identifies research and translation priorities and suitable approaches
To enable the rapid translation of research into practice, emerging researchers need to engage with a range of stakeholders to identify research and translation priorities with which to align their efforts. Health managers were identified as a key stakeholder group, ideally positioned to identify and communicate research and translation priorities at both the organisational and team level:
We always have research communication coming from the researchers, going up to the managers. I think we also need communication in both ways. So, the managers should be able to make a research plan that can be communicated or discussed with their teams so that – I think that would be very useful for translating whatever comes out of the research into actual practice because the chain has already been developed. (Mentor 1)
Engagement with managers is perceived to be ideal even before research ideas are developed into projects, to ensure alignment with local priorities and plans, which probably reflect organisational priorities. The notion of ‘organisationally endorsed’ research ideas was described:
I would also be interested in people coming into it [research activity] with a more like organisationally endorsed research question in mind … I worry that perhaps people would come in with their own agenda or project and it will be hard to get off the ground if it’s not in line with the direction of the organisation to begin with. (Emerging researcher 3)
Research translation was also considered a reciprocal ‘capacity-building process’, highlighting the importance of engagement and shared learning between researchers and end users (community members, patients, health professionals and health service managers) throughout research and translation processes:
It’s also a capacity-building process to allow people to actually have the skills to implement it, so it’s a two-way process. The end users may not fully understand the research methodology and the process, and the researchers may not fully understand the limitations that the end users have. So, I think it’s about a conversation between [end users and researchers]. (Mentor 5)
Emerging researchers may also be end users and are ideally placed to broker between other end users (ie their colleagues) as well as members of the research team to facilitate this two-way capability-building process.
Translating research into practice invariably requires changes to procedures and processes, which may not be achieved without intentional effort to ameliorate resistance to change by bringing clinicians on the journey:
It’s also that change management, so it’s bringing clinicians onboard because sometimes the research [evidence] challenges clinicians to work differently to what they’ve previously done. (Manager 2)
Opportunities for community-level stakeholder engagement are enhanced in rural areas, and there is recognition of the potential benefits of engaging with rural communities to champion locally led health research endeavours:
If you can go out into the community and say ‘I’m doing this, and I’d like your ideas’ maybe they can put pressure on the health service or help you with funding … I think people are always – particularly in country areas – thinking they are a bit neglected and here’s someone who cares about making my health better. (Mentor 5)
When engaged throughout the process, community members can play a key role in influencing the research agenda in rural health organisations and potentially supporting research endeavours through funding and other mechanisms. Participants also identified the need for priorities common to health organisations across the region to be established and actioned, to improve the impact of research and successful translation:
[Organisation] is going to do this and someone else is going to do this, rather than having all this duplication and replication … maybe it’s sharing it across the region and saying, these are six different things that we want to look at, and either everybody’s collaborating on the one thing or you’re dividing it up and saying, you look at this and I’ll look at that. (Mentor 3)
Overall, it was noted that setting priorities for research translation must consider the needs of multiple stakeholder groups: organisations, health managers and knowledge users, including clinicians and consumers.
Theme 3. Mentor and managerial support assists navigation of research translation activities
Guidance from and informal discussions with research mentors were considered important:
Having people on hand that are easy to talk to about those things would be really helpful … Accessing or having someone to chat to about things where you don’t need to provide papers of documentation beforehand and get them to be an author on your work – just have access to them just to ask simple questions. It’s kind of hard to look up on the internet when you don’t really know what you’re talking about. It’s hard to look up the words to even get started. (Emerging researcher 2)
Support and guidance were regarded as essential and considered important very early in the research translation process. Manager support was identified as critical for health professionals to progress ideas and enact change:
They need to be good leaders and listen to their staff. If you bring something up in your performance development review, ‘well okay let’s have another meeting to discuss that. How could we make that happen? How can I support you to do that? What do you need from me?’ Rather than ‘yep, righto that’s your performance development review done, move onto next year’, it’s actually – it’s a real leader. It’s somebody that says that’s a great idea, have you thought about developing that further. So that as a leader – yeah, a manager should be a leader in all areas including research. (Emerging researcher 7)
Managers need not be experts in research but are ideally placed to foster or, where required, reframe their team members’ enthusiasm and interest in pursuing research translation endeavours. As one participant explained, research translation can be conceptualised as a culture of collaborative learning and idea formation. By fostering this culture during clinical work time, managers can help to bring research and translation into everyday practice:
… research is not a singular thing. It’s coming up with ideas, your own ideas, sharing them with others, collaborating with others, sharing information, publications, digesting the research yourself, sharing it with your team, helping less experienced or less confident people to even be brave enough to think about an idea, creating an environment where research is encouraged where we can enable staff to have time to sit and think about research, to read research, so they’re not always being dragged away to clinical duties 8 hours every shift. All of those things are just aspects of real-world translating research into everyday practice to me. (Manager 1)
The process of engaging stakeholders in research translation can be overwhelming for emerging researchers, and the need for guidance was evident:
… a mentor that can help you navigate the various places you need to intercept. It’s quite nuanced and I’m thinking about even an ethics application process can be very overwhelming – well slightly off-putting really – for someone who hasn’t had a lot of experience in that space. So, it’s navigating a lot of different worlds as well and even knowing your own organisation sometimes and being connected to the right people to help with those resource development things. (Manager 3)
Similarly, an emerging researcher highlighted: ‘it’s really complex … you don’t know what you don’t know until you need it’ (Emerging researcher 9). Different sources and types of mentoring and support are central to support emerging researchers engage in research and translation.
Theme 4. Access to clinical and research networks promotes research translation partnerships and collaborations
Participants identified the need for clinical and research networks to facilitate more rigorous research activity, and promote collaboration and clearer pathways for emerging researchers:
If we could have some kind of structure so that the collaboration goes across the region, where everybody knows what everybody’s doing. If there was a career pathway or research journey that was well articulated … that’s blue-sky horizon for me … People could see that if [it is] a clinician’s passion and interest area and [they] knew who to go to for different types of support and there was a supervision model or something structured, and you could navigate that structure, it would be fantastic. (Manager 3)
Emerging researchers who struggled to progress their research ideas benefited from connecting with likeminded experienced researchers, networks and potential partners:
We had this idea for 5 years before we could get it off the ground … It really wasn’t until we met the right people that we could start to see this come to life. There just seemed to be a lot of barriers in our way but when we met [Researcher A] – and [Researcher B] … it just seemed to get some legs. It created some networking opportunities and links for us, which I think adds strength within our organisation. So, I guess that’s another thing to foster is those links within your own organisation and externally; the right people to partner with. (Emerging researcher 6)
Similarly, a mentor described the benefits of knowing others in the local region are available to support emerging researchers:
… if you have a good network of communication and I think it’s knowing where the support is and since those translation roles have been in place, I might not have all the answers and people might not even come directly to me but I might be able to say, if you’re allied health then there’s good support through [Researcher C] and [Researcher D], if you’re not allied health then potentially, we could channel this to someone like [Researcher E] or [Researcher F]. So, it’s knowing who and what’s available. (Mentor 3)
Collaborations and networks were considered crucial for smaller rural towns where workforce shortages and pressures are more pronounced. Participants described a key feature of a research and translation capable region as:
… linkages between all of the major partners across the region, universities and health services partnerships and collaborations. It is a very different picture, rural research. I worked in [rural town] for a time, and it was very different to working in [regional town] or [regional town]. Interesting even when the support was there at a managerial level, there was just not staff to fill places. So, staff really couldn’t take time off for research even if they had the money because they couldn’t get anyone in to replace them. (Mentor 4)
Although funding and managerial support for research are fundamental to support research activity, smaller rural services also need networks and human resources to support and progress research and translation endeavours.
Discussion
This is the first study of the individual-level capability-building needs of rural health researchers to promote the translation of research into practice, from multiple stakeholder perspectives. Of the many definitions of research translation14,18, the current findings reflect a common conceptualisation: research that is grounded in health practice and the activities required to tailor and implement research evidence in the local context11,14,40. The support required and areas for rural and regional capability building identified in the current study relate to these two research translation concepts.
On tailoring and implementing research into practice, health professionals are called on to critically analyse the study characteristics and context and the features of the local (implementation) context18. There are numerous strategies and mechanisms described in the implementation science and health services research literature to support this work, including academic partnerships, developing implementation blueprints18, integrated knowledge translation11, and knowledge brokerage2. Hitch and colleagues40 developed a practical framework to guide knowledge translation in allied health settings specifically; however, empirical evidence to demonstrate its utility in practice is currently in development. Another proposed mechanism to build research translation capability is through more actionable dissemination of health research evidence to reduce barriers associated with interpreting research papers, and to make clear the actions required of clinicians for implementation41. This study confirms the need to support place-based, contextually relevant research to promote translation.
The research impact and research capacity-building literature emphasise research priority setting as pivotal to ensuring the relevance and potential benefits of health research on policy, practice and health outcomes8,42-44. Processes and models for engaging and setting priorities with the range of stakeholders that have interest in health research have been documented45. Our research highlights the need to build health professional-researcher capability to identify and engage with the range of stakeholders who are integral to successful research translation: end users (eg other health professionals, support staff, healthcare consumers, community groups), health managers, and other key decision-makers within organisations. Although focused on individual capability building, this study also points to the need for organisational capability development to enable the identification and communication of strategic and research priorities20, and, moreover, to identify research priorities common to health services and communities within the local region that can be addressed collaboratively46.
Hitch et al40 define social capital as the resources afforded by the research translation team and its networks, and brings the need for collaborative approaches to research translation to the fore. Under their definition, social capital includes leadership, social network composition, and the range of skills held by the research translation team and its extended social networks. The delivery of health care in rural settings centres on the relationships between healthcare providers and those accessing services47. Emerging researchers in rural health settings are therefore at an advantage in terms of their established relationships and networks within the health and community setting48. This provides social capital, which could be leveraged through timely and appropriate community engagement and partnerships with consumer groups to bolster their health research translation endeavours.
To reduce duplication and strengthen research efforts, emerging researchers require knowledge of and access to clinical and research networks to link into44,46. Collaborative research is particularly important in rural and regional settings, where health practice problems are often disparate from metropolitan settings and where financial and other supports for research are comparatively less5,6,44. These findings resonate with those of Schmidt et al44 of the need for collectivity and collaboration to support rural health research, particularly partnerships between academic institutions and health services. These findings also resonate with the outcomes of a population health research practice partnership and embedded researcher model described by Wolfenden et al4.
The current study also identified the need for timely mentoring and support to guide emerging researchers through the nuanced and complex research and translation processes. Research mentoring is commonly described as a mechanism whereby experienced researchers support and steer emerging researchers through the research process and milestones49 and is recognised as an important feature of research and translation training programs24,50-52. This research highlights that in addition to the conventional form of research coaching, managers and leaders can play an essential role by offering encouragement, mentoring and strategic support. These findings align with existing evidence that elucidates the important role managers and leaders play in supporting evidence-based practice and innovation53,54. Current findings suggest that although managers may not have research experience, they have the decision-making ability and influence that is critical to enabling research and its translation1,54. Urquhart and colleagues55 found the key factors influencing managers’ commitment to and support for the implementation of innovative practices in cancer care were the ease of implementation and the perceived benefits to patients. This study highlights the need to develop a different skillset in managers to equip them to identify and communicate research translation priorities, recognise the features of the research translation climate within their setting or team, and reconcile the priorities of multiple stakeholder groups to facilitate change54. Managers also play a critical role in nurturing their team members’ enthusiasm for research and in identifying and promoting important ideas and questions27. When managers and their staff are aligned in their commitments to translating research into practice, they can form effective and influential dyads56. Nonetheless, it is recognised that first-level managers are constrained by the same organisation-level barriers to research translation as their team members, such as inadequate senior manager support for research and translation, limited resources, and time constraints1,57,58.
Strengths and limitations
The study was set in two large rural and regional areas in Australia, with participants from several organisations. Nonetheless, the findings may not be transferable to other rural and regional settings with different levels of research activity and infrastructure. The study involved three important research translation groups (emerging health professional researchers, health managers and mentors); however, it did not consider the perspectives of healthcare consumers, health service executives, research funders, non-government organisations and policymakers. These perspectives may be useful for future broader explorations of research translation capability-building strategies. Although the sample consisted of participants representing different stakeholder groups, levels of experience in their roles, two genders and a range of ages, the sample size (n=19) may limit the transferability of findings to the population of interest.
Implications for practice
These findings highlight the need for a region-wide approach to building research translation capability. Although emerging researchers need support and training to develop various research translation skills, they also require managers and mentors who are adequately equipped to aid their identification and progression of translation-focused research. Research translation capability-building programs, therefore, must be multi-dimensional and address the needs of numerous groups playing a role in research translation. In a bid to maximise the impact of emerging researcher-led endeavours, organisations need to identify and communicate their priorities, and, ideally, shared priorities across the region should be established. Implementing systematic approaches for collaborative rural health research priority setting is crucial and rural health researchers may be at an advantage with respect to access to their communities for research priority identification and engagement.
Conclusion
This study identified numerous individual-level emerging researcher skills and supports that are required to see the conduct of more translation-focused research, and the translation of research into practice in rural health settings. Emerging researchers need to develop multiple types of research translation skills through different approaches and levels of influence. They need support and guidance to ensure their endeavours align with and leverage organisational and regional priorities for research translation. These findings can inform existing approaches to research capability building through training and resource provision, and organisation-level infrastructure development and capacity-building initiatives to support the rapid translation of research into clinical practice.
Acknowledgements
The authors acknowledge and thank the focus group participants for generously sharing their insights and for the health organisation managers who supported their participation.
Funding
The authors acknowledge and thank Western Alliance for their financial and in-kind support for this research.
Conflicts of interest
The authors declare they have no conflicts of interest.
References
You might also be interested in:
2011 - Earthquake, tsunami, radiation leak, and crisis in rural health in Japan


